We present a Myotonic Dystrophy type 1 (DM1) patient with nocturnal alveolar hypoventilation, who performed twelve weeks of inspiratory muscle training (IMT).
A 54-year-old DM1 male, classical phenotype, visited the outpatient-clinic because of progressive fatigue and dyspnoea. Pulmonary function was stable with reduced forced vital capacity of 3.2L (64%) and severely reduced maximum inspiratory muscle strength (PImax) of 17.95cmH2O (19.7%). A nocturnal transcutaneous gas-exchange measurement showed a median of PtcCO2 6.6kPa (49.5mmHg) and four episodes of 30min hypoventilation (probably REM sleep related), with deep oxygen desaturations of 80% and PtcCO2 increases to 7.5kPa (56.3mmHg). While he was placed on the waiting list for initiation of non-invasive home mechanical ventilation (HMV), he started a 12 week home based IMT programme, after written informed consent. During this period he did not start with HMV, nor other modifications in treatment were made. Based on positive effects of IMT in neuromuscular disorders and of general exercise training in DM1, we hypothesized that IMT could improve his weakened respiratory muscles and respiration.1–3 Training programme consisted of two sessions per day at five days a week. He used an electronic POWERbreathe KHP2 device (Hab international, Southam, UK) and wear a nose clip. One session included 30 inspirations against resistance, started on 30% of baseline PImax (5cmH2O). The resistance was increased every two weeks during a supervised training, based on patients’ highest tolerable intensity, which was confirmed with stable real-life inspiratory flow measurements using a POWERbreathe KH2 device and associate software.
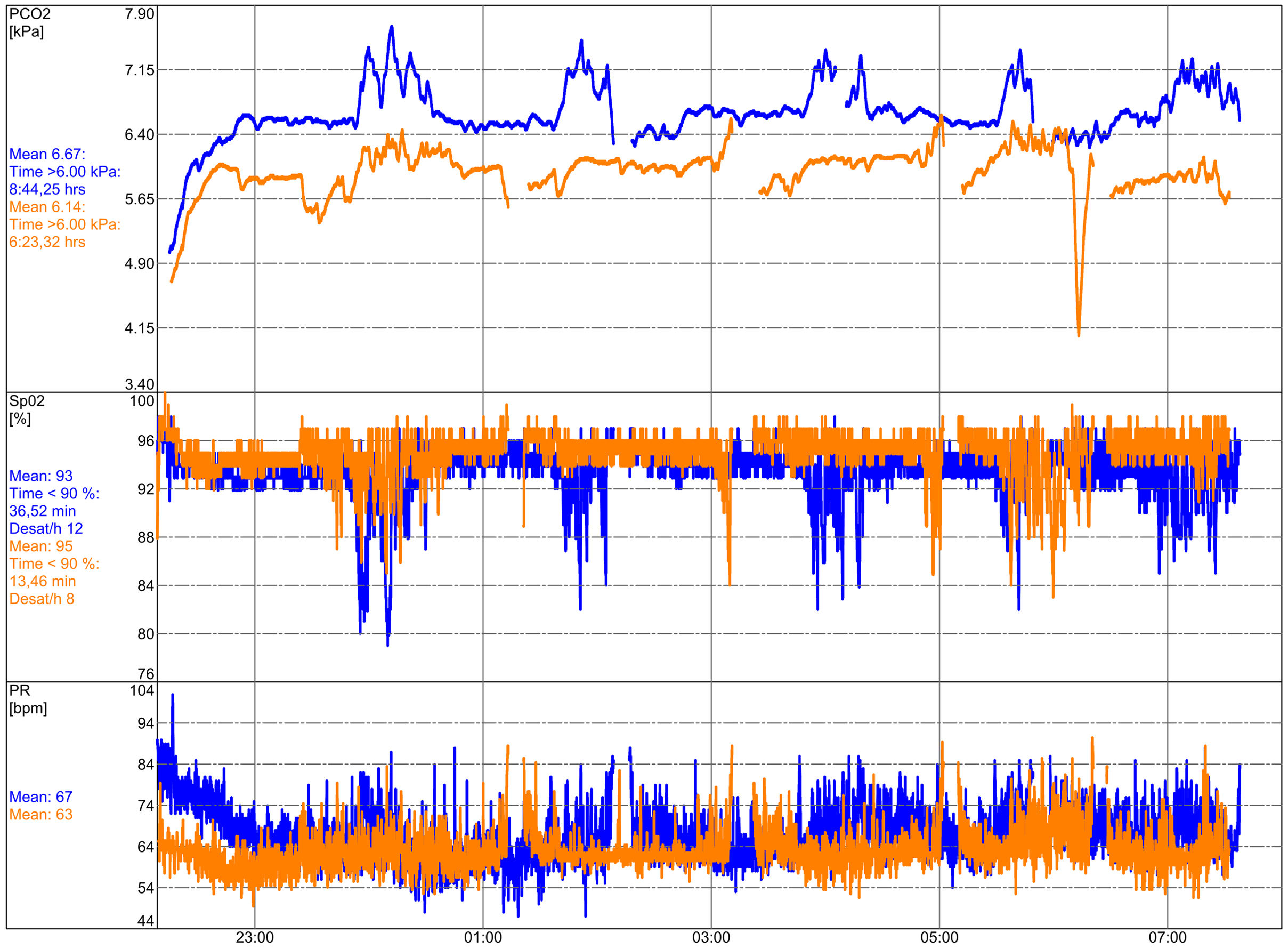
Power and inspiratory endurance capacity of breathing muscles ameliorated significantly. PImax improved with 176% to 47.94cmH2O (52%) and inspiratory endurance capacity increased from 187s. on a resistance of 7cmH2O to 305s. on 19cmH2O. The effects on nocturnal gas-exchange are visualized in Fig. 1. Compared to baseline both oxygenation and ventilation improved. Mean saturation increases from 93% to 95% and hypercapnia decreases from a median PtcCO2 of 6.6kPa (49.5mmHg) to 6.2kPa (46.5mmHg). The four PtcCO2 peaks are lowered, accompanied by less deep desaturations and steady heart rate frequency. Forced vital capacity remained stable with 3.2L. IMT resistance was gradually increased every two weeks as follows: 5-7-12-17-21cmH2O to a maximum of 26cmH2O. He fulfilled all prescribed exercises, which were well tolerated without side effects. Afterwards, he reported improvement in his speech. MRC dyspnoea score improved from 4 to 3 points and health-related quality of life score measured on the Severe Respiratory Insufficiency questionnaire improved from 55 to 61 points.4
Transcutaneous measured nocturnal gas-exchange with SenTec before and after 12 weeks of IMT. Blue colour lines indicate measurement before IMT, orange colour lines after IMT. The top row visualizes PtcCO2 (kPa), the middle row the saturation (%) and the bottom row the pulse rate (PR) in bpm.
Respiratory muscle weakness is the main reason for life-threatening pneumonia and respiratory failure, which are primary causes of death at a mean age of 54 years.5 Current treatment for chronic hypercapnic respiratory failure is HMV, which is a high-burden and expensive treatment with usually a low adherence in DM1.6 To the opposite, IMT is a low-burden therapy with negligible risks, low costs and positive effects in 951 patients with several neuromuscular disorders, although DM1 was not included.2 This case adds to the existing evidence that DM1 can respond favourably to IMT, as well. Especially the benefits on hypercapnia are promising. It warrants further investigations, whether IMT could improve respiration in order to become a complementary treatment with HMV in DM1 patients.
Conflict of interestNone.