To evaluate the economic impact of a telemedicine procedure designed to improve the quality of lung function testing (LFT) in primary care in a public healthcare system, compared with the standard method.
Materials and MethodsThe economic impact of 9039 LFTs performed in 51 health centers (2010–2013) using telespirometry (TS) compared to standard spirometry (SS) was studied.
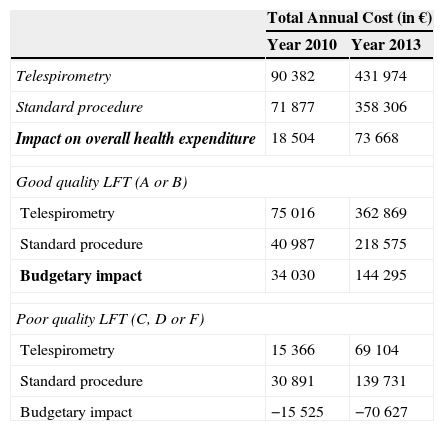
ResultsTS costs more per unit than SS (€47.80 vs €39.70) (2013), but the quality of the TS procedure is superior (84% good quality, compared to 61% using the standard procedure). Total cost of TS was €431974 (compared with €358306 for SS), generating an economic impact of €73668 (2013). The increase in cost for good quality LFT performed using TS was €34030 (2010) and €144295 (2013), while the costs of poor quality tests fell by €15525 (2010) and 70627€ (2013).
ConclusionThe cost-effectiveness analysis concludes that TS is 23% more expensive and 46% more effective. Healthcare costs consequently fall as the number of LFTs performed by TS rises. Avoiding poor quality, invalid LFTs generates savings that compensate for the increased costs of performing LFTs with TS, making it a cost-effective method.
Evaluar el impacto económico de un sistema de telemedicina en un sistema público de salud para la mejora de la calidad de las espirometrías (espirometrías forzadas [EF]) en atención primaria.
Material y métodosSe ha evaluado el impacto económico de 9.039 EF realizadas en 51 centros de salud (2010-2013) mediante teleespirometría (TE) comparándose con el sistema habitual.
ResultadosEl sistema de TE encarece el coste unitario de la EF (47,8€ vs 39,7€) (2013), pero logra una mejora en la calidad de las mismas (un 84% con buena calidad, frente a un 61% mediante el procedimiento habitual). El coste total de la TE ha sido de 431.974€ (358.306€ por sistema habitual), lo que supone un impacto económico de 73.668€ (2013). El aumento de gasto para EF de buena calidad realizadas con TE fue de 34.030€ (2010) y de 144.295€ (2013), mientras que para las pruebas con mala calidad fue de −15.525€ (2010) y de −70.627€ (2013).
ConclusiónDel análisis coste-efectividad se concluye que la TE es un 23% más costosa y un 46% más efectiva. Asimismo, el gasto sanitario es menor a medida que el número de EF realizadas mediante TE aumenta. La no realización de EF de mala calidad, no válidas, supone un ahorro que compensa el aumento del gasto por la realización mediante TE, siendo un sistema coste-efectivo.
Lung function testing (LFT) is a first-line procedure for diagnosing patients with respiratory symptoms.1–3 Its success depends largely on the skills of the technician performing it, and some quality control issues have been detected since it was introduced into the primary care setting.4–7 Several studies have confirmed that the quality of LFTs performed in the primary care setting can be less than desirable, underlining the importance of ongoing training programs for technicians, if reliable results are to be obtained.8–15 Recently published strategies recommend the use of remote monitoring for ensuring LFT quality in various settings.16,17 Burgos et al.18 showed how these telemedicine systems could be applied in primary care. Their results were subsequently confirmed in a study which used the same computer application in greater numbers of spirometries analyzed over longer periods of time.19
The main aim of this study was to perform an economic analysis to estimate the cost of introducing a telemedicine procedure for LFT quality assurance in the primary care sector of a public health system. Our secondary objective was to use a cost-effectiveness analysis to justify the generalized use of this initiative as a quality control system in this healthcare setting.
Materials and MethodsOur group participated in the development of a computerized telemedicine tool for monitoring spirometries (e-Spiro, Linkare: Tecnología Sanitaria, S.L).19,20 Nurses performing LFTs in health centers log on to this online computer system, known as telespirometry. They submit their LFTs to a central laboratory and receive an evaluation of the quality of these tests.
In an initial 9-month phase, we evaluated the effectiveness of the telespirometry application for improving spirometry quality and the costs of these activities in the primary care health centers of the Basque Health Service located in Ezkerraldea-Enkarterri, Uribe and Bilbao (northern Spain). The reference values of the Lung Function Laboratory of the Hospital Universitario Cruces (Barakaldo, Spain) were used for evaluating LFT quality.
The economic analysis was performed according to the tariffs of the funding agency of the Basque Health Service. A cost-effectiveness analysis was performed, comparing the telespirometry procedure with the standard procedure.
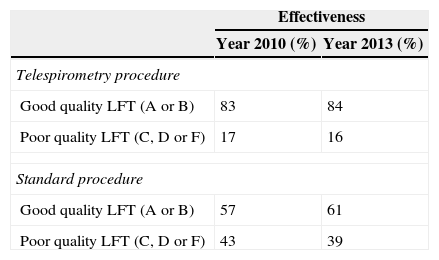
Effectiveness was determined from data obtained during a 9-month, controlled, longitudinal, multicenter study, performed in the Respiratory Medicine Department of the Hospital Universitario Cruces and 15 primary care centers20 (Table 1). Quality was graded according to the criteria of the European Respiratory Society-American Thoracic Society.12,13,19 Effectiveness was calculated from the percentage of Grade A and B LFTs performed in each center at the start of the study.
Effectiveness of Study Procedures, Years 2010 and 2013.
| Effectiveness | ||
|---|---|---|
| Year 2010 (%) | Year 2013 (%) | |
| Telespirometry procedure | ||
| Good quality LFT (A or B) | 83 | 84 |
| Poor quality LFT (C, D or F) | 17 | 16 |
| Standard procedure | ||
| Good quality LFT (A or B) | 57 | 61 |
| Poor quality LFT (C, D or F) | 43 | 39 |
LFT, lung function test.
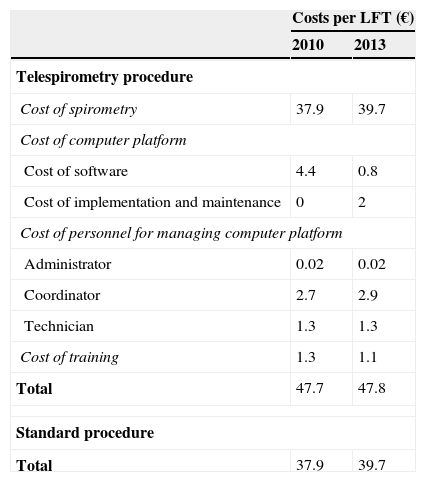
We calculated the specific direct costs of procedures, human resources and training costs for the telespirometry procedure. To this, we added the costs of the platform software (Table 2). Human resources costs (a pulmonologist and a nurse) for both training and managing and operating the system were calculated on the basis of LFT costs for 2010 and 2011, retrieved from the tariffs of the Basque Health Service lists for health and teaching services for those years (Table 2).
Comparison of Lung Function Test Costs, in 2010 and 2013.
| Costs per LFT (€) | ||
|---|---|---|
| 2010 | 2013 | |
| Telespirometry procedure | ||
| Cost of spirometry | 37.9 | 39.7 |
| Cost of computer platform | ||
| Cost of software | 4.4 | 0.8 |
| Cost of implementation and maintenance | 0 | 2 |
| Cost of personnel for managing computer platform | ||
| Administrator | 0.02 | 0.02 |
| Coordinator | 2.7 | 2.9 |
| Technician | 1.3 | 1.3 |
| Cost of training | 1.3 | 1.1 |
| Total | 47.7 | 47.8 |
| Standard procedure | ||
| Total | 37.9 | 39.7 |
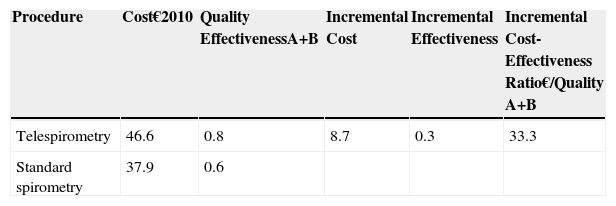
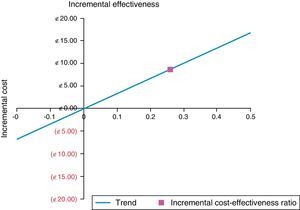
The equivalent annual cost of the computer platform was calculated on the assumption that its useful lifespan was 5 years and its residual value was zero. The rate of discount applicable in the calculation of the equivalent annual cost was 3%.21,22 The cost and incremental effectiveness of both procedures was also determined and the incremental cost-effectiveness ratio was deduced (Table 3).
Incremental Cost-effectiveness Ratio per Spirometry Performed Using the 2 Study Procedures.
| Procedure | Cost€2010 | Quality EffectivenessA+B | Incremental Cost | Incremental Effectiveness | Incremental Cost-Effectiveness Ratio€/Quality A+B |
|---|---|---|---|---|---|
| Telespirometry | 46.6 | 0.8 | 8.7 | 0.3 | 33.3 |
| Standard spirometry | 37.9 | 0.6 |
The data obtained in this initial phase were used to evaluate the economic impact of incorporating telespirometry into the public health system. This constituted the second phase of the study, conducted over a 3-year period (2010–2013).
In this second phase, after the program was implemented in the public health system, we evaluated the overall costs of its progressive introduction compared to the traditional system. Data were analyzed in the centers that at the end of 2013 had performed LFT with telespirometry for a period of at least 9 months.
We based our analysis of the effectiveness of the telespirometry procedure for the period 2010–2013 on data obtained by Marina et al.19 For the standard procedure, we assumed for 2013 the same effectiveness as that recorded at the beginning of 2010.
The same amount of time dedicated to training and management of the platform was assigned for 2010 and 2013. Human resources costs (a pulmonologist and a nurse) in 2013 were calculated using figures from 2010 updated with the 5.6% official inflation rate between December 2010 and December 2013, according to National Labor Institute figures.
Finally, the direct cost of the test itself for the year 2013 was retrieved from the tariffs of the Basque Health Service lists for health and teaching services.
The total cost for both procedures was calculated from the total number LFTs performed and the mean cost of the technique. The impact of telespirometry on health expenditure between 2010 and 2013 was taken as the difference between the total annual cost of the telespirometry procedure and the cost of the standard procedure. The impact of telespirometry on health expenditure was also calculated according to the quality of the test.
ResultsA total of 1894 spirometries were performed in the 15 centers during the initial 9-month phase; 83% of the telespirometry procedures were good quality (A or B), compared to 57% of the standard procedures (Table 1). The cost of each LFT during the initial study phase was €46.60 at the beginning, and €47.70 at the end of 2010 if telespirometry was used, compared to €37.90 for the standard procedure (Table 2).
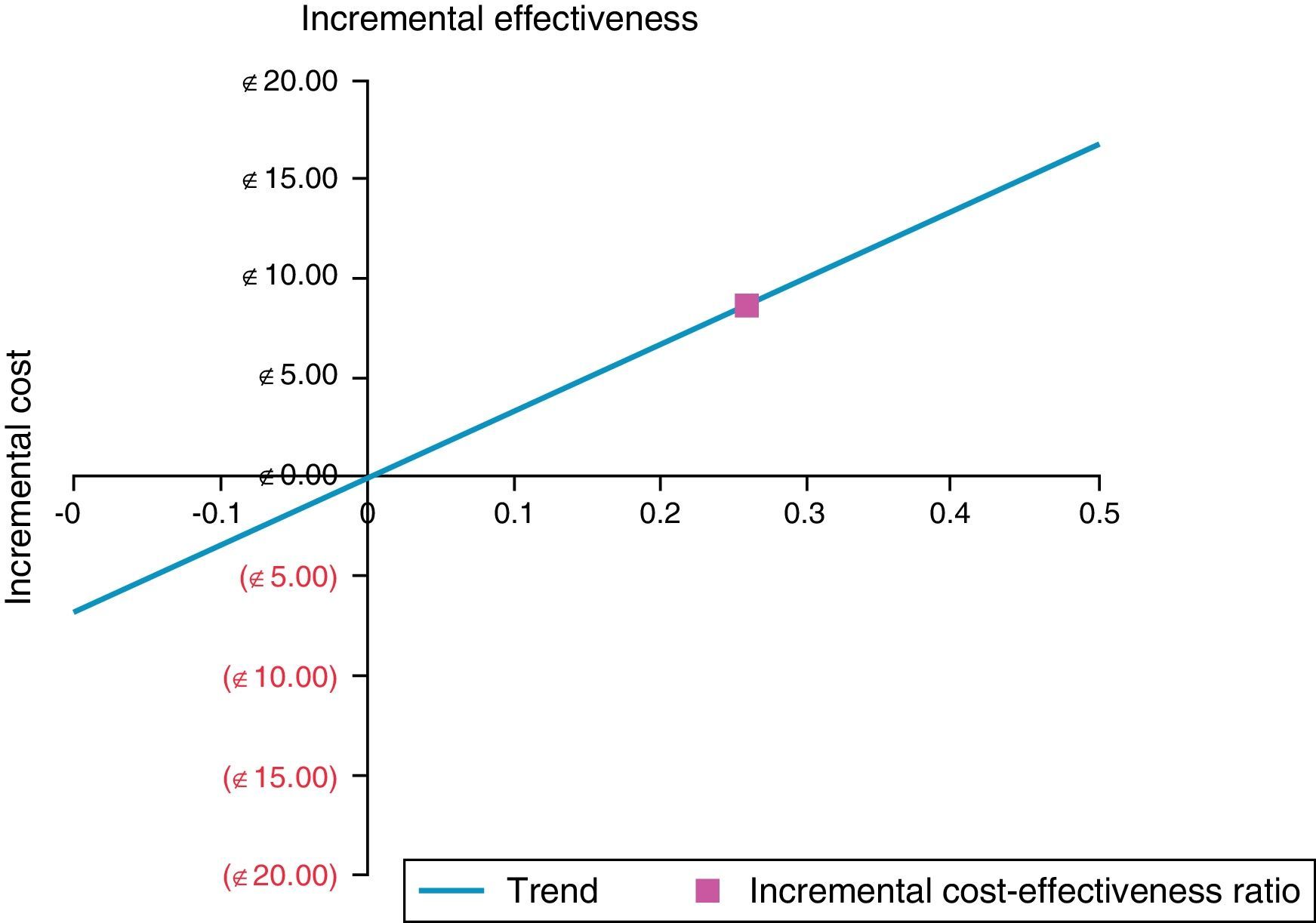
The incremental cost-effectiveness ratio for producing quality A or B spirometries was €33.30 (Table 3), calculated using the LFT unit price from the beginning of 2010. The cost-effectiveness diagram places the telespirometry procedure in the upper right quadrant, indicating higher cost and greater effectiveness (Fig. 1).
Implementation of the SystemAfter evaluating the costs per spirometry and the effectiveness of telespirometry, we examined the cost of introducing it into the public health system. The effectiveness of telespirometry was greater than 80% in both phases, compared to nearly 60% with the standard procedure (Table 3). Use of resources per spirometry was similar in the periods 2010 and 2013. A total of 1894 spirometries were performed in 2010 (initial phase) and 9039 between 2010 and 2013 (second phase) (Table 4).
Total Cost of all Spirometry Studies and Cost/quality Relation in 2010 and 2013.
| Total Annual Cost (in €) | ||
|---|---|---|
| Year 2010 | Year 2013 | |
| Telespirometry | 90382 | 431974 |
| Standard procedure | 71877 | 358306 |
| Impact on overall health expenditure | 18504 | 73668 |
| Good quality LFT (A or B) | ||
| Telespirometry | 75016 | 362869 |
| Standard procedure | 40987 | 218575 |
| Budgetary impact | 34030 | 144295 |
| Poor quality LFT (C, D or F) | ||
| Telespirometry | 15366 | 69104 |
| Standard procedure | 30891 | 139731 |
| Budgetary impact | −15525 | −70627 |
Cost per procedure using the telespirometry method was €47.70 (end of 2010) and €47.80 (end of 2013), compared with €37.90 (2010) and €39.70 (2013), respectively, for the standard method (Table 2). The cost of LFT using telespirometry was thus 20% more expensive in 2010 and 17% more expensive in 2013.
The total cost of telespirometries performed in 2010–2013 was the product of the number of spirometries performed (9039) multiplied by the cost of each spirometry (€47.70), giving a total cost of €431974, compared to €358306 if the spirometries were performed using the standard procedure. If we break down this data in terms of quality, we find that the total expenditure for poor quality LFTs with telespirometry is €69104 compared to €139731 with the standard procedure (Table 4).
Impact on Health ExpenditurePerforming LFTs with the telespirometry procedure, instead of the standard procedure, increased health spending by €18504 in 2010 and €73668 in 2013 (the difference between telespirometry costs and standard procedure costs) (Table 4).
If these figures are broken down by LFT quality grades, the impact on health expenditure was €34304 in 2010 and €144295 in 2013 for good quality LFTs (A or B). For poor quality LFTs (grades C, D or F), the impact was a saving of €15525 in 2010 and a saving of €70627 in 2013 (Table 4).
DiscussionOur study shows that the telespirometry system is cost-effective in a healthcare system, because, despite being more expensive than standard spirometry, it is much more effective and represents a better use of resources.
Before a new procedure can be introduced into a healthcare system, an economic analysis is necessary to assist in decision-making. By using a cost-effectiveness analysis, we can assess the costs of implementing a new program that has proven to be effective.
Our results show that the telespirometry procedure was more expensive than the standard method (incremental cost of €8.70 per test), but it was also more effective (incremental effectiveness of 0.3). A more effective telespirometry procedure increases the proportion of good quality LFTs, and reduces the proportion of poor quality LFTs. Reducing spending on poor quality procedures results in a better utilization of economic resources.
The good management of patients with respiratory diseases requires the provision of good quality spirometry in both primary care settings and specialized centers. Many authors have evaluated the quality of spirometries performed in different healthcare settings and the introduction of strategies aimed at improving standards. Hueto et al.6 studied the use of spirometry in primary care centers in Navarra (Spain). They found that 90.9% of health centers had a spirometer, but that in 22% the device had never been used. With regard to the quality of the procedures, 76% of tests failed to meet reproducibility criteria, and in 39.7% the functional diagnoses were incorrect.
Other groups23,24 found major differences in the performance of spirometries among different autonomous communities of Spain. The number of spirometries conducted per week ranged from 2 to 8.9 in primary care and from 34.3 to 98.3 in specialized centers. Spirometry quality criteria differed widely: the percentage of spirometries that met 6 or more quality criteria ranged from 9.1% to 84.6% in primary care and from 37.5% and 100% in specialized centers.
Various strategies have been used to improve the quality of spirometry in primary care. Marina et al.19 used a telespirometry system, and after analyzing 7200 procedures, achieved high quality spirometries (A or B) in 84% of procedures. Burgos et al.,18 using a similar telespirometry system, reported a slightly lower rate: of 4581 spirometries, 71.5% of the intervention group were quality A or B, compared to 59.5% of the control group.
Castillo et al.25 postulated that offering spirometries in pharmacies could be of use in identifying individuals at risk of chronic obstructive pulmonary disease. They enrolled 161 subjects in 13 pharmacies and obtained a rate of 70% of quality A or B spirometries. Masa et al.17 compared results from standard spirometries performed by an operator with 15 years’ experience, with those conducted using a teleconference system. The rate of good quality spirometries obtained with the conventional method was 87.7%, compared with 81.6% for the webcam spirometries.
Represas-Represas et al.15 performed an interventional study in 26 health centers in the region of Vigo (Spain) using measurements obtained before and after operators received tutored training. In the first month of tutoring, they correctly performed and interpreted 370 out of 521 spirometries (71%). In the second month, this proportion had risen to 562/619 (90.9%). Spirometry quality was assessed one year later in 62.5% of the trainees: of the 255 procedures evaluated, 211 (83%) were valid and correctly interpreted.
Most of these studies are based on a much smaller numbers of spirometries and centers than ours, limiting the application of their designs to other geographical settings. None of the previous publications evaluated the costs of the widespread implementation and use of these strategies in health systems.
The aim of our study was to evaluate the impact on healthcare expenditure of switching from a conventional LFT procedure to a telespirometry technique.
The cost analysis suggests that the telespirometry procedure is 23% more expensive, but it is 46% more effective than the standard procedure. These results show that as the number of LFTs performed using telespirometry increases, the health costs fall, since the savings made on poor quality LFTs compensate for the costs of good quality tests.
Our data indicate that the savings of avoiding poor quality LFTs that are invalid for diagnosis makes up for the increased costs of performing telespirometry LFTs, thus making the procedure cost-effective.
For this study, we had to quantify times and procedures on the basis of available data. We believe that we overestimated the assumed quality of the standard spirometries before the intervention, since we based our estimation on the activity of previously trained health professionals motivated enough to participate in the study.
This study focused on the direct costs of the systems used, as these are simpler to quantify. We did not consider more complex and variable indirect costs that could derive from the over or underdiagnosis of respiratory disease, inappropriate use of treatments, or the impact of poor quality spirometry on clinical practice and patients’ health. In any case, these health and economic costs, which would provide an even more favorable estimation than our calculation of direct costs, are yet another incentive for determining systems that might improve the performance of spirometries.
In our opinion, this study is an example of translational research: we conceived it as a research project on the efficacy of a telemedicine procedure,18 evaluated its implementation in a healthcare system,19 and developed it with the economic study which we present in this article. It is unusual to find health economic data in our publications, but this information is vital when presenting new technological tools to health authorities. Our economic data show that the implementation of this tool, with the help of pulmonologists, is feasible, cost-effective and useful for improving the performance of healthcare providers.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Marina N, Bayón JC, de Santa María EL, Gutiérrez A, Inchaustia M, Bustamante V, et al. Evaluación económica e impacto presupuestario de un procedimiento de telemedicina para el control de calidad de las espirometrías en atención primaria. Arch Bronconeumol. 2016;52:24–28.