Surgery is the treatment of choice for tracheal stenosis. In patients unfit for surgery, endoscopic treatment is a valid alternative, providing relief from dyspnea and improvement of quality of life.
Combined endoscopic management includes radial incision of stenotic scar with laser or cold instruments, mechanical dilatation and stent placement in presence of tracheal ring fracture to prevent recurrence.1
Shapshay et al.2 pioneered endoscopic dilatation in 1987, using a CO2 laser in patients with tracheal stenosis. Following this, use of the technique has increased, and is now standard in most hospitals.
CO2 and ND:YAG lasers are generally used in the management of tracheal stenosis. The CO2 laser is a highly accurate cutting tool with causing scant thermal damage, but its main drawback is the difficulty of delivering the beam through the bronchoscope. The ND:YAG laser is easily used with a bronchoscope, but it is less precise and may cause surrounding thermal damage.
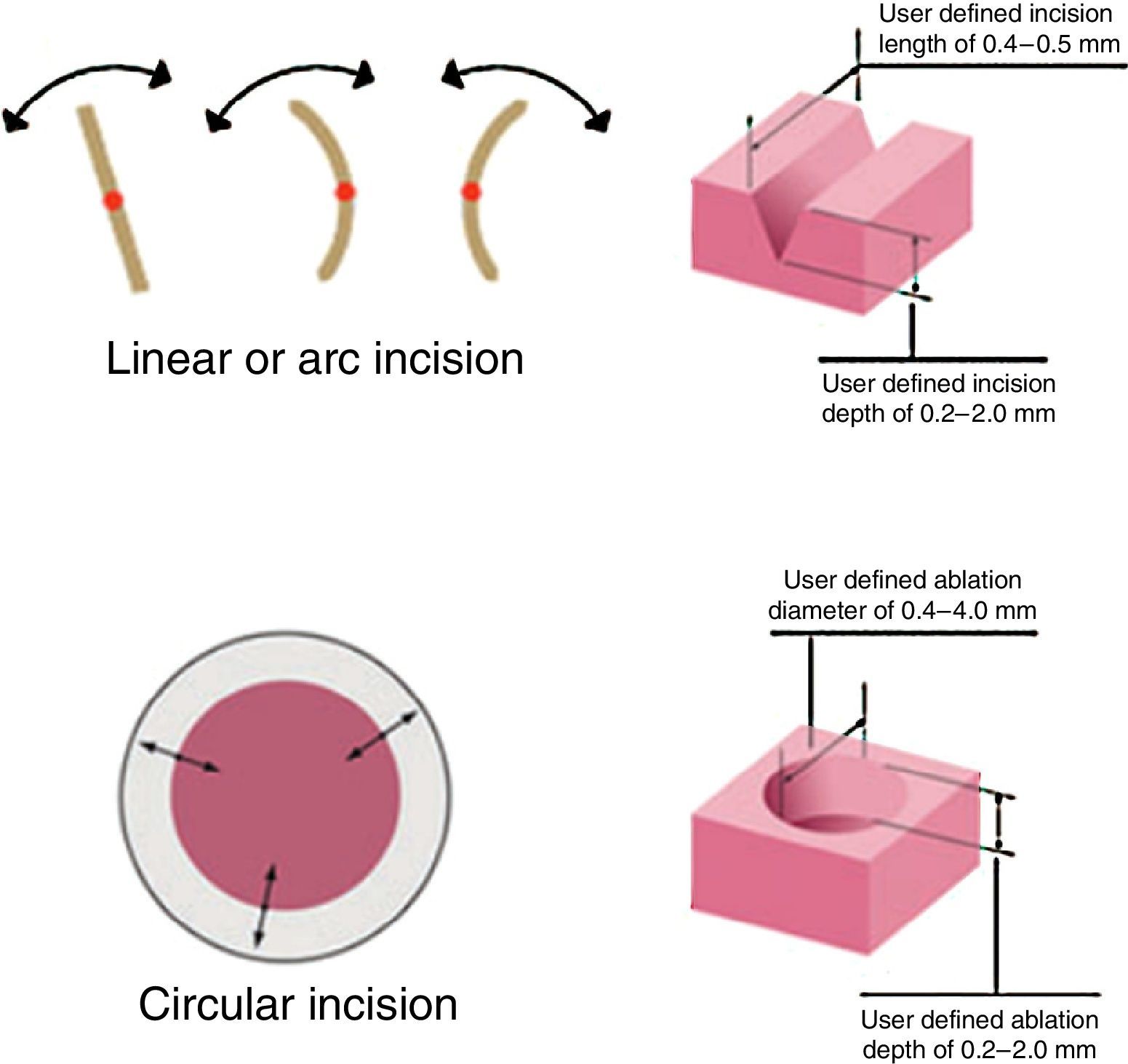
Digital Acublade Robotic Microsurgery Laser System (Lumenis© Surgery) is a new generation of CO2 laser commonly used in phonomicrosurgery. The main advantages of AcuBlade compared to traditional CO2 are the possibility of setting the type of incision (straight, curved, or disk ablation; Fig. 1), the minimal thermal damage, and the computer filtering that eliminates the operator's tremor without preventing its ability to guide the laser in the target zone.3,4 Thus, resection with AcuBlade is as even as that achieved with cold instruments, but with the advantage of a bloodless operative field.
We used AcuBlade for the first time in the management of idiopathic subglottic stenosis in a 73-year-old female. The stenosis appeared as a circumferential fibrotic web-like lesion, lying 8mm from vocal folds, with a length of 15mm and airway lumen of 6mm.
With AcuBlade, we achieved an even resection of the stenotic scar without injuring the tracheal epithelium, and restored the normal tracheal lumen. Thus, we decided against mechanical dilatation to avoid tracheal injury and against stent placement due to proximity to vocal folds. At 15-month follow-up, the patient was asymptomatic with normal spirometric values and a patent tracheal lumen.
In the light of this experience, we used AcuBlade in another challenging case involving management of granulations complicating subglottic stent placement.5 The lesions completely destroyed vocal folds with luminal stent obstruction. AcuBlade was able to create a precise haemostatic excision of granulations without injuring vocal folds. It allowed us to assure airway patency while avoiding other treatments such as arytenoidectomy or cordectomy with adverse effect on phonatry function.
Finally, AcuBlade may be a useful tool in the armamentarium of the interventional bronchoscopist. Compared to traditional lasers, it gives a highly uniform, hemostatic incision with minimal thermal spread. In addition, the type of incision can be adapted to the shape of lesion.
Please cite this article as: Fiorelli A, Mazzone S, Santini M. Sistema láser AcuBlade®: una nueva herramienta para el broncoscopista intervencionista. Arch Bronconeumol. 2016;52:283–284.