Bronchial artery aneurysm (BAA), corresponding to a vascular caliber greater than 2mm,1 has been reported in only 50 cases in the literature to date. Mizuguchi et al.2 mention that only 12 BAA ruptures were described in England before 2009. The ideal approach in this situation remains controversial. A minimally invasive endovascular embolization technique showed greater efficacy and safety than thoracotomy3,4 but with a conservative approach, clinical stability of the patient can be maintained without increasing operative morbidity.
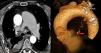
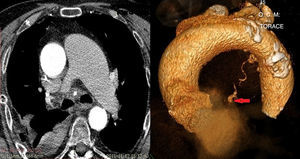
We present the case of a 75 year-old man admitted to the emergency department of our hospital with dyspnea, a single episode of hemoptysis and sudden pain in the right hemithorax. The patient had diabetes, hypertension, COPD and reported triple coronary by-pass in 2009. The chest X-ray showed right pleural effusion and the origin of the bleeding was determined with thoracentesis. The patient was hemodynamically stable (hemoglobin 10g/dl, blood pressure 110/70mmHg) but displayed slight hyperventilation with normal blood gases (SO2 95.2%, PO2 90.8mmHg, and PCO2 24.1mmHg) and sinus tachycardia (115–120beats per minute) on ECG. Video-assisted thoracoscopy (VAT) was performed and 2000cm3 of blood removed, although there was no evidence of any source of bleeding in the pleura, diaphragm or lung. The mediastinum appeared swollen, convex, congested and contained blood, as demonstrated by needle aspiration. Within 24h of this minimally invasive method, three-dimensional thin-section computerized tomography (3D-TSCT) of the thorax showed a conspicuous hematoma in the posterior mediastinum, pulmonary artery ectasia, predominantly on the left (4.6cm), and a right BAA (6mm×5mm in diameter) in the area of the hematoma, that was most probably the site of the previous bleeding. On the basis of radiological assessment, we decided to avoid the surgical approach and opted for conservative treatment. Pleural drainage was discontinued on postoperative day 4 and the patient was discharged on day 6, following a repeat chest 3D-TSCT, which showed a drastic reduction of mediastinal hematoma. The follow-up with 3D-TSCT at 4 months and 1 and 2 years revealed resolution of the BAA and total resolution of hemomediastinum. Etiology of BAA can be attributed to increased blood flow, high pressure in the pulmonary artery or various lung diseases.5
Several factors intervened in our choice of a conservative approach: (a) control of bleeding due to the obliteration of the vessel by mediastinal hematoma; (b) the resolution of blood effusion in the pleural cavity after VAT; (c) previous myocardial revascularization (using the left internal mammary artery) with mediastinal fibrosis, making open BAA access difficult; (d) good hemodynamic status. In view of the patient's stable condition, we used VAT as a first-line approach. Moreover, sinus tachycardia and hyperventilation could be symptoms of a worsening general status, requiring an urgent non-targeted approach. Video-assisted thoracoscopy has proved to be ideal for emptying and cleaning the pleural cavity and allowed us to determine that the bleeding originated in the mediastinum (Fig. 1).
Please cite this article as: Divisi D, de Vico A, Crisci R. El abordaje conservador para la rotura de un aneurisma en la arteria bronquial: una opción terapéutica. Arch Bronconeumol. 2015;51:473–474.