We report a case of benign metastasizing leiomyomatosis (BML) manifesting as a giant pleural mass. To the best of our knowledge, this is the first reported case of thoracic BML with isolated pleural involvement (no pulmonary involvement), and the only report in the literature of pre-operative embolization of this type of lesion to minimize the risk of bleeding during surgery.
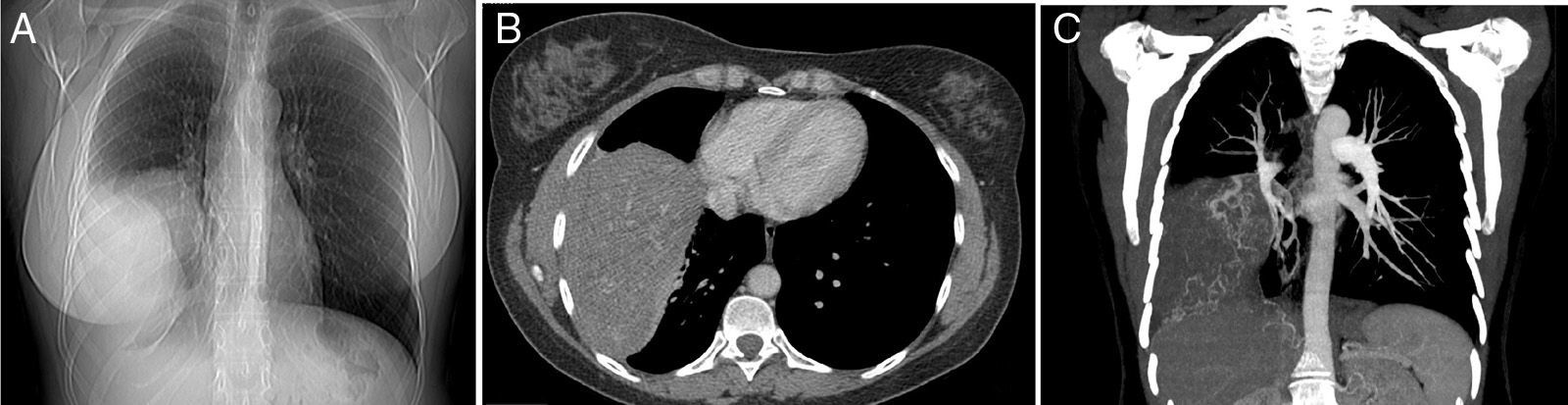
The patient was a 48-year-old woman, non-smoker, who presented due to a 1-month history of cough. Her only significant medical history was hysterectomy for uterine myomatosis 9 year previously. A large mass in the right hemithorax was observed on chest X-ray. Chest computed tomography (CT) revealed a large, solid, extraparenchymal mass, 20cm in its longest diameter, with marked arterial vascularization from the right phrenic, intercostal and bronchial arteries, and right internal thoracic artery (Fig. 1).
Posteroanterior chest X-ray (A) showing a large mass in the right hemithorax. Chest computed tomography with intravenous contrast medium confirming the presence of a solid extraparenchymal mass in the pleura (B) with marked systemic arterial vascularization from the right bronchial, intercostal, internal thoracic and phrenic arteries (C, coronal reconstruction with maximum intensity projection).
A CT-guided core needle biopsy was obtained from the pleural mass and diagnosed as leiomyoma. Histology was identical to that of the previously resected uterine myomas. On the basis of the histology results, a presumed diagnosis of BML was given.
Given the significant systemic vascularization of the pleural mass, we decided to perform preoperative embolization with a view to simplifying resection of the lesion. Selective embolism of the distal branches of the right internal thoracic artery and the right phrenic artery was performed with 500 microparticles, and vascularization of the mass was successfully reduced. Two days later, right posterolateral thoracotomy was performed and the pleural mass was completely removed. Bleeding during the procedure was estimated to be less than 100ml. Pathological examination of the resected specimen confirmed the diagnosis of BML. No significant complications occurred during the postoperative period. Twelve months after surgery, the patient remains asymptomatic and without radiological signs of local or distant relapse.
BML is a rare disease, characterized by the development of smooth muscle tumors originating from uterine leiomyomas that require hysterectomy in most cases. The mean time from hysterectomy to the appearance of metastasis is 15 years with a range of 3–20 years.1,2
The most widely accepted ethiopathogenic theory is that MBL metastases are caused by hematogenous spread from the uterine tumor at the time of surgery, but isolated cases have been reported in which metastasis has appeared even before hysterectomy.1,2 Thoracic MBL metastasis occurs most frequently in the lung, but lymph node, cardiac, and vertebral and retroperitoneal spine involvement have been reported.3 Most patients are clinically asymptomatic and MBL is discovered by chance during imaging studies performed for another reason. Some patients with thoracic involvement can have symptoms such as cough, chest pain and dyspnea.2,3
Only one case of BML with pleural involvement has described the scientific literature, but this was associated with lung lesions.4 Our case is the only one published to date with isolated pleural involvement and no pulmonary lesions, and is also the largest BML chest lesion reported to date (20cm).
Treatment of choice is usually surgical resection, often accompanied by estrogen suppression via bilateral oophorectomy or hormone treatment (due to the presence of estrogen and progesterone receptors in both metastatic lesions and uterine leiomyomas).2 In our case, we decided to perform preoperative embolization due to the large size and hypervascularity of the tumor. This is the first case of BML with presurgical embolization for reducing the risk of intraoperative bleeding reported in the literature, although this procedure is common in other thoracic tumors.5 One case of embolization of a pulmonary MBL has been reported, but in that case, the intention was to treat life-threatening hemoptysis.6
In conclusion, this is an exceptional case of giant MBL with isolated pleural involvement in a patient with a history of uterine myomas. The pleural mass was embolized before surgery to minimize the risk of bleeding.
Please cite this article as: Abad Fernández C, Romera Sánchez R, Gorospe Sarasua L. Presentación de leiomiomatosis benigna metastatizante como una masa pleural gigante sin afectación pulmonar. Arch Bronconeumol. 2016;52:51–52.