Adenocarcinoma of the lung occasionally presents with atypical clinical and radiological manifestations. We report a clinical case with an unusual radiological presentation, and review the diagnostic and therapeutic developments that we believe are of interest to the clinical pulmonologist.
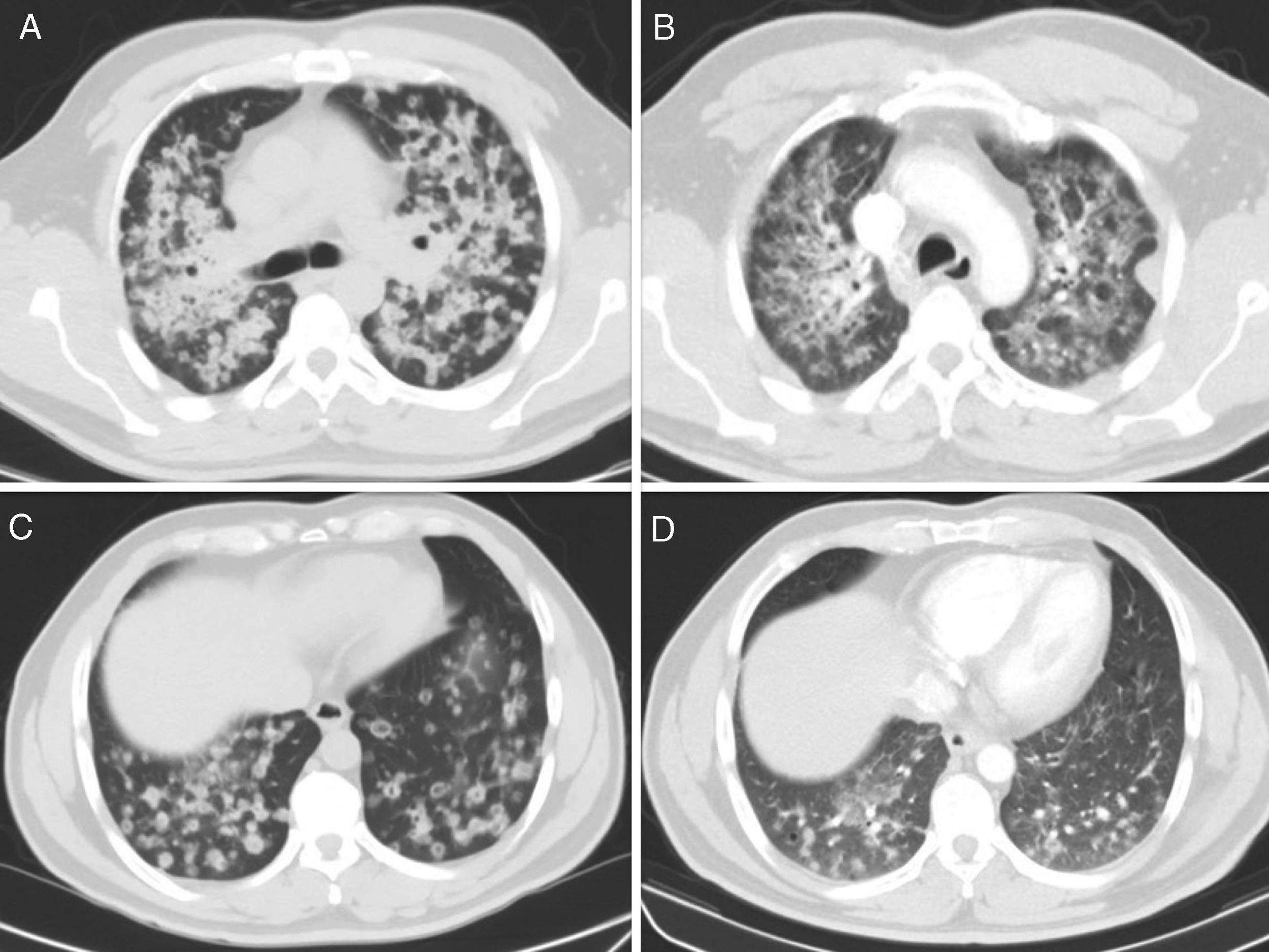
Our patient was a 49-year-old man, originally from Ecuador, non-smoker, with no significant personal history and no known contact with patients with active tuberculosis. He consulted due to a 10-month history of chronic productive cough, mucopurulent, occasionally with bloody sputum, in addition to intense hyporexia and a 3kg weight loss. Chest X-ray showed bilateral pulmonary infiltrates with some poorly defined, pseudonodular images, predominantly in the upper lobes. He was hospitalized in a respiratory isolation room with an initial suspicion of tuberculosis, but sputum smears were negative. After multiple bilateral pulmonary nodular opacities, mostly cavitary, were seen on the chest computed tomography (CT) (Fig. 1A and C), a thorough, bilateral bronchoscopy was performed that showed no pathological findings. A cytological study of the bronchoalveolar lavage samples was conducted, yielding a diagnosis of lung adenocarcinoma with micropapillary pattern. The exon 19 deletion was positive, while the rest of the mutations studied were negative (L858R, T790M, G719A/C/S, exon 20, S768I and L861Q, ALK and ROS1). The patient began treatment with gefitinib, with a good clinical and radiological response at 4 months (Fig. 1 B and D).
Adenocarcinoma is the most frequent histological type of lung cancer. In 2011, a new, much-needed classification of adenocarcinoma addressing the different patterns and their various prognoses and management was published after a consensus was reached among pulmonologists, thoracic surgeons, oncologists, pathologists, molecular biologists, and radiologists.1 This classification has been updated over the years to include genetic and molecular biology data. Two groups were differentiated in the latest revision of the lung adenocarcinoma classification in 2015: preinvasive lesions (atypical adenomatous hyperplasia and adenocarcinoma in situ) and invasive lesions (minimally invasive adenocarcinoma and invasive adenocarcinoma).2,3
The spectrum of radiological manifestations of adenocarcinoma of the lung is very variable, ranging from subsolid or solid lesions to consolidations and masses that are usually closely correlated with histology and prognosis, hence the importance of the role of the radiologist. A determining factor in the detection and characterization of lung nodules has been the use of high-resolution multidetector CT instead of the conventional helical CT (with thicker collimation).4
Invasive adenocarcinoma represents 70% of resected lung adenocarcinomas and is defined by the presence of an invasive component greater than 5mm. Histologically, these masses tend to be heterogeneous, with mixed patterns (acinar, papillary, micropapillary, lepidic, and solid), and are given the name of the predominant component. Some subtypes are associated with a specific prognosis. For example, adenocarcinoma with a predominant lepidic component has a better prognosis. In contrast, the presence of a micropapillary component predicts worse survival. For this reason, adenocarcinoma with this pattern has aroused much interest lately, especially due to its high rates of recurrence and metastasis. It is more common in men and non-smokers, and more frequently associated with lymphatic and pleural invasion and lymphadenopathies than other histological subtypes.
Typical radiographic findings in invasive adenocarcinomas are solid or mixed nodular lesions (with part solid component, part ground glass), while purely ground glass nodules are less common. In addition, it is quite important to quantify the size of the solid component, since if it is greater than 9mm, a diagnosis of invasive adenocarcinoma is 100% specific, while a size of 3–5mm makes it less likely. This concept seems to be gaining importance, and future classifications will focus more on the size of the solid component than the overall size of the nodule as a criterion for staging the T of the TNM.5,6 Another consideration when differentiating preinvasive lesions from invasive lesions is the cross-sectional diameter of the nodule in the lung window.4,6
With regard to treatment, recent advances are facilitating a more specific approach. These developments have been led by a group of drugs that target the epidermal growth factor receptor (EGFR), generically known as tyrosine kinase inhibitors. They include erlotinib and gefitinib for first-line treatment, and afatinib in second line when the former fail or after relapse. We now know patients with a mutation in the EGFR gene activator (exon 19 deletion or L858R replacement) are most likely to respond well to these drugs.7
Our case is unusual due to the uncommon radiological presentation. Accordingly, we believe that lung adenocarcinoma should be included in the differential diagnosis of this radiological pattern.
Please cite this article as: Montes Ruiz-Cabello M, Guirao Arrabal E, Gallardo Medina M, Vinuesa García D. Presentación radiológica atípica de un adenocarcinoma de pulmón. Arch Bronconeumol. 2019;55:160–162.