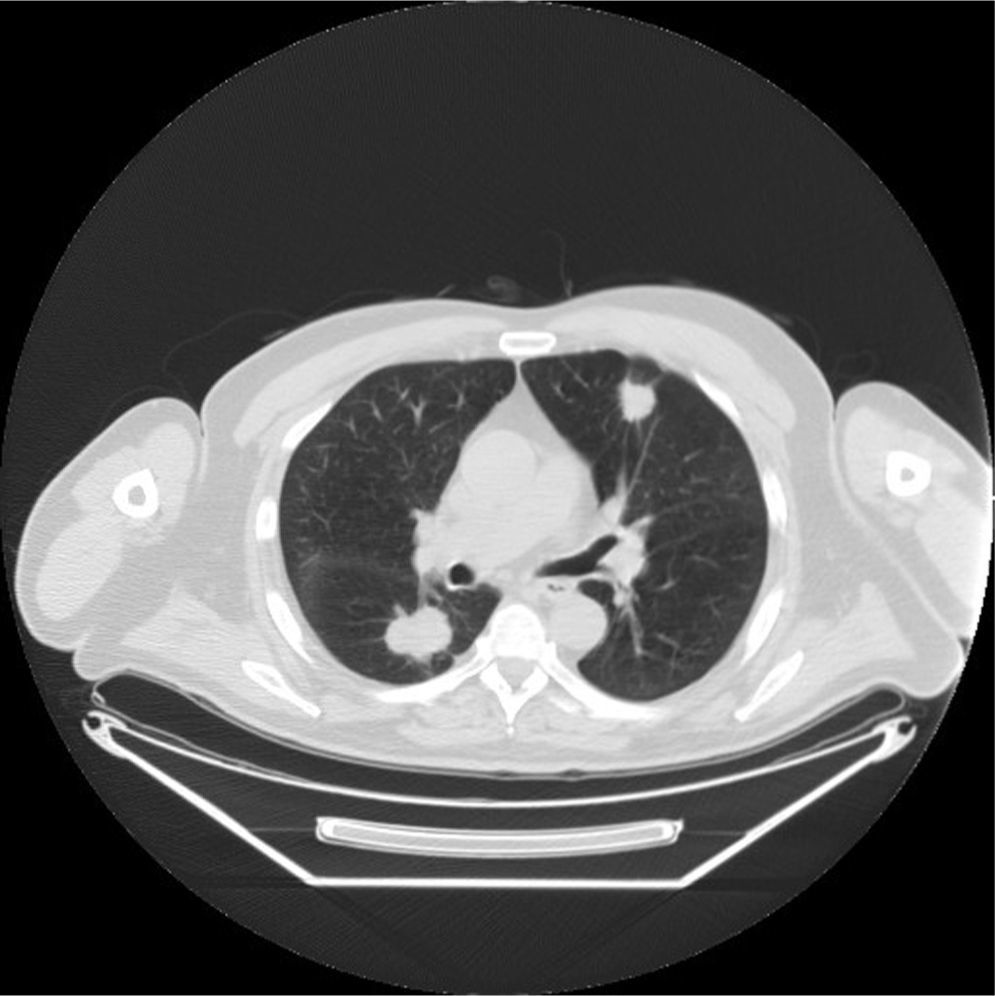
We report the case of a 65-year-old man with no significant clinical history who was referred to the respiratory medicine department after a pulmonary nodule was identified during a preoperative workup for a cataract operation. After the initial evaluation, computed tomography (CT) was performed, which revealed several pulmonary lesions: 1 in the right lower lobe (RLL), 1 in the left upper lobe (LUL), and 1 in the left lower lobe (LLL), suggestive of synchronous lung tumors. Positron emission tomography (PET-CT) confirmed the presence of pulmonary lesions with increased uptake, indicative of malignancy (Fig. 1). Fiberoptic bronchoscopy was normal. CT-guided fine needle aspiration and biopsy was performed for histological diagnosis, and the pathology report confirmed non-lymphoid adenoid cystic carcinoma with chondroid stroma induction. Immunohistochemistry showed negativity for gliofibrillar protein, cytokeratins 8/18 and 19, TTF1 and osteocalcin, and weak cytoplasmatic positivity to VT1 and intense positivity to AE1/AE3 and vimentin. We discussed the case with the pathologist and concluded that the histological picture was reminiscent of malignant mixed tumors of the salivary glands. Accordingly, magnetic resonance imaging and eye, nose and throat (ENT) examination were performed to rule out maxillofacial disease. Both examinations were strictly normal, so the final diagnosis was adenoid cystic carcinoma, probably of pulmonary origin. We came to this conclusion because, while the most common origin is the salivary glands, these tumors have been reported to occur in other sites, such as the trachea, breast, or lung, as in our patient. Adenoid cystic carcinoma of the lung is rare, and accounts for 0.1%–0.2% of lung tumors.1
The natural history of this tumor is not well defined, and it is generally thought to grow and progress slowly. However, some reports of rapid, refractory evolution have appeared in the literature. The first line of treatment should always be surgery, if possible, but the rarity of the entity means that no standard treatment has been established. In recent years, interest in this tumor has grown, since cases with c-kit mutations that have shown sustained response to imatinib2–4 have been reported.
We would like to illustrate 2 points with this case: firstly, when adenoid cystic carcinoma is detected in the lung, an ENT examination must be performed to exclude the possibility that the lesions are metastatic disease; and secondly, it underlines the lack of treatment for orphan tumors, a situation which seriously affects their prognosis.
Please cite this article as: Cruz Castellanos P, D’Errico G, Miranda J, de Castro Carpeño J. Adenoma pleomórfico pulmonar. A propósito de un caso. Arch Bronconeumol. 2016;52:50.