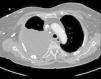
We report the case of an 84-year-old woman, with a history of arterial hypertension, type 2 diabetes, diabetic nephropathy treated with dialysis via a right jugular vein catheter (thrombosed 3 months before admission), and spinal stenosis (L4–L5). She was referred to the emergency department when she reported cough during a hemodialysis session, and pulmonary auscultation revealed diminished breath sounds in the lower half of the right hemithorax. She did not have fever or dyspnea. In the days before admission, she had received amoxicillin/clavulanate for a possible urinary infection. Physical examination showed arteriovenous fistula for hemodialysis access in the left forearm, rhythmic heart sounds with a grade III/IV systolic murmur in the mitral valve, and diminished breath sounds in the right lung base. Complete blood count and biochemistry results were normal, except for proBNP 1750 and triglycerides 99mm/dl. Chest radiography revealed pleural effusion in the lower third of the right hemithorax, thickening of the minor fissure, and catheter in the right jugular vein. A diagnostic thoracocentesis was performed, obtaining milky fluid with pH 7.30, ADA 21U/l, LDH 119U/l, glucose 214mg/dl, total proteins 4.1g/dl, cholesterol 94mg/dl, and triglycerides 870mg/dl. Cytology was negative for malignancy. Chest CT findings included large right pleural effusion, passive atelectasis of the right lung with mediastinal shift, large collateral circulation in the right hemithorax through the azygos/hemiazygos system, and superior vena cava stenosis with a right jugular vein catheter (Fig. 1). The central jugular catheter was removed under fluoroscopic control, and replaced by a femoral catheter. Before chylothorax was diagnosed, a pleural drain was placed, which collected 1800ml. Chest radiograph on discharge showed complete resolution of the pleural effusion, which did not relapse during follow-up.
Patients receiving hemodialysis may develop pleural effusion for diverse reasons. Some may be exudates in the setting of infections, cancers, uremic pleuritis, and hemothorax, but most are transudates caused by volume overload or changes in venous drainage. Chylothorax, on the other hand, is rare.1 In the case of our patient, thrombosis of the central jugular vein catheter led to the appearance of stenosis/obstruction of the superior vena cava, obstructing lymphatic drainage and promoting the formation of chylothorax.
In short, chylothorax is a rarely documented cause of effusion in patients undergoing hemodialysis,2 and requires an appropriate clinical suspicion and a specific therapeutic approach, including withdrawal of the hemodialysis catheter.3
Please cite this article as: De Freitas González EM, Villegas Alcázar JA, García García S. Quilotórax en paciente en hemodiálisis. Arch Bronconeumol. 2017;53:404.