Accidental aspiration of sand is an unusual and potentially fatal condition that often occurs in cases of near drowning and accidental burial in sand.
We report the case of a 58-year-old man who accidentally fell into a tank of sand and was buried for more than 5min. On arrival at the emergency room, the patient's Glasgow Coma scale was 7, he appeared cyanotic, and he was gasping. After removing the sand that obstructed the airway, orotracheal intubation was performed which proved difficult due to glottic visualization being impaired by the particulate material.
Once hospitalized, he underwent computed tomography which revealed foreign material in the auditory canals and both outer ears. Radiopaque material was identified in the pharynx, trachea, and right bronchi. The patient was admitted to the intensive care unit with severe hypoxemic respiratory failure that required the delivery of high FiO2 rates (SpO2 95%; FiO2 80%). The respiratory medicine department was urgently consulted and fiberoptic bronchoscopy (FB) was performed, revealing sand in the subsegmental bronchi of the lower right lobe, particularly segment IV, which was entirely occluded. A large amount of sandy material was removed, resulting in patent bronchi, and remarkable clinical improvement was observed, with lower airway pressures and reduced FiO2 requirements that were adapted according to arterial blood gas results. FB was repeated at 48h, revealing signs of diffuse acute bronchitis due to local irritation by sand.
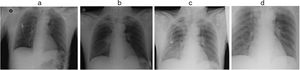
Daily chest X-rays were requested that showed the appearance of perihilar and right basal infiltrate, and later an image of disseminated air bronchogram in the right hemifield not impinging on the peripheral area (Fig. 1). Prophylactic antibiotic therapy with amoxicillin–clavulanic acid was administered for 10 days from the first day of admission, and no pathogenic bacteria were found in the bronchoalveolar lavage. The patient was successfully extubated on day 4 of admission, and was discharged 10 days after the event, without sequelae.
Changes in oxygenation and ventilation after bronchoaspiration of sand occur as a result of laryngospasm, mechanical obstruction, and inflammation caused by chemical irritation.1 After resuscitation and initial stabilization, therapeutic management was initially focused on reducing the burden of sand as far as possible. FB for removal of sand from the tracheobronchial tree was a priority intervention. This prompt action minimized the secondary inflammatory response, and progress was very favorable. Therapeutic bronchoscopic lavage has been previously described in cases of aspiration of sand, with good results.2,3 Removal of material should only be performed when the clinical situation of the patient is compromised by the aspiration. In other situations, efforts to remove aspirated sand in an asymptomatic patient are probably not indicated.3
Airway lesions are a result of a combination of the inevitably traumatic effect of repeated FB manipulation and the local effects of direct epithelial damage from the aspirated sand. The use of systemic corticosteroids as anti-inflammatory agents must be assessed in each individual case, depending on the extent of the local lesions.
Radiographic characteristics after the aspiration of sand are highly variable; the most common abnormality is a confluent spongy nodular image with perihilar distribution, consistent with pulmonary edema. The apex, bases, and lateral lung fields tend to be unaffected, and air bronchograms may be very marked.4
Pneumonia or sinusitis are likely to develop due to the inoculum of infectious pathogens. The benefits of prophylactic antibiotic therapy in this context are not clear.5,6
We believe that, circumstancing permitting, early extubation of these patients could be beneficial to optimize the management of secretions and spontaneous expectoration of secretions mixed with residual sand from the distal bronchial tree. Respiratory physiotherapy was not used as a therapeutic strategy in this patient because it was not considered necessary. Some physical therapy techniques may have theoretical benefits (for example, chest percussion and postural drainage) and should be considered on an individual basis.
In conclusion, massive aspiration of sand and secondary asphyxiation cause a wide variety of clinical, radiological, and bronchoscopic manifestations. Acute respiratory failure may develop as a result of inadequate ventilation if material is occluding the upper airway. Lesions in the bronchioles and alveoli with significant inflammation, acute lung injury or even acute respiratory distress syndrome may later develop. Early aspiration and clearing of the bronchial tree by FB is important to reduce initial ventilatory needs and to avoid injury from local inflammation caused by sand particles.
Please cite this article as: Charco Roca LM, Sánchez Lopez ML, Pazos Crespo JJ, Martinez Villar C, Moreno de la Rosa L, Garcia-de Enterria Ramos I. Asfixia por enterramiento. Arch Bronconeumol. 2019;55:221–222.