A 50-year-old woman, non-smoker, with a clinical history of psoriatic arthritis only. A chest X-ray was performed before starting treatment with methotrexate. Physical examination and clinical laboratory tests were normal.
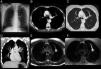
The chest X-ray (Fig. 1A) revealed a water attenuation pseudonodular mass with well-defined margins in the parahilar region of the left upper lobe, which appeared to be a pulmonary nodule. Multidetector computed tomography (CT) confirmed the presence of a well-defined nodular lesion, extending in the form of a bifurcated tubular structure, not enhanced after the administration of intravenous contrast medium. Distal parenchyma showed air trapping (Fig. 1B–D). On magnetic resonance imaging (MRI), the morphology of the lesion was similar to the CT image: hyperintense in T1 and T2-weighted sequences (Fig. 1E and F), suggestive of bronchocele. Both CT and MRI confirm the diagnosis of bronchial atresia.
(A) Posterior–anterior chest X-ray. (B and C) Chest computed tomography with intravenous contrast medium, axial slice at the level of the aortopulmonary window in a mediastinum and lung window, respectively. (D) Multidetector CT coronal reconstruction in maximum intensity projection (MIP) mediastinum window. (E and F) Chest magnetic resonance image, axial slices at level of aortopulmonary window. T2 and T1-weighted axial slices with fat suppression.
Bronchial atresia is a congenital defect characterized by obliteration of the proximal section of a lobar, segmentary, or subsegmentary bronchus, with no clear cause. If mucus accumulates in the dilated distal bronchus, bronchocele occurs. It is detected incidentally in adults and should be taken into account in the differential diagnosis of solitary pulmonary nodule.1,2 It can be diagnosed using multidetector CT and MRI techniques.
Please cite this article as: Fernandez Rodriguez L, Fernandez-Velilla M, Torres Sanchez I. Caso de atresia bronquial. Arch Bronconeumol. 2016;52:103.