Lung cancer involving the heart is rare. It is associated with a poor prognosis and often not detected until autopsy. Very few cases have been published describing lung cancer with intracardiac metastasis. We report the case of a patient with cardiac metastases at the time of diagnosis.
A 43-year-old man, smoker with an accumulated consumption of 30 pack-years, occasional drinker, with no other clinical history of interest. He presented in the emergency room with a 3-month history of cough, expectoration of mucus, dysphonia, and weight loss, asthenia and anorexia. Examination was unremarkable, and the patient was in good general condition. Blood tests were performed, revealing platelets 580,000/mm3, hemoglobin 12g/dl, leukocytes 12,000/mm3 and C-reactive protein 10. Chest radiograph showed a mass in the right upper lobe with generalized cardiomegaly. Electrocardiogram showed sinus tachycardia. In view of these findings, we decided to extend the evaluation, as follows:
- –
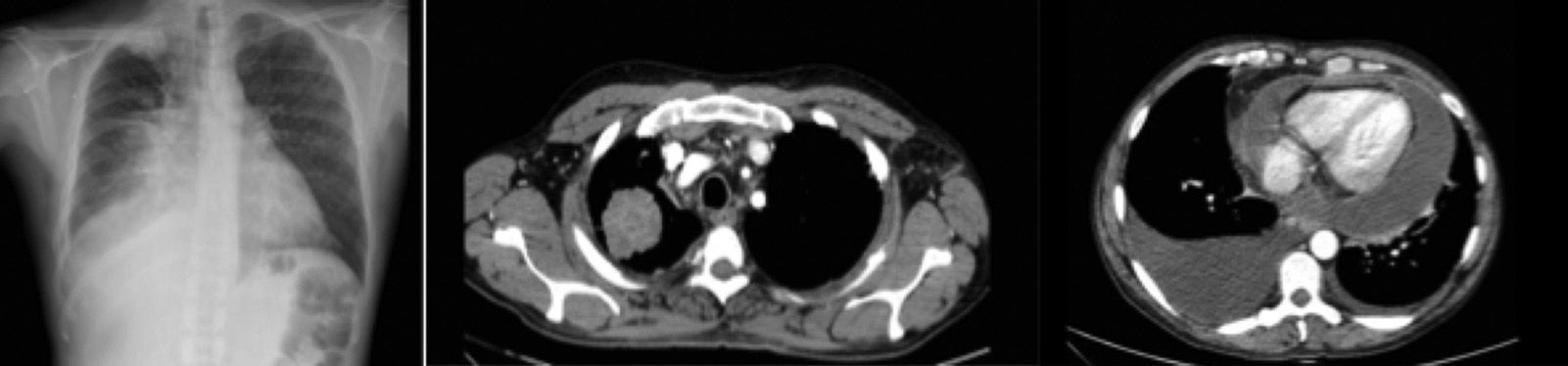
Computed tomography (CT): a mass measuring >5cm was found, with lobulated borders and spiculated margins in ample contact with the apical segment of the right upper lobe, another mass measuring 2.5cm in the apical segment in contact with the mediastinal pleura, obstructing segment 3 with distal pneumonitis. Multiple bilateral pulmonary nodules, mediastinal lymphadenopathies measuring >1cm in the supraclavicular regions on both sides in all mediastinal spaces. Significant pericardial effusion with diffuse pericardial thickening. Significant right and mild left pleural effusion. Hypodense hepatic lesion measuring >2cm in segment IV. Nodular thickening of the left adrenal gland and a lytic bone lesion in the D8 vertebra, suggestive of metastasis. Conclusion: pulmonary masses consistent with synchronous neoplasms. Stage IV (Fig. 1).
- –
Echocardiography: a predominantly posterior, large pericardial effusion was revealed with minimal evidence of hemodynamic involvement. Several mobile multilobulated masses, measuring several centimeters, were observed adhering to the anterior, lateral and posterior areas of the visceral pericardium. An echogenic image measuring around 15×9mm was observed within the inferior aspect of the myocardium, consistent with metastatic implant.
A diagnostic thoracocentesis was performed, the results of which were inconclusive. During the bronchoscopy, the patient had an episode of hypotension, so the test was suspended. Diagnosis was obtained from a CT-guided fine-needle aspiration and biopsy (FNAB) with results consistent with the diagnosis of lung adenocarcinoma. EGFR and ALK mutation cytologies were requested, reported as “mutation absent” and “no translocation”, respectively.
On admission, a pericardiocentesis was proposed to prevent possible cardiac tamponade, but in view of the patient's hemodynamic instability, we decided to start treatment with corticosteroids, leading to clinical improvement confirmed in subsequent monitoring. The patient was referred to medical oncology to start chemotherapy.
Any malignant tumor can metastasize to the heart. Although primary cardiac tumors are rare, secondary involvement from a primary tumor is not so uncommon, and carries a poor prognosis. Some studies have reported a higher incidence than expected, ranging between 2.3% and 18.3%.1 Bussanni et al.2 performed 18,751 autopsies, including 7289 cancer patients, of whom 9.1% had cardiac involvement. The most common primary tumor is mesothelioma (48%), followed by melanoma (27.8%) and lung adenocarcinoma (21%). Lymph node propagation is considered the most common,3 although hematological dissemination and, to a lesser extent, direct extension have also been described.
Clinical presentation is very variable, depending on the metastatic site, and it is generally asymptomatic, but on occasions it can manifest as dyspnea, cough or chest pain,4 or even pericardial tamponade. Management of pericardial effusion depends on the type of underlying primary tumor.5 In the case of lung tumors, some guidelines5 propose that the best therapeutic option for resolution is the combination of systemic and intrapericardial chemotherapy.
This case demonstrates a rare intracardiac metastatic manifestation of lung cancer, conferring a very poor disease prognosis. Cardiac metastases must be considered in the differential diagnosis of heart disease in a patient with lung cancer.
The authors thank the Respiratory Medicine Department of the Hospital Universitario Virgen de la Victoria.
Please cite this article as: Cabrera César E, Fernández Aguirre MC, Hidalgo Sanjuan MV. Metástasis cardiacas de una neoplasia pulmonar. Arch Bronconeumol. 2017;53:80–81.