Transbronchial needle aspiration (TBNA) of pulmonary lesions without endobronchial affectation in combination with transbronchial biopsy (TBB) has been shown to increase diagnostic perfortmance. The objective of this present study was to analyze whether the combination of TBNA with conventional TBB is a cost-effective approach.
MethodologyOurs is a prospective study that included patients with lung nodules or masses with no evidence of endobronchial lesions after flexible bronchoscopy in whom both TBNA and TBB were performed. We analyzed the additional diagnostic value, the impact of TBNA on the cost of the diagnosis and the minimum level of sensitivity required in order for TBNA combined with TBB to be considered a cost-effective diagnostic approach.
ResultsThirty-six patients were included in the study, 25 of whom were males. TBB reached a histologic diagnosis in 39% of the cases, and its combination with TBNA diagnosed 47%. The mean diameter of the lesions was significantly greater in the positive TBNA cases compared with the negative cases (31mm vs 23mm; P=.034). The cost analysis did not show the additional TBNA to be more cost-effective, despite demonstrating greater diagnostic sensitivity. The minimum sensitivity required for TBNA combined with TBB to be considered a cost-effective approach was 88%.
ConclusionThe contribution of TBNA to TBB in the diagnosis of lung nodules or masses without associated endobronchial lesions does not seem to justify the additional economic cost.
La punción aspiración transbronquial (PTB) de lesiones pulmonares sin afectación endobronquial en combinación con la biopsia transbronquial (BTB) ha demostrado incrementar la rentabilidad diagnóstica. El objetivo del presente estudio fue analizar si la combinación de la PTB con la BTB convencional es un abordaje coste-efectivo.
MetodologíaEstudio prospectivo en el que se incluyeron pacientes con nódulos o masas pulmonares sin evidencia de lesión endobronquial tras la realización de una broncoscopia flexible a los que se les realizó PTB y BTB. Se analizó el valor diagnóstico adicional, el impacto de la PTB en el coste del diagnóstico y el nivel mínimo de sensibilidad requerido para que la PTB combinada con la BTB pudiese ser considerada una aproximación diagnóstica coste-efectiva.
ResultadosSe incluyeron 36 pacientes (25 varones). La BTB obtuvo un diagnóstico histológico en el 39% de los casos y su combinación con la PTB en el 47%. El diámetro medio de las lesiones fue significativamente mayor en los casos con PTB positivos en comparación con los negativos (31 vs. 23mm; p=0,034). Tras la realización del análisis de costes la realización adicional de una PTB a pesar de demostrar una mayor sensibilidad diagnóstica no mostró una mayor eficiencia. El mínimo de sensibilidad requerido de la PTB combinada con la BTB para que pudiese ser considerada una aproximación coste-efectiva fue del 88%.
ConclusionLa contribución de la PTB a la BTB en el diagnóstico de masas o nódulos pulmonares sin lesión endobronquial asociada no parece justificar su coste económico adicional.
The diagnosis of peripheral lung lesions continues to be a frequent problem in standard clinical practice. New advances in bronchoscopic methods, such as the use of ultrafine bronchoscopes, endobronchial ultrasonography with mini probes and electromagnetic navigation, for the diagnosis of pulmonary lesions without observed endobronchial lesions seem to improve the diagnostic performance compared with classical techniques.1–9 However, said highly expensive technology is not available in many hospital centers. Thus, classic bronchoscopic techniques for the diagnosis of pulmonary lesions without endobronchial anomalies, such as transbronchial biopsies (TBB) and transbronchial needle aspiration (TBNA), are still important. Despite the fact that many studies have proven the diagnostic sensitivity of both techniques,6–19 there are few papers that have demonstrated their cost-effectiveness.20,21
The objectives of this present paper were to analyze whether the combination of TBNA followed by TBB could be a cost-effective approach in the diagnosis of lung lesions with no evidence of endobronchial lesion and to establish a theoretical calculation of the minimum level of diagnostic sensitivity of the combination of both to demonstrate their cost-effectiveness.
MethodologiesA prospective study was done including consecutive patients in whom bronchoscopy was indicated to diagnose well-defined peripheral lung lesions with no type of visible endoscopic lesion who underwent TBNA followed by TBB guided by fluoroscopy in a one-year period (November 2007–November 2008). Excluded from the study were those patients in whom lesions were observed in the tracheobronchial mucosa (visible tumor or infiltration) during bronchoscopy. All the procedures were done by the Bronchopleural Techniques Unit of the Pulmonology Department at Complexo Hospitalario in Vigo. The variables included in the study were demographic (age and sex) and radiological (size, location, presence/absence of the bronchus sign), as well as the final diagnostic result of the lesions that motivated the study, if they had been obtained. All the patients had had thoracic computed tomography (CT) (multislice, 16 rows) within the month prior to the exploration. The diameters of the lesions were determined by measuring the maximum anteroposterior and lateral diameters from the chest CT and calculating the mean of the two. The location of the lesions was defined by the lobe where they were situated and their distance to the pulmonary hilum. To do so, as in previous studies,8,14–16,19 we divided the area around the hilum on the CT into 3 elliptical regions: central (ellipse of the inner third), intermediate (ellipse of the middle third) and peripheral (ellipse of the outer third). When the lesion occupied more than one ellipse, it was assigned to the area that contained most of it. The lobe in which the lesion was located was determined by performing a detailed study of the available radiographies and chest CTs by 2 of the researchers. When the lesion affected more than 2 lobes, the one that contained most of it was chosen. The presence of the bronchus sign was defined in the same way.
For the procedures, several Olympus (Olympus, Tokyo, Japan) bronchoscope models were used. The bronchoscopies were done following standard procedure, with the patient being monitored, in supine decubitus and under conscious sedation (midazolam±fentanyl). The nasal pathway was mainly used, and for anesthesia 2% lidocaine was used. In all the cases, the tracheobronchial tree was completely inspected, after which the lesion was located with biplane fluoroscopy. Later, TBNA was carried out, followed by TBB. After locating the lesion with fluoroscopy, between 2 and 4 samples were taken by fine-needle aspiration. The type of needle used for the puncture was a Wang 22-gauge cytology needle (Bard-Wang, Billerica, MA, USA). The samples were considered “adequate” when there was abundant cellularity corresponding with the pulmonary parenchyma, neoplastic cells or another specific entity. The samples with atypias that were either doubtful or had no specific pathological diagnosis were classified as “undiagnosed”. The samples with neoplastic cytology or another specific diagnosis were considered “diagnosed”. In all the procedures, a cytopathologist was present for immediate microscope evaluation of part of the material obtained after hematoxylin–eosin staining. Later, the remainder of the cytological material was studied in the anatomic pathology laboratory after Papanicolau staining. After TBNA, TBB was performed by guiding the forceps to the lesion with fluoroscopy. A minimum of 4 biopsy samples was obtained per procedure. The TBB were done with oval fenestrated forceps (FB-21C-1, Olympus, Tokyo, Japan) with a length of 100cm and a diameter of 1.8mm. The material from the transbronchial biopsies was processed and later studied in the pathology laboratory. Both bronchial suction and brushing were carried out according to the criteria of the bronchoscopist, and the results were not included in the analysis.
For the purpose of this study, we theoretically assumed that if the bronchoscopy was not diagnostic, all patients would undergo CT-guided transthoracic fine-needle aspiration (FNA). We considered the diagnostic technique of reference to be that with which specific cytohistologic diagnosis could be obtained. It was assumed that in cases of negativity of the tests, a diagnostic protocol would be followed, which included more invasive procedures like surgery.
Cost AnalysisFor the cost-effectiveness analysis, we constructed 2 strategies and we compared the effectiveness and cost of each. In strategy I, both techniques (TBNA and TBB) were used, and in strategy II only TBB was done. The costs were calculated based on Decree 2009/2011 of the standard Costs and Fees of the Galician Healthcare Services. Specifically, within the cost of the pathologist, both the in situ cytological assessment and the later lab cytology analysis were included. The cost of the bronchoscopy included the cost of the procedure (250.45€). TBB was 595.46€ and TBNA included the cost of the needle for aspiration (80€), while cytology included the in situ assessment by the pathologist (253.69€). For the calculation of the transthoracic FNA cost, we included the cost of CT (366.32€), needle for aspiration (60€) and cytology, also including the in situ assessment by the pathologist (253.69€). The study was approved by the Research Ethics Committee of Galicia.
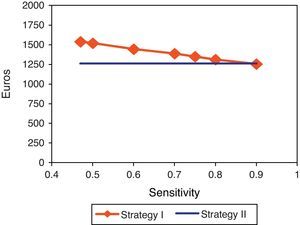
Statistical AnalysisThe qualitative variables were expressed as absolute frequencies and percentages, and the numerical variables as mean and standard deviation (SD). The comparison of the discrete variables was done with the chi-squared or Fisher's exact tests. The continuous variables were compared using the Student's t-test. P<.05 was considered statistically significant. The analyses were calculated with SPSS 15.0 software (SPSS, Chicago, IL, USA). The cost-effectiveness analysis was done using the diagnostic performance obtained and the costs for bronchoscopy, TBNA, TBB and CT-guided transthoracic FNA. We determined the minimum sensitivity that the combination of both techniques (TBNA and TBB) should have in order to equal the cost per patient of both strategies. To do so, we created a theoretical calculation model of the minimum sensitivity of strategy I in order for the cost per diagnosed case to be less than that of strategy II (Fig. 1). The calculation of the sample size was done by assuming a cost difference between using only TBB or using the 2 techniques (TBB and TBNA) of 300€ per patient, with a power of 80% and a confidence interval of 95% for an analysis of paired data.
Cost in euros per diagnosed case according to the sensitivity of the test. The theoretical model shows that, when the sensitivity of strategy I is modified (transbronchial needle aspiration and transbronchial biopsy), the cost per diagnosed case would be less than that of strategy II if its sensitivity were higher than 88%.
Thirty-six consecutive patients were included, most of whom were males (69.4%). The epidemiological characteristics, size and location of the lesion, as well as the presence of bronchus sign and the diagnoses by bronchoscopy, are shown in Table 1. The mean number of TBB was 4 per lesion (SD 2). TBB was diagnostic in 14 (39%) patients, and was the only test that provided diagnosis in 5 (14%) cases. TBNA was diagnostic in 11 (30.6%) cases and was the only procedure that provided a diagnosis in 3 (8.3%) patients. The mean number of passes per lesion was 2 (SD: 1.5). The combination of both TBB and TBNA bronchoscopic techniques provided diagnosis in 17 (47.2%) patients. In 19 patients, a specific bronchoscopic diagnosis was not obtained due to the presence of normal pulmonary parenchyma or insufficient material to make a pathological diagnosis. The only factor that was related with a greater percentage of positivity of the TBNA was the greater diameter of the lesion (31mm vs 23mm; P=.034). No differences were found in the performance influenced by the presence of bronchus sign, the location of the lesion or its benign or malignant etiology. In 6 cases, it was possible to perform TBNA due to the lack of progression of the needle through the apical segmental bronchi of the upper lobes, although they were considered within the final analysis as non-diagnostic. However, in said cases it was possible to perform TBB.
Patient Characteristics: Diameter, Location, and Diagnostic Bronchoscopies of the Nodules.
| Patients | |
| No. | 36 |
| Mean age, years (SD) | 65.6 (11.3) |
| Sex, males | 25 (69.4%) |
| Largest mean diameter, mm (SD) | 26.3 (10.6) |
| Largest diameter of the lesion<30mm | 24 (66.7%) |
| Bronchus sign | 10 (27.8%) |
| Location ULs | 21 (58.3%) |
| Location | |
| Medial | 9 (25%) |
| Central | 10 (27.8%) |
| Peripheral | 17 (47.2%) |
| Diagnostic bronchoscopy | 17 (47.2%) |
| Non-small cell carcinoma | 15/17 (88.2%) |
| Metastasis | 2/17 (11.7%) |
ULs, upper lobes.
The total cost of strategy I was 1538.48€ per patient diagnosed, and that of strategy II was 1261.45€ per patient diagnosed, with a cost difference of 277€ per patient (Table 2). Table 3 shows the sensitivity and the costs of the combination of both techniques (strategy I) and that of just TBB (strategy II). Strategy I, despite presenting greater sensitivity than strategy II, did not show greater effectiveness, so that both strategies had the same cost and, therefore, we could consider the combination of TBB and TBNA cost-effective, and the minimum sensitivity required of the combination of both was 88% (Fig. 1).
Sensitivity and Detailed Costs of the Procedures of Strategies I and II.
| Cost of the Procedure | Sensitivity | CT-guided Transthoracic FNA | Cost per patient diagnosed | |
| Strategy I:BronchoscopyWith TBBand TBNA | 250.45€ (bronchoscopy)595.46€ (TBB)253.69€ (cytology)80€ (cytology needle)No.=36 patients | 0.47 | 366.32€ (CT)253.69€ (cytology)60€ (needle)No.=19 patients | |
| 1179.60€ (totala) | 680.01€ (totala) | 1538.48€ (totalb) | ||
| Strategy II:BronchoscopyWith TBB | 250.45€ (bronchoscopy)595.46€ (TBB)No.=36 patients | 0.39 | 366.32€ (CT)253.69€ (cytology)60€ (needle)No.=22 patients | |
| 845.91€ (totala) | 680.01€ (totala) | 1261.45€ (totalb) | ||
FNA, fine-needle aspiration; TBB: transbronchial biopsy; TBNA: transbronchial needle aspiration.
The data obtained in our study confirm that the combination of TBB and TBNA for peripheral lung lesions involves a non-significant increase in the diagnostic sensitivity of the procedure (47.2% vs 39%). Nevertheless, in this series in particular the modest increase observed in sensitivity is not sufficient to be able to consider the contribution of TBNA to TBB cost-effective. According to different published series, the diagnostic performance of TBNA in peripheral lung lesions ranges between 40% and 80%, giving rise to an increase in the diagnostic sensitivity when combined with TBB between 5% and 30%.6–11
The variability of the reported data may be due to the fact that the diagnostic exactness of both techniques may be influenced by the size, location, presence of bronchus sign and diagnosis of malignancy. In this paper, all these variables were not associated with diagnostic performance, except for the size of the lesions, this being the only factor that was significantly associated with greater TBNA performance. In our study, we have found a diagnostic sensitivity of both techniques slightly less than that reported by other authors, which could be explained by the small mean size of the lesions (mean: 26.3mm). One of the reasons that may explain the importance of the size of the lesions could be that the larger ones are better viewed with fluoroscopy, although it is also possible that these may be accessed by more bronchi, regardless of whether these are seen on CT or not.
The lesion location has been defined in the literature as a determinant factor of the diagnostic performance of bronchoscopy, although in our study neither the lobe where it was located nor its location in the axial axis predicted the result. Chechani8 demonstrated, in a series of patients with lung masses or nodules without endobronchial lesion, that the diagnostic performance of the bronchoscopy was lower in the lesions located in basal segments of the lower lobes and apical segments of the upper lobes (58%) vs lesions located in the remaining segments (83%) (P=.03). However, Baaklini et al.12 did not find differences when comparing the lesions located in these segments, although they did observe better performance of TBB in lesions that were located in the middle lobe (83%) and lingula (67%). One possible explanation of this effect could be the greater difficulty for reaching the apical bronchi, which is aggravated even more so in the case of the cytological needle due to its consistency. In our series, we did not encounter this difficulty in any TBB procedure, but it was impossible to perform needle aspiration in 6 patients. Said procedures were considered non-diagnostic, but they were included in the costs of the final analysis.
The presence of the bronchus sign did not influence the performance of the bronchoscopy. In 1967, Tsuboi et al.15 classified the anatomical relationship of the bronchi with lung lesions. The lesions classified as I (the bronchus leads to and ends at the lesion) or II (the bronchus crosses it) were those in which the performance of TBB was greater. Later, Naidichi et al.16 defined this radiological sign, and in numerous studies it was related with a greater sensitivity of the endoscopic techniques in the diagnosis of this type of lesions.17–19 However, said factor did not influence the diagnostic performance of the bronchoscopy, which could be explained by its limited presence in only 27% of the lesions. Another factor that could influence the results is the needle model, but in our study, since the same type was always used, it would have no possible influence on the results. Nevertheless, it could justify the differences found with other studies in which the needle models used were different.
The diagnostic sensitivity of the new bronchoscopic techniques that have been developed in recent years, such as electromagnetic navigation and ultrasound bronchoscopy with radial mini probe, has led to an increase in diagnostic performance that is nearly 90%, according to preliminary studies.1–5 The main disadvantage of said techniques is that the technology is expensive and requires a high level of qualification and training, and they are therefore not accessible to many hospital centers.
Although it has been reported that the combination of TBB with TBNA and other accessory techniques (such as bronchial suction, lavage and brushing) may significantly improve results,7,8,12,22,23 it seems important to define the most cost-effective combination to obtain results according to the characteristics of the lesion and the clinical situation of the patient. In addition, despite the fact that there are many papers that evaluate the diagnostic performance of the techniques, there are few studies that evaluate their cost-effectiveness, which would enable the best diagnostic strategy to be defined based on cost.20,21 Therefore, despite the study being based on basic techniques, when we take into account their extensive availability in hospital centers, the current economic situation and the lack of related studies, our research is original and timely.
Nonetheless, there are some limitations that merit comment. First of all, the series is from a single center, which presents limitations when trying to extrapolate the results. However, the calculation of the sample size demonstrates that it is sufficient for the cost-effectiveness analysis. Another aspect that could limit the interpretation of the results is that the immediate assessment by the pathologist of the TBNA could obviate the need for TBB (assuming it was diagnostic) and therefore affect the costs. This aspect has not been analyzed in this paper, as we did not take into account the percentage of diagnostic in situ TBNA samples. For the analysis, the cost of complications was obviated because their frequency was similar in both strategies given that we did not have complications derived from the TBNA. In this study, we have not analyzed the cost of transthoracic FNA complications (fundamentally pneumothorax) with a frequency that can reach 30%. In our experience, as most transthoracic FNA procedures are done in an outpatient setting, the percentage of cases requiring hospitalization and drainage is very low (<5%), and the cost of said complication is that of 2 X-rays, 8 and 24h after the puncture. Thus, in our experience and in our setting, the expense of said complication is unlikely to compensate the additional expense of the TBNA needle.
In our study, the excessive cost of the TBNA, compared with its modest increase in diagnostic sensitivity, does not justify it being done routinely in combination with conventional TBB.
In spite of these 2 strategies being theoretical models created in order to compare costs, both are based on the standard diagnostic circuit used in most patients with this type of lesions in our hospital center. Given the data, we can assume that TBNA would be cost-effective if its diagnostic sensitivity reached 88%. It is a theoretical model, and if we modified the sensitivity of strategy I, the cost per diagnosed case would be less than that of strategy II if its sensitivity were higher than 88%. In this situation, only 4 of the 36 patients would have required CT-guided transthoracic FNA and, therefore, the cost per patient of both strategies would be the same.
ConclusionAccording to our analysis in this population in particular, the additional diagnostic value of the combination of TBNA with conventional TBB for the diagnosis of lung lesions without endobronchial alterations would not justify its additional cost.
Conflict of InterestsThe authors declare having no conflict of interests.
Please cite this article as: Leiro Fernández V, et al. Análisis coste-efectivo de la punción aspiración transbronquial de lesiones pulmonares sin afectación endobronquial. Arch Bronconeumol. 2012;48:448–52.