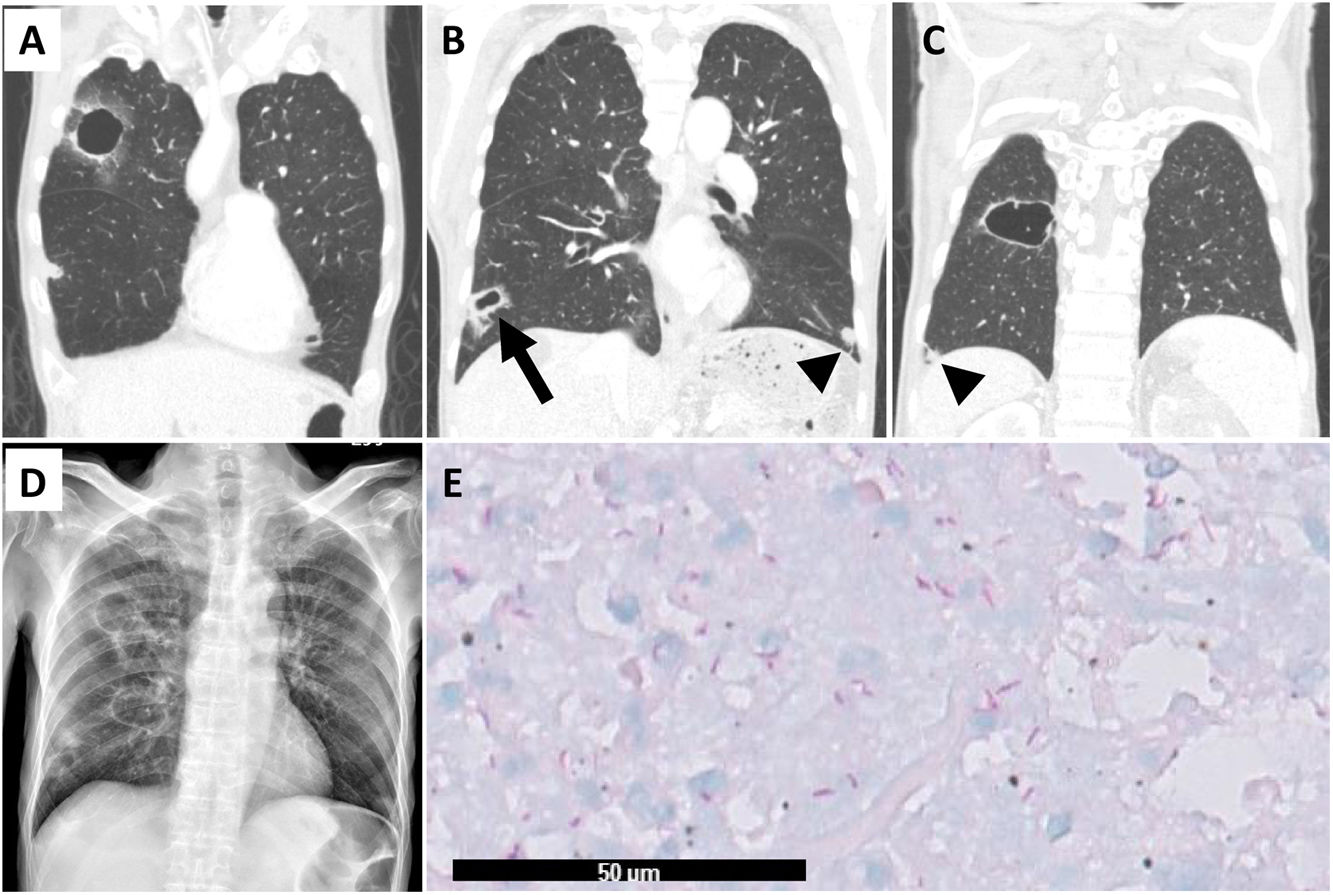
A 58-year-old man had renal cell carcinoma with liver metastases and started pembrolizumab, a programmed death-1 immune checkpoint inhibitor, plus axitinib. Six months later, after 8 doses of pembrolizumab, he developed productive cough. A chest radiography and computed tomography disclosed multiple cavitary lesions formation in right upper and right lower lobes without change in size of pre-existing nodules (Fig. 1A–D). The sputa were smear-positive for acid-fast bacilli and culture-positive for nontuberculous mycobacteria (NTM) isolates, which were identified as Mycobacterium avium complex (MAC) through genotyping method.
(A–C) The computed tomography revealed newly developed cavitary lesions in right upper and right lower lobes and pre-existing unchanged nodules (arrowheads). (D) The chest radiography showed corresponding cavitary lesions in right lung field. (E) The histopathologic finding in the wedged lung tissue (arrow in B) was extensive tissue necrosis with the presence of numerous acid-fast bacilli but no granuloma.
He received a thoracoscopic wedge resection for cavitary lesion in right lower lobe to rule out lung metastasis. The histopathologic findings were acute and chronic inflammation with necrosis and the presence of acid-fast bacilli without granuloma (Fig. 1E). A diagnosis of cavitary MAC-pulmonary disease (PD) was made. He initiated antibiotics treatment but discontinued 4 months later due to intolerance and drug-drug interaction. His sputa remained culture-positive for MAC.
Immunotherapies using immune-checkpoint inhibitors have improved outcomes in patients with cancers. However, a drug monitoring survey and case series reported development of NTM-PD after immunotherapy.1,2 Although the impact of immunotherapy on mycobacterial infection remains uncertain, physicians should be aware of NTM-PD in patients receiving immunotherapy.
Conflicts of interestThe authors do not have any conflicts of interest.