Chronic obstructive pulmonary disease (COPD) is characterized by chronic, progressive, irreversible airflow limitation associated with exposure to tobacco smoke and, to a lesser extent, inhalation of occupational or environmental toxins or biomass combustion products.1–3
COPD is a complex, heterogeneous disease that confers high morbidity and mortality. The World Health Organization (WHO), in an update of the Global Burden of Disease Study published in 2010, reported a significant increase in the number of COPD sufferers, estimated at 328615000 individuals worldwide. Currently this disease is the third cause of death, after ischemic heart disease and cerebrovascular disease.4
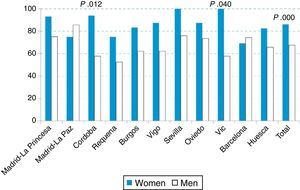
Data from the 2007 EPI-SCAN study indicate that the prevalence of COPD in Spain is 10.2% (15.1% in men and 5.7% in women) of the population aged between 40 and 80 years.5 The rate of underdiagnosis can be as high as 73%, although this varies widely depending on geographical region, and distribution among the sexes is uneven, with 1.27 times more women being underdiagnosed than men (Fig. 1).6
In Spain, population aging, which affects women more than men due to their greater longevity, and the massive surge in smoking among women during the 1970s have led to an increase in smoking-related diseases particularly in middle-aged women, and with it not only an increase in prevalence, but also in associated morbidity and mortality. According to a U.S. study, the rate of mortality associated with COPD in women rose 5-fold in that country between 1971 and 2000, and in 2000, the number of deaths due to COPD in women (59936) overtook that of men (59118).7
Despite these data, COPD is still considered mainly a “man's disease”, causing a diagnostic bias that contributes to underdiagnosis in women. Two similar studies, one conducted in the U.S. and Canada8 and the other in Spain,9 concluded that diagnosis of COPD was biased according to the sex of the patient. The results showed that men have a 1.5-fold chance of receiving a provisional diagnosis of COPD, a bias that is significantly reduced when abnormal spirometry results are available.
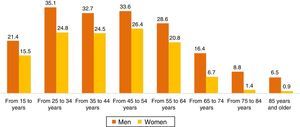
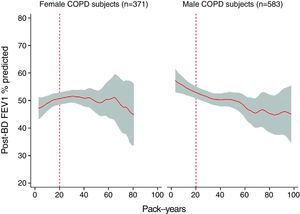
Risk FactorsThe main risk factor for developing COPD is smoking (Fig. 2). Numerous studies have evaluated the hypothesis that women are more susceptible to the toxic effects of tobacco than men. A study published in 1997 that included 13987 individuals from 2 populations in Denmark10 concluded that smoking has a greater impact on the deterioration of lung function in women than in men, a result that corroborated earlier findings.11,12 Later, Sorheim et al.13 observed that in a group of COPD patients aged under 60 years, women who smoked less (<20 pack-years) had lower absolute and percentage values for forced expiratory volume in 1 second (FEV1) than men; while women with a smoking history of more than 25–30 pack-years had similar figures to men (Fig. 3).
Dose–response relationship between number of pack-years and predicted percentage of forced expiratory volume in first second after bronchodilation (post-PBD FEV1% predicted) in female COPD subjects and male COPD subjects, expressed by linear regression with 95% confidence interval.
Greater susceptibility to tobacco may be determined by anatomical (smaller airways), genetic and hormonal factors, and this difference may manifest already in childhood, since girls undergo greater lung function deterioration than boys when exposed to smoke or environmental pollution.14 Foreman et al.15 analyzed the data from 2500 individuals included in the Genetic Epidemiology of COPD (COPDGene) study, and concluded that women and African Americans may be more susceptible to the toxic effects of smoking, since they experience more severe disease forms with earlier onset. The results of this study also indicate that a maternal history of smoking or respiratory diseases were also significantly associated with earlier and more severe forms of COPD.
In biological terms, studies conducted in animals confirm that females may be more susceptible to the deleterious effects of smoking. Estrogens and other related compounds may increase the expression of the cytochrome P450 (CYP) enzyme, which is directly involved in the metabolism of some of the components of tobacco smoke, such as polycyclic aromatic hydrocarbons. Bioactivation of these compounds by CYP produces reactive substances that are highly toxic to the lung and potentially carcinogenic.16,17
Other risk factors for the development of COPD, in addition to smoking, include environmental pollution, which is increasing in developed countries, and occupational exposure to organic dusts, coal, heavy metals, textiles, tin, ceramics, and glass. One etiological factor that is growing in importance is exposure to smoke from biomass combustion, which primarily affects women in rural areas and/or in developing countries, who cook in poorly ventilated environments where concentrations of material particles in room air are higher than the recommended levels.18 Published data emerging mainly from Latin American cohorts in Mexico and Colombia19,20 suggest that the clinical presentation of COPD caused by this exposure has a greater component of chronic bronchitis and less emphysema, while survival rates are similar to those of women with COPD caused by smoking.21
Clinical PresentationDyspnea is one of the characteristic symptoms of COPD and one of the main prognostic factors determining survival and quality of life of these patients.22
According to several published studies,23,24 women report higher grades of dyspnea than men, measured according to the modified Medical Research Council (mMRC) scale, even with similar airflow obstruction and less exposure to tobacco. A study published by De Torres et al.25 shows that in women, but not in men, the best predictor of dyspnea is the central respiratory drive, suggesting that other non-physiological factors, such as anxiety or depression may be involved and should be systematically evaluated in these patients.
Cough and chronic expectoration are other symptoms that also characterize respiratory diseases and COPD in particular. A study published in 2012 in 4500 COPD patients, 740 of which were women, concluded that female patients reported higher grades of dyspnea than males, but less cough and expectoration.26 The results of the EPI-SCAN also found that women with COPD have comparatively less sputum production than men, a factor that may be affected by social factors.6
Wheezing is more common in women with COPD than in men,27 probably because they have more airway involvement and greater bronchial hyperreactivity, which may be a reason for the high incidence of the mixed COPD-asthma phenotype among women smokers.28,29
Exercise capacity is determined with a submaximal exertion test, the 6-minute walk test (6MWT), and, like dyspnea, is another predictor of mortality in COPD patient. Several studies have found that both male and female COPD patients have lower than expected exercise capacity, and this parameter is more useful as a prognostic factor in men.30 It was initially thought that this limitation was due to respiratory dysfunction (airflow resistance and pulmonary hyperinflation as an independent mortality factor both in men and in women31), although we now know that it is due in large part to differences in the use of oxygen by skeletal muscle.32 In a study measuring the results of cardiopulmonary exercise tests performed on a cycle ergometer, women with COPD showed lower peak anaerobic power and lower optimal velocity than men, probably related with loss of lean muscle mass in the lower limbs.33
Several studies have shown significant differences in the prevalence and distribution of emphysema between men and women with COPD. Martínez et al.34 of the National Emphysema Treatment Trial Research Group (NETT) included 1053 patients (409 women) undergoing screening for a lung volume reduction surgery program, and compared clinical, physiological, radiological, and histological data from a small subgroup of patients. Comparatively, women had smaller airway diameters with proportionately thicker walls; emphysema was less extensive than in men, and predominantly central in distribution. Dransfield et al.35 found that, irrespective of disease severity, male COPD patients who were smokers or former smokers had greater areas of emphysema on radiography than women with the same disease. However, a study published by Hardin et al. in 2016 concluded that women in 3 phenotype subgroups (early-onset COPD, severe emphysema, and grade IV COPD according to Global Initiative for Obstructive Lung Diseases (GOLD) criteria) had a comparable grade of emphysema to men, despite a lower pack-year index.36
Nutritional status is a basic clinical parameter that must be evaluated in COPD patients using body mass index (BMI) or fat-free mass index (FFMI) measured with bioimpedance. A study published in 1999 showed that COPD-related mortality increased considerably when BMI was lower than 21.37 Several subsequent papers indicate that nutritional changes are more prevalent in women with COPD than in men.24,30 According to a study published in 2006, a reduced FFMI in patients with normal BMI is closely related with the female sex, so the complete and systematic evaluation of the nutritional status in women is recommended, in view of its potential as a prognostic factor.38
Exacerbations are episodes of clinical instability that cause significant deterioration in health-related quality of life among COPD patients, affecting disease progression and increasing the risk of death.39 According to the available data, women have a greater number of exacerbations,24,40,41 but hospitalization rates are similar in both women and men, and readmission and survival rates after exacerbation are better in women.42
Concomitant DiseaseCOPD is a complex disease with multisystem manifestations, and is associated throughout its course with other diseases or comorbidities that complicate the health status and prognosis of these patients. Some of the most common include cardiovascular diseases, lung cancer, osteoporosis, diabetes mellitus, and affective disorders (anxiety and depression).
According to the ECLIPSE study,41 cardiovascular diseases are less prevalent in women with COPD, while osteoporosis and affective disorders are more common in women than in men. The results of the ECCO study43 indicate that there are significant sex-dependent differences in the comorbidities of these patients, and these may be underestimated if the only method of quantification used is the Charlson index. According to this study, women with COPD have a lower prevalence of ischemic heart disease than men, but a higher rate of heart failure, osteoporosis, and diabetes.
Anxiety and depression are very common among COPD patients and have a significant impact on the disease because of their effect on symptom management, quality of life, and prognosis. Studies in this area indicate that women have much higher rates of anxiety and depression, even when disease involvement is moderate in terms of airflow obstruction and respiratory symptoms.44 Anxiety and depression in women with COPD is associated with a greater risk of exacerbation, longer hospital stays, persistent smoking habit, less physical activity, greater mortality, and possibly poorer treatment adherence.26
Osteoporosis is one of the most important comorbidities associated with COPD, with a prevalence of around 35%. It predominantly affects women, particularly after menopause. Factors such as age, smoking, and the use of systemic corticosteroids are involved in the development of osteoporosis in these patients and are associated with more severe forms of the disease and a poor nutritional status. Clinical management of COPD patients, then, must include a bone scan and determination of bone mineralization markers, so that early treatment with bisphosphonates, calcium (if dietary intake is insufficient), and vitamin D supplements can be started if deficiencies are detected.45
PrognosisHealth-related quality of life is a parameter directly associated with hospitalization, use of healthcare resources, response to treatment or mortality in COPD patients, and can be evaluated with the Saint George's respiratory quality of life questionnaire (SGRQ). Health-related quality of life is poorer among women with COPD than men, and women begin to experience symptoms at an earlier age and with less severe airflow obstruction. In men, parameters such as dyspnea, exercise capacity, degree of hyperinflation, or comorbidities are significantly associated with the overall SGRQ score, whereas in women only dyspnea and arterial oxygen tension are significantly correlated, suggesting the need to find other factors for evaluation, such as anxiety or depression, that might explain the greater and earlier deterioration in quality of life among women.46
Until relatively recently, disease prognosis was evaluated purely on the basis of lung function involvement measured according to the predicted percentage of FEV1. This changed drastically with the introduction of multidimensional indexes, such as BODE (Body mass index [BMI], Airflow obstruction, Dyspnea, Exercise capacity), which have greater prognostic value and better represent the heterogeneous nature of the disease47 A study published in 2007 suggested that the proportional weight of each of the components of the BODE index varied between men and women, and that in women the most important parameter was dyspnea grade according to the mMRC scale and BMI.30 Despite these variations, BODE is an excellent predictor of mortality (respiratory and all-cause) in both sexes.31
TreatmentSmoking is the major risk factor for COPD in the developed world, so smoking cessation is the main intervention for delaying the progressive decline in lung function seen with this disease.2 As mentioned above, women appear to be more susceptible than men to the toxic effects of tobacco, and some studies show that they are less likely to give up smoking, and that their long-term cessation rate is lower than in men, probably because they experience less symptomatic benefit after smoking cessation. However, according to the results of the Lung Health Study, women who give up smoking definitively experience an improvement in lung function (FEV1) 2.5 times greater than that of men.48 Some of the most widely used drugs in smoking cessation, such as bupropion and varenicline, appear to be as effective in women as in men, while nicotine replacement therapy is more effective in men.49
Pharmacological treatment for COPD is based on long-acting bronchodilators administered via inhalation devices, and a good inhalation technique is essential to ensure their efficacy. A study published in 1994 found that inhalation technique was poorer among women than men in the same age group, and errors in each of the inhalation procedures were observed. Proper training in the use of these devices is essential to optimize treatment.50 In the past, few studies on the use of pharmacological agents in COPD were designed to evaluate efficacy by sex, so the information available on the peculiarities of inhaled treatment in women is scant and occasionally contradictory. In the TRISTAN study, Vestbo et al.51 reanalyzed the efficacy of the combination of salmeterol/fluticasone on lung function (FEV1), exacerbation rates and quality of life of COPD patients, and found no differences between sexes. However, a more recent meta-analysis published by Soriano et al.52 reported greater improvement in lung function in COPD patients in the first 6 months of treatment with inhaled corticosteroid in women (this finding again supports the idea of greater bronchial hyperreactivity among women), and in patients who had given up smoking. The results of the UPLIFT study, which evaluated the effects of tiotropium bromide on lung function, quality of life, and exacerbations, found no significant differences according to sex.53 Although these studies contribute significant information with possibly therapeutic implications, new studies are needed to draw a more accurate picture of the appropriate medical treatment of women with COPD.
Respiratory rehabilitation has been shown to be a mainstay in the treatment of COPD, since it improves dyspnea, quality of life, exercise tolerance, and reduces exacerbations and the use of health resources. Rehabilitation programs must combine peripheral muscle training with specific respiratory muscle training, psychosocial/behavioral education, and nutritional interventions, among others. The minimum recommended duration of programs is 8 weeks or 20 sessions, at a rate of 2–5sessions/week.39,54 Studies that evaluate the response of COPD patients to pulmonary rehabilitation programs have found no significant differences in benefit with regard to sex, but it must be mentioned that women obtain a much greater benefit in the initial months of physical training, similar to the long-term effect.55
Long-term home oxygen therapy (LTOT) is indicated in patients with COPD and severe resting hypoxemia as it improves quality of life and survival, but differences in the effect of this treatment between the sexes is not clearly defined. Studies, such as that of Miyamoto et al.,56 found that women receiving LTOT had improved survival compared to men, irrespective of the etiology of their respiratory failure. These results were subsequently confirmed by Crockett et al.57 and Franklin et al.58 In contrast, a recently published study by Machado et al.59 showed that among patients with COPD receiving LTOT, survival is significantly lower in women, in individuals with lower BMI, and in those with higher grades of respiratory failure. These conflicting results underline the need for new studies to evaluate the possible existence of a difference between sexes in response to LTOT.
Unfortunately, we do not have any specific information on the effect of sex on the results of surgical (lung volume reduction) or endoscopic (valves or coils) treatment for reducing lung volume in patients with emphysema. However, given the unique characteristics of the clinical presentation of COPD in women, differences in response to these treatments are only to be expected.
ConclusionsCOPD is a growing health issue among women. Our priority is to design educational programs and training courses to emphasize the importance of COPD in the female sex and to help raise clinical suspicion and reduce underdiagnosis. Similarly, the therapeutic management of these patients must be optimized with better differential characterization and special attention to comorbidities such as osteoporosis, anxiety or depression.
We would like thank María Pilar Ausín (Servicio de Neumología. Hospital del Mar, Barcelona), JB Soriano (Servicio de Neumología, Hospital Universitario de La Princesa, Instituto de Investigación Sanitaria Princesa [IP], Madrid), and Julio Ancochea (Servicio de Neumología, Hospital Universitario de La Princesa, Instituto de Investigación Sanitaria Princesa [IP], Madrid) for their important contribution to this manuscript.
Please cite this article as: Alonso T, Sobradillo P, de Torres JP. Enfermedad pulmonar obstructiva crónica en mujeres: ¿somos diferentes? Arch Bronconeumol. 2017;53:222–227.