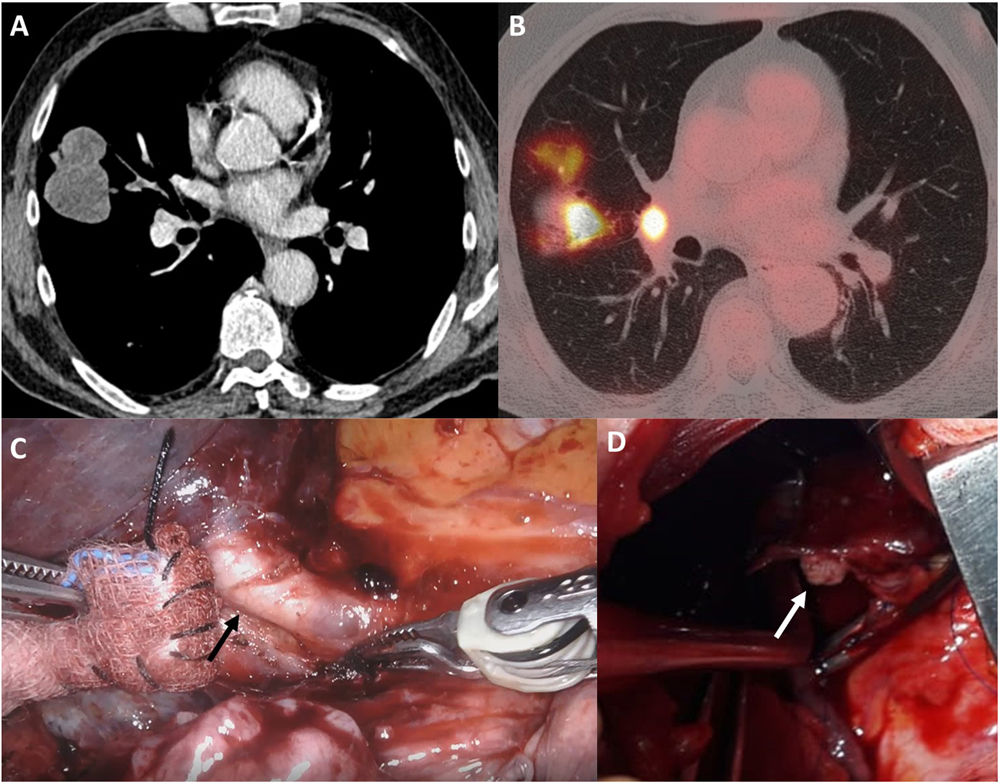
We report the case of a 68-year-old patient with a history of acute myeloblastic leukemia and acute myocardial infarction who presented with a mass in the middle lobe (Fig. 1A) that was hyperdense on PET, and interlobar lymphadenopathy suggestive of malignancy (Fig. 1B). After ruling out N2 involvement, a robotic middle lobectomy was planned and performed 2 months after the diagnostic CT scan. During the procedure, a tumor thrombus, unsuspected before the procedure, was observed in the middle lobe vein 10–12mm from the atrium (Fig. 1C), so extrapericardial proximal clamping and manual suture of the vein were performed (Fig. 1D) after conversion to thoracotomy. The pathological diagnosis was pleomorphic carcinoma (pT3N1M0).
Chest CT image showing a hypodense lobulated mass measuring 6.1cm×5.8cm×4.4cm (transverse, anteroposterior, craniocaudal) located predominantly at the periphery of the middle lobe in contact with the costal pleura, the horizontal fissure, and the oblique fissure. Central extension, forming a partly endobronchial obstruction of the lateral segmental bronchus of the middle lobe and subsegmental bronchi and a medial interlobar lymphadenopathy to the mass measuring 1.2cm were observed (A). PET/CT image showing a hypermetabolic mass in the middle lobe with SUVmax 19.51 and focal uptake of FDG in the right hilar region, and lymphadenopathy with SUVmax 13.36 (B). Intraoperative image during the robotic approach revealing the presence of an intravascular tumor extension at the mid-lobe vein (arrow) level (C). Intraoperative image during the open approach (thoracotomy without muscle section) showing the presence of tumor in distal margin (arrow) and clamp in proximal margin of the middle lobe vein after vessel section (D).
Histopathological evidence of intravascular tumors extending into pulmonary veins has been reported in 0.7% of lung cancer patients.1 Its presence significantly worsens prognosis and has a significant impact on therapeutic management.2
The use of the latest imaging technologies (3D vision and high resolution) in endoscopic surgical procedures (VATS and robotics) improves quality and precision, revealing details that assist in the identification of this type of lesion.
FundingNone.
Conflict of interestsThe authors declare that they have no conflict of interests directly or indirectly related with the contents of this manuscript.