Journal Information
Vol. 61. Issue 4.
Pages 229-231 (April 2025)
Share
Download PDF
More article options
Vol. 61. Issue 4.
Pages 229-231 (April 2025)
Scientific Letter
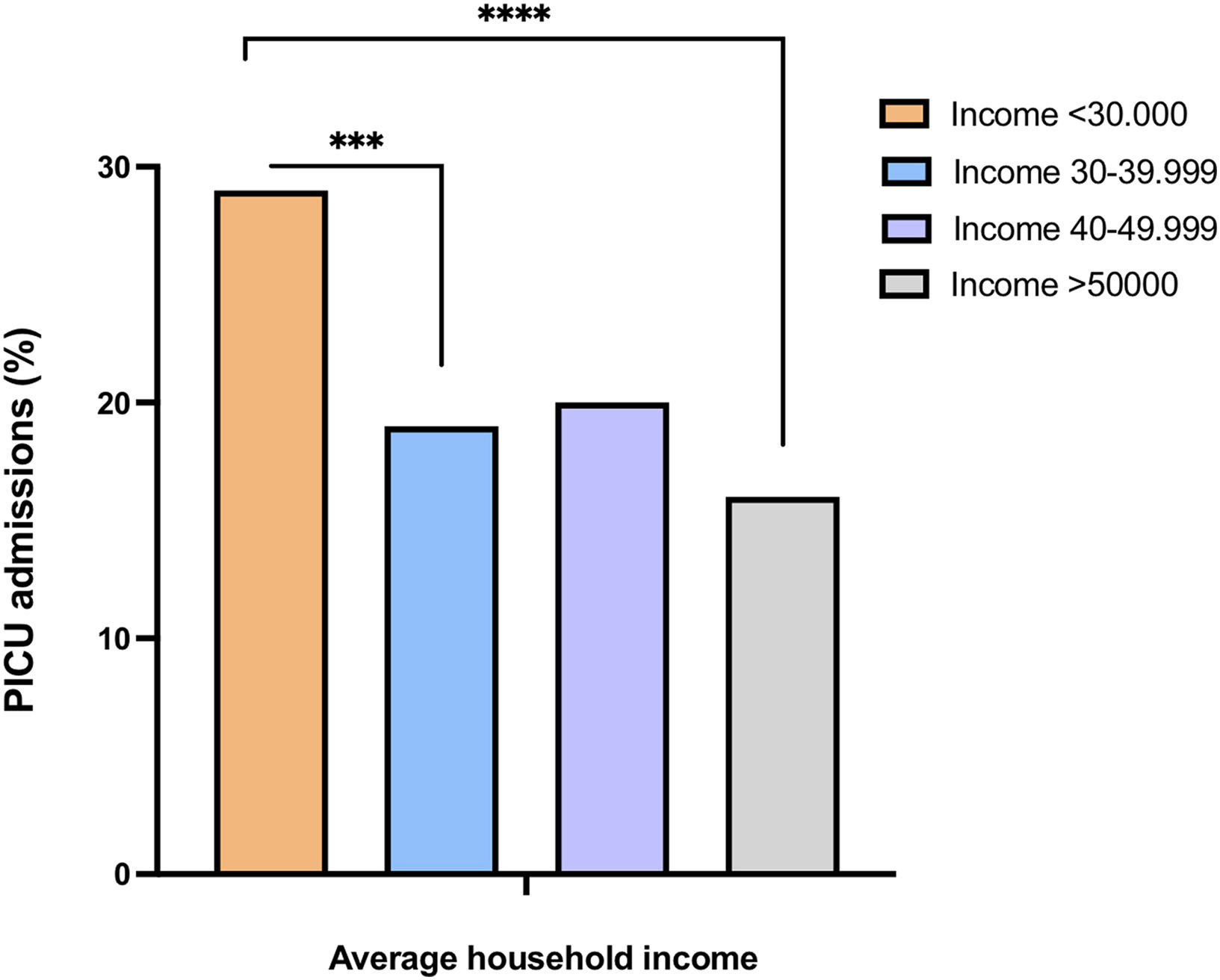
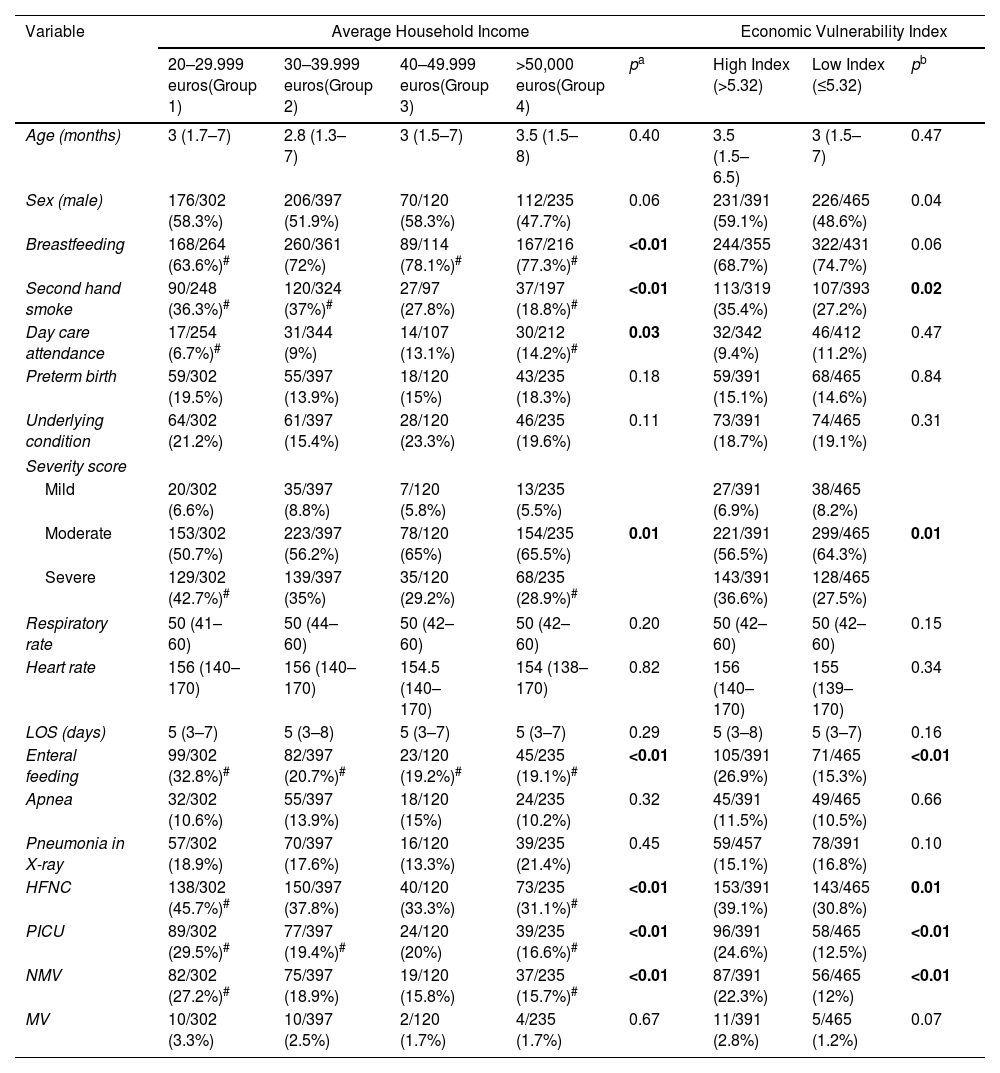
The Importance of ZIP Code-related Average Household Income on the Severity of Respiratory Syncytial Virus Infection in Infants
Visits
465
This item has received
Article information
These are the options to access the full texts of the publication Archivos de Bronconeumología