Pneumomediastinum is defined as the presence of free air in the mediastinum. This is a rare manifestation and usually presents spontaneously, as a consequence of injury, rupture of a hollow viscus, or gas-producing infection.
It generally occurs in young adults exposed to a sudden change in intrathoracic pressure that results in the rupture of alveolar septa and alveoli, causing air to escape from the pulmonary interstitial tissue to the peribronchiolar and perivascular tissues of the upper mediastinum and the neck. In clinical practice, it is often the result of precipitating factors such as previous muscle exertion (physical exercise, coughing fit, or asthma attack), which lead to a Valsalva maneuver or an increase in intrathoracic pressure. In many cases, it is difficult to differentiate spontaneous pneumomediastinum from more subtle causes of secondary pneumomediastinum, such as esophageal perforation, small tears in the central tracheobronchial tree, or lung or mediastinal infections.1
The most commonly described symptom is central chest pain, which may radiate to both sides of the chest and the neck. Dyspnea and irritative cough may also appear. Dysphagia, hypernasal speech, and tachycardia are less common. The classic triad of spontaneous pneumomediastinum consists of chest pain, dyspnea, and subcutaneous emphysema.2 However, no symptoms associated with compression of the cervical neurovascular bundle (pupillary changes, loss of visual acuity, headache, etc.) have been described in the literature.
We report the case of a patient with a diagnosis of spontaneous pneumomediastinum associated with anisocoria.
This was a 19-year-old man, with no significant clinical history or known toxic habits, who attended the emergency room due to a 12-h history of cervical neck pain associated with central chest discomfort, and a “crackling” sound on palpation of the neck. He reported watery rhinitis in the previous days, and 2 episodes of self-limited vomiting of small amounts of food in the hours prior to presentation in the emergency room. No other symptoms, such as coughing or shortness of breath, were reported. The patient denied a history of trauma in the previous days; he only mentioned that he had resumed his musical activity, playing a wind instrument (cornet).
Of note on examination was subcutaneous emphysema in the cervical spine and both supraclavicular fossa. No changes were observed in voice tone and there was no dysphagia. A neurological examination detected significant normoreactive anisocoria (left pupil smaller than the right), with no changes in visual acuity or ptosis.
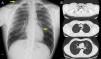
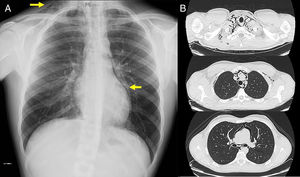
Complete blood count with serum proteins were normal. Serum biochemistry showed vitamin B12 levels of 172.1pg/ml. Chest radiograph on admission (Fig. 1A) showed an area of left paracardiac hyperlucency, consistent with pneumomediastinum. A chest computed tomography (CT) was performed to confirm the diagnosis and to complete the study.
(A) Chest X-ray, showing (arrows) signs of subcutaneous emphysema the right laterocervical region and an area of left paracardiac hyperlucency, suggestive of pneumomediastinum. (B) Chest CT (parenchymal window) showing extensive pneumomediastinum in several regions, dissecting the mediastinal structures.
On computed tomography (Fig. 1B), the most significant findings were a large pneumomediastinum that dissected the mediastinal structures and extended along the left oblique fissure. It was also accompanied by subcutaneous emphysema in both laterocervical regions, the supraclavicular fossa (predominantly in the left side), and both axillary regions. Neither pneumothorax nor rib fractures were observed.
Given the patient's stable status, he was admitted to the general hospital ward, under the care of the pulmonology staff. A clinical judgment of spontaneous pneumomediastinum was made, although the contribution of factors associated with Valsalva maneuvers or barotrauma could not be ruled out. Conservative treatment was administered, with oxygen therapy, rest, and analgesia.
During the hospital stay, evaluation by the neurologist was requested, since anisocoria is not described in the literature as a symptom associated with pneumomediastinum (except in cases of cervical spine injuries in which the sympathetic nervous system is affected).3 The neurological study was completed with head CT, cranial artery angio-MRI (circle of Willis), and echo-Doppler of the supra-aortic trunks, all of which were normal. We concluded that the anisocoria was associated with altered sympathetic and vagal modulation in the setting of pneumomediastinum with secondary compression of nerve structures by associated subcutaneous emphysema.
The patient was also assessed by hospital's ENT specialist, and no changes were found on fiberoptic naso-laryngoscope.
The patient was discharged 7 days after admission, with a chest X-ray showing no signs of pneumomediastinum and full reabsorption of subcutaneous emphysema. Anisocoria resolved progressively during the stay.
The course of spontaneous pneumomediastinum is benign in most cases, and observation and conservative treatment are sufficient for recovery.4 The risk of recurrence is very low. Secondary causes that, if not promptly diagnosed, might occasion an unfavorable clinical course should be excluded,5 including cervical spine injuries and/or contusions, vascular aneurysms, and esophageal perforation. Diagnosis requires a high level of suspicion, given the scant or unclear clinical manifestations; up to one third of patients do not present any precipitating factor, and subtle changes in the chest X-ray may go unnoticed. Given our experience, it may also be of interest to evaluate concomitant neurological changes. Though not reported in the literature, these may contribute to the differential diagnosis of this entity, and moreover, require a full assessment to rule out more severe clinical syndromes that can compromise the cervical sympathetic nervous system.
Please cite this article as: López LL, Bueno AR, Kubarsepp A. Anisocoria como síntoma asociado a neumomediastino espontáneo. Arch Bronconeumol. 2018;54:437–439.