A hydatid cyst in the pulmonary arteries is a very rare presentation of hydatid disease that has been published on a very few occasions. In most cases, it is caused by rupture and embolization of a cardiac cyst1 or hematogenous dissemination from a hepatic focus.2 We report the case of a patient with hydatid cysts in the right lung and pulmonary artery, with no previous history of cardiac or hepatic hydatid disease.
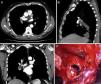
This was a 56-year-old man with no substance abuse or significant medical history who consulted his primary care physician due to a 2-week history of bloody expectoration accompanied by right chest pain. The chest radiograph revealed a polylobulated mass in the right lower lobe with hilar thickening, initially suggestive of lung cancer. Chest computed tomography showed a mass measuring 11×8.8cm in the right lower lobe with hypodense areas suggestive of cysts. The mass showed a 10cm contact with pleural surface, extending with peribronchovascular distribution toward the hilar region. Multiple nodular images of similar characteristics measuring up to 4.5cm were seen inside the artery. Radiological findings were suggestive of pulmonary hydatidosis with invasion of the right lower lobe artery (Fig. 1A–C).
Chest computed tomography showing hypodense nodular images in the interior of the right pulmonary artery suggestive of cysts in the axial, sagittal, and coronal projections (A–C). Intra-operative view after clamping of the right pulmonary artery and arteriotomy of the lower lobe branch, showing hydatid membranes in the interior (D).
After serological confirmation of Echinococcus granulosus infection, the case was presented before the multidisciplinary committee, and the decision was taken to start antiparasitic treatment with albendazole (400mg/12h) and praziquantel (1800mg/12h), with follow-up CT for evaluating treatment response and subsequent surgical resection.
After 6 weeks of antiparasitic treatment, the radiological findings showed little reduction in mass size and persisting internal cavitated areas, along with significant neovascularization originating in the thoracic artery via the bronchial arteries, and in the celiac trunk, via the arteries of the diaphragm. The patient's lung function test results were within normal limits.
Surgical resection was performed, and antiparasitic treatment continued throughout the peri-operative period. Intraoperative findings included hepatization of the lower right lobe, significant vascularization originating in the bronchial arteries, and increased caliber of the right lower lobe artery. After control and clamping of the right pulmonary artery at the extrapericardiac origin, arteriotomy was performed at the lower lobe branch, and the intravascular hydatid cysts were extracted (Fig. 1D). The proximal lumen of the pulmonary artery was aspirated to the level of the clamp. Given the significant perihilar inflammatory reaction, the proximal intermediate bronchus could not be resected, so a middle-lower bilobectomy was performed.
The only post-operative complication presented by the patient was prolonged air leak. He was discharged on day 8 after surgery, and referred to the infectious diseases department for follow-up and control of his medical treatment.
Hydatidosis is a parasitic infection caused by the larval forms of Echinococcus granulosus. The most commonly affected organs are the liver (70%) and the lungs (25%). About 10%–15% of the embryos can spread to other organs via the systemic circulation, including the chambers of the heart, interventricular septum and pericardium (0.02%–2%).2 The pulmonary arteries are an exceptionally rare site of involvement. In our case, the hydatid cyst was located at the level of the right lower lobe, within the right lower lobe artery, presumably due to the parasite implanting in the arterial lumen after crossing the wall through small lesions in the intima, aneurysms, or via the feeder vessels.2
A hydatid cyst located within the pulmonary artery is associated with high mortality rates due to secondary dissemination, embolization, or anaphylactic shock after rupture.3 Hydatid cysts are known to grow 2–3cm/year. Within vessels, cysts grow slowly inside the lumen until it is obstructed. In pulmonary arteries, this process may be sufficiently slow to allow pulmonary perfusion to be adequately established via the bronchial arteries or other collateral branches. This explains why patients may be initially asymptomatic, and why our patient had no signs of occlusion despite total occlusion of the right lower lobe artery.
The differential diagnosis of hydatid cysts in the pulmonary artery should include pulmonary thromboembolism (fat, amniotic fluid, septic emboli, exogenous material) and primary tumors of the pulmonary artery, such as sarcomas.4
Due to the high risk of cyst rupture and anaphylactic shock, surgery should be performed as soon as possible after diagnosis. The extraction of endovascular cysts even in asymptomatic patients is recommended.5 As this form of hydatidosis is so rare, no standardized surgical techniques have been described, so treatment must be individualized. The approach will depend on the adherence of the hydatid cyst to the arterial wall and its anatomical location. Surgical treatment must focus on preventing cyst rupture and migration, which may have fatal consequences, such as secondary dissemination, embolism, anaphylactic shock, and the formation of pseudoaneurysms.6 In our case, we clamped the right pulmonary artery to avoid such complications. Unilateral obstruction of the pulmonary artery can be successfully treated with arteriotomy and cyst resection with or without lung resection, or with pulmonary endarterectomy. In situations of concomitant pulmonary and arterial involvement, a 2-stage surgical intervention can be considered: first, resection of the intra-arterial hydatid cyst, followed by cystectomy or lung resection.7
Recommended treatment of intra-arterial hydatidosis is surgical intervention followed by complementary medical treatment. CT follow-up is indicated to detect possible recurrences or development of pseudoaneurysms.2
Please cite this article as: Gómez Hernández MT, Rodríguez Pérez M, García Hernández P, Jiménez López MF. Un ocupante insólito de la arteria pulmonar. Arch Bronconeumol. 2017;53:402–404.