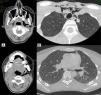
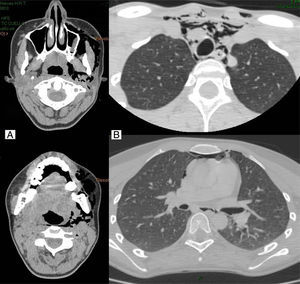
A 22-year-old woman presented in the emergency department with difficulty breathing and swallowing, and pain in the left hemithorax, 2h after two molars were extracted. On physical examination, no changes were seen in the oropharyngeal region, apart from the missing two upper left molars, and no evidence was seen of upper airway compromise. However, crepitation on palpation of the neck and upper chest region were of interest. All vital signs were stable. Computed tomography was performed of the face, cervical spine and chest, revealing pneumomediastinum, involving the upper and anterior mediastinum and subcutaneous emphysema of the neck and face, dissecting even in the deepest cervical planes (Fig. 1). The patient was treated with metamizole and antibiotic prophylaxis with amoxicillin–clavulanic acid. She was discharged 48h later, and attended a follow-up visit in the thoracic surgery department two weeks later, confirming complete resolution of the process.
(A) Subcutaneous emphysema extending to the cervical–facial region, dissecting even in the deepest cervical planes (pterygoid fossa and the submandibular, masticatory, retropharyngeal, parapharyngeal, and left carotid spaces) and (B) pneumomediastinum extending toward the upper (surrounding the trachea, supraaortic trunks, and adjacent structures) and anterior (in front of the pericardium and the outlets of the great vessels).
The appearance of pneumomediastinum and massive subcutaneous emphysema associated with dental extraction is very rare, and few cases have been documented. It is generally self-limiting and not life-threatening, but on rare occasions it can progress to tension pneumothorax, mediastinitis or gas embolism. Antibiotic prophylaxis is indicated, particularly in the presence of underlying respiratory diseases or dental infections.1
Conflict of interestsThe authors declare that they have no conflict of interests.
Please cite this article as: Vera MRM, Rosales RL, González AS. Neumomediastino y enfisema subcutáneo secundarios a extraccióndental. Una complicación poco frecuente. Arch Bronconeumol. 2016;52:104–105.