Endobronchial ultrasound-transbronchial needle aspiration (EBUS-TBNA) is a minimally invasive technique used to sample structures adjacent to the tracheobronchial wall, such as adenopathies and/or mediastinal tumors, under real-time ultrasound control.1,2 The main indication for this technique is the diagnosis and staging of lung cancer, but it can also be very useful in other diseases, such as sarcoidosis or tuberculosis.
EBUS-TBNA is a safe technique, with a complication rate of between 1.23% and 1.44%.3,4 Pneumothorax, hemorrhagic accident, and infection are some of the main complications described.
We report the case of a 65-year-old man who consulted for persistent cough and purulent expectoration. Significant history included bilateral bronchiectasis and recurrent respiratory infections, with positive cultures of Stenotrophomonas maltophilia and Pseudomonas aeruginosa.
A chest computed tomography (CT) scan was performed, revealing already known bilateral bronchiectasis, along with mediastinal adenopathies (4, 5, 7, and 10R) and bilateral pulmonary infiltrates predominantly in the upper right lobe, both of which were new. On the basis of these findings, EBUS was performed, and a subcarinal adenopathy, 3cm in diameter, was observed. Multiple TBNA passes were performed in this adenopathy, along with bronchoalveolar lavage and bronchial aspiration, and material for microbiological and pathology studies was obtained.
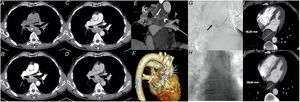
Five days later, while awaiting results, the patient attended the emergency room with an history of several hours of chest pain, irradiating to his back, which worsened with deep inspiration. Laboratory tests revealed no significant findings. Chest X-ray showed increased retrocardiac density. The study was completed with a chest CT scan after intravenous administration of contrast medium that revealed the presence of a large mediastinal hematoma (13cm craniocaudal diameter), with possible extravasation of intra-hematoma contrast at the subcarinal level, coinciding with the aspirated adenopathy. Given these findings, we decided to complete the study with a thoracic CT angiogram scan (3h later) that confirmed the presence of a hyperdense mediastinal collection in the study, without contrast material (Fig. 1A). A hypervascular nodular image measuring 8mm in the subcarinal region was observed in the arterial phase (Fig. 1B). The lesion was not observed during the early and late venous phases of the study (Figs. 1C and D), ruling out the presence of an active point of bleeding. The maximum intensity projection (MIP) showed that this hypervascular structure was dependent on the right bronchial artery (Fig. 1E), suggesting a diagnosis of bronchial artery pseudoaneurysm. The diagnosis was confirmed by angiogram (48h later), in which a 10mm pseudoaneurysm was identified at the bifurcation of the right inferior bronchial artery (Fig. 1G). Angiographic occlusion of the pseudoaneurysm was performed using 1.3ml of liquid embolic agent (Squid-12®; Emboflu, Gland, Switzerland), and closure was confirmed (Fig. 1H). A follow-up CT was performed after arterial embolization, in which a significant decrease in the extension and diameter of the mediastinal hematoma was observed with respect to the CT scan performed 10 days earlier (Fig. 1 I-J).
A) Non-contrast-enhanced phase of chest CT angiogram. Extensive mediastinal hematoma (*). B) Arterial phase of the study. Hypervascular nodular image within the subcarinal adenopathy, associated with right bronchial artery pseudoaneurysm. C-D) Early and late venous phases. No significant extravasation of contrast medium is observed to suggest active bleeding; note the vascular (arterial) nature of the lesion. E) Maximum intensity projection (MIP) in the oblique coronal plane. The nodular image (pseudoaneurysm, white arrow) can been seen to depend on the right bronchial artery (arrowhead). F) Volume-rendering. 3D reconstruction indicating the pseudoaneurysm (white arrow). G) Angiogram shows a contrast-filled nodular structure, with no extravasation in venous or parenchymal phases, consistent with pseudoaneurysm of the right inferior bronchial artery. H) Closure of the pseudoaneurysm after embolization. I-J) Mediastinal hematoma before (48.83mm) and after embolization (28.60mm).
The EBUS-TBNA pathology report was negative for malignancy. Pseudomonas aeruginosa was cultured from the aspirate, and treatment began with intravenous ceftazidime and inhaled tobramycin. The patient remains asymptomatic 5 months later, after resolution of the infectious process.
Complications of EBUS-TBNA are rare, but hemorrhagic accident is one of the most common.3,4 The site and size of the structures under study, together with respiratory movements and arterial pulse can make this technique difficult and increase the risk of this complication.5 Aspiration needles now have safety systems to control the depth to which the needle needs to be advanced for sample collection. Moreover, the real-time visualization of the puncture site allows the distance from the center of the lesion and/or adenopathy to the point of entry of the needle to be measured.1. Despite these safety measures, the possibility remains of inadvertently puncturing mediastinal vessels, an occurrence that does not generally lead to major complications. Indeed, several studies have described EBUS-guided aspiration through vascular structures as a reliable and safe diagnostic technique.6,7
Most post-puncture bleeds associated with mediastinal vessels are self-limiting and do not require further intervention.2 In the AQuIRE study, hemorrhagic accidents required management in 0.2% of patients.3
In general, most bleeding events occur immediately after the vessel is punctured, and are diagnosed in situ with real-time ultrasound imaging. However, in our case, no ultrasound changes were detected at the end of the test and clinical manifestations did not appear until 5 days after EBUS. Few reports to date describe complications following EBUS-TBNA. After an exhaustive review of the literature, we present the first case of bronchial artery pseudoaneurysm as a complication of EBUS-TBNA.
Aneurysms and pseudoaneurysms of the pulmonary vascular structures are rare but potentially life-threatening, so they must be managed and treated urgently. Iatrogenesis and trauma are the main causes of pulmonary pseudoaneurysm.8 Pulmonary arteries are the most frequently affected vessels, ahead of the bronchial arteries or pulmonary veins. Hemoptysis and chest pain are the most common initial symptoms. However, pseudoaneurysms can sometimes be detected as incidental findings on imaging tests.
The bronchial arteries originate primarily from the proximal region of the descending aorta. Right bronchial arteries, however, often originate from the intercostal arteries.9 In both cases, these vessels are part of the systemic circulation, which implies an increased risk of bleeding after puncture. Bronchial circulation plays an important role in chronic inflammatory and infectious diseases involving the lung parenchyma and airways, and responds to damage by enlarging or dilating vessels in an attempt to maintain blood flow to damaged áreas.10 Bronchiectasis is one of the main causes of hypertrophy and/or dilatation of the bronchial arteries, and is a risk factor for the appearance of complications such as bleeding, as described in our case.
To conclude, we present a case of bronchial pseudoaneurysm following EBUS-TBNA, a complication not previously reported in the literature. In most cases, hemorrhagic accidents occur immediately after puncture of the mediastinal vessels during EBUS. However, our case is an example of how bleeding in significant amounts and in a sensitive location can be associated with late clinical manifestations. Imaging techniques such as thoracic angio-CT and angiogram are highly useful in the diagnosis and control or treatment of bleeding.
Please cite this article as: Recalde-Zamacona B, Ezponda A, Zulueta JJ, Marín-Oto M, Alcaide AB, Campo A et al. Seudoaneurisma de arteria bronquial y hematoma mediastínico tras EBUS-TBNA. Arch Bronconeumol. 2021;57:142–143.