Bronchiolitis obliterans (BO) after hematopoietic stem cell transplantation (HSCT) is a serious, potentially fatal complication, which generally appears in the context of graft-vs-host disease (GVHD).1,2 The clinical presentation of BO after HSCT is non-specific, and no universal consensus is available on the diagnostic criteria of this entity, although imaging studies, particularly computed tomography (CT), dynamic inspiratory CT (iCT), and expiratory CT (eCT), are of growing diagnostic value in the detection of this complication.3,4
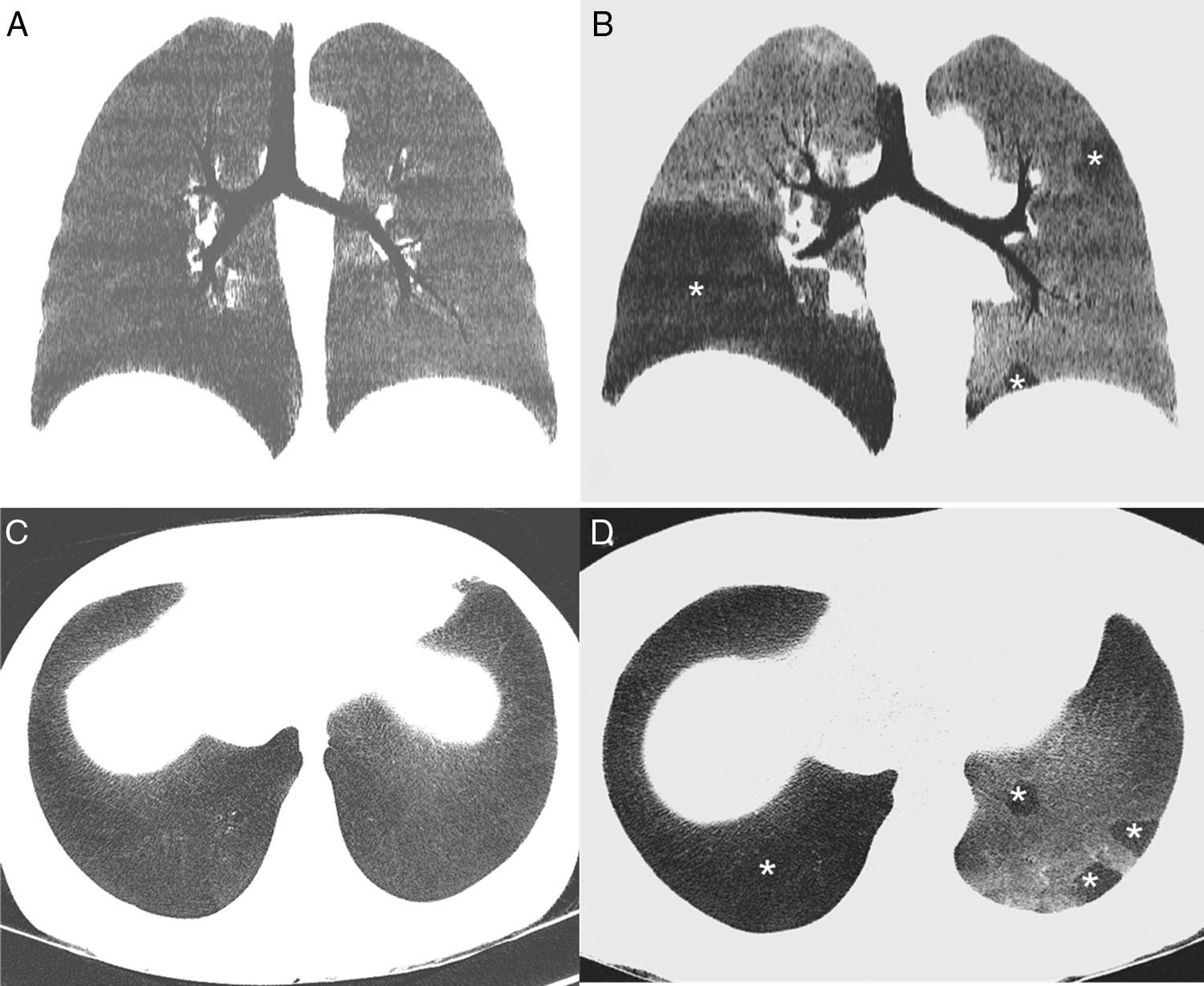
We report the case of a 44-year-old woman with a history of acute myeloid leukemia, treated 6 months previously with unrelated donor HSCT, who consulted due to dyspnea and dry cough. As a complication of the HSCT, the patient had transitory cytomegalovirus viremia and cutaneous GVHD grade III, which responded favorably to treatment with corticosteroids. No parenchymal opacities were observed on chest radiograph, but chest iCT and eCT revealed a marked mosaic pattern in the pulmonary parenchyma in the expiratory phase, and multiple areas of air trapping were identified in both lungs (Fig. 1), while infectious complications were ruled out. Areas of air trapping on CT can be better viewed with the use of the minimum intensity projection (minIP), an algorithm for visualization of images that enhances areas of less attenuation. Lung function tests (LFT) showed a mild reduction (<20%) in forced expiratory volume in 1 second (FEV1) and increased residual volume (RV) (138%) with respect to pre-HSCT values. No changes were observed on fiberoptic bronchoscopy and bronchoalveolar lavage ruled out opportunistic infections. Given these findings, a diagnosis of BO was given, and the patient responded favorably to treatment with high-dose systemic corticosteroids (stabilization of functional tests).
(A) minIP coronal reconstruction of the chest inspiratory CT showing homogeneous pulmonary parenchyma with uniform attenuation. (B) minIP coronal reconstruction of chest expiratory CT, showing a mosaic pattern of the pulmonary parenchyma, with areas of low density (asterisk), alternating with areas of greater attenuation. Low density areas (affecting particularly the right lower lobe and the left lung in a patchy pattern) correspond to areas of air trapping, while the areas of greater density correspond to normal pulmonary parenchyma. (C) minIP axial reconstruction of the chest inspiratory CT showing homogeneous pulmonary parenchyma. (D) minIP axial reconstruction of chest expiratory CT, showing areas of low density (asterisks), related with areas of air trapping.
BO is the most common non-infectious complication of HSCT, and is usually diagnosed about 6–12 months post-transplantation.1 Some risk factors for the development of post-HSCT BO include age over 20 years, pre-HSCT airflow obstruction, the appearance of viral respiratory infections in the early post-transplantation months, but the most significant of all is the presence of chronic GVHD.2 Clinical presentation is often insidious, and symptoms are unspecific (cough, dyspnea), although 20% of patients can be asymptomatic. Long-term prognosis is generally poor, and the aim of treatment is to prevent progression of airflow obstruction. No universally accepted diagnostic criteria have been accepted for the diagnosis of post-HSCT BO, but the National Institutes of Health of the United States suggest the following criteria: (1) demonstrated airflow obstruction (FEV1/forced vital capacity [FVC]<0.7 and FEV1<75% predicted value); (2) evidence of air trapping on iCT and eCT, RV>120% predicted value, or histological confirmation of BO; and (3) absence of respiratory tract infection (clinically, radiologically, or microbiologically documented).5 The most significant radiological finding of BO is the demonstration of air trapping on eCT (with respect to iCT), which has a sensitivity of 91% and 94% in some studies, respectively; these radiological changes can precede LFT changes.2,3 We believe that dynamic CT (iCT and eCT) should be performed in all symptomatic HSCT patients for the early detection of BO, since this serious pulmonary complication cannot be detected on iCT alone.
Please cite this article as: Gorospe Sarasúa L, Barrios-Barreto D, García Gómez-Muriel I, Chinea-Rodríguez A. Bronquiolitis constrictiva tras trasplante de progenitores hematopoyéticos: importancia de la tomografía computarizada espiratoria. Arch Bronconeumol. 2017;53:349–351.