Female, 72 year-old, non-smoker, autonomous, with a 5-year history of exposure to birds and known diagnoses of asthma, essential hypertension, dyslipidemia, and type 2 diabetes. She was hospitalized for moderate SARS-CoV2 infection, 2 years ago.
She presented with worsening fatigue and dyspnea for 2 years. Imaging exams showed ground-glass reticular densification, traction bronchiectasis and “honeycomb”. Functionally, she presented moderated restriction and DLCO of 48% (ERS/ATS 2021). The echocardiogram showed PSAP 41mmHg without other alterations. Chronic interstitial pneumonia was suspected and cryobiopsy was requested.
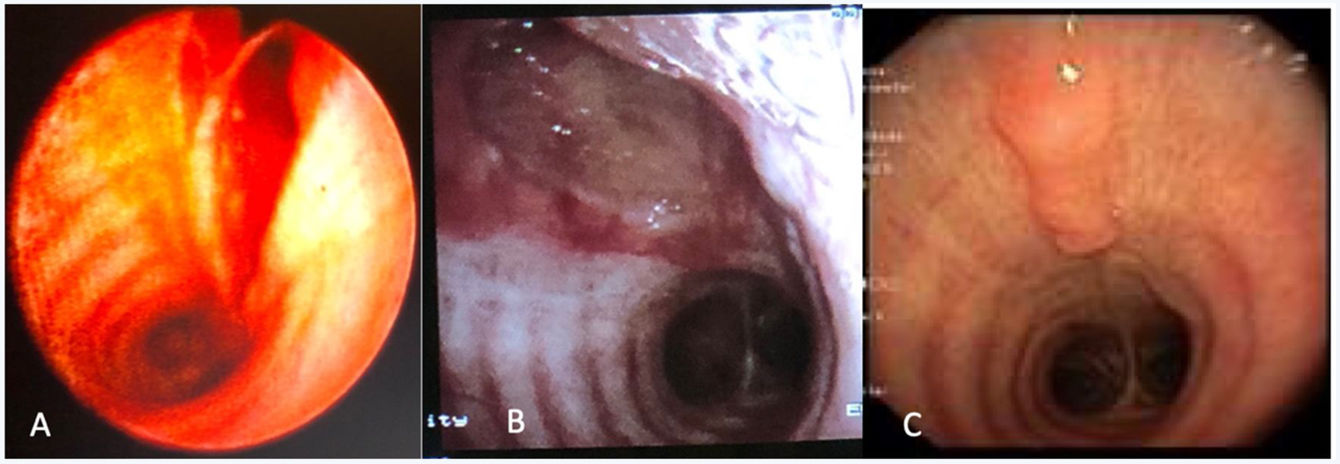
The cryobiopsy was performed under general anesthesia with placement of an endotracheal tube (ETT). After the procedure, residual but persistent bleeding was identified, and bronchofibroscopy revealed a 3cm longitudinal tear in the posterior wall of the trachea, up to the submucosa (Fig. 1A).
The patient was admitted to the Intensive Care for clinical and imaging surveillance, with no evidence of pneumomediastinum, pneumothorax or subcutaneous emphysema. Conservative therapy was chosen (monitoring). Endoscopic reassessment after 4 days showed a laceration on the posterior wall of the trachea with signs of flap healing (Fig. 1B). The injury was classified as grade I according to Cardillo et al.1 She was discharged after 4 days, with indication for monitoring. Endoscopic reassessment after 1 month showed complete healing of the tear, without interruption of continuity (Fig. 1C).
The pathology of the cryobiopsy suggested chronic hypersensitivity pneumonitis.
Iatrogenic injuries of the trachea and main bronchi (IIT) are complications associated with invasive medical–surgical procedures, especially orotracheal intubation or percutaneous tracheostomy, which are defined as post-intubation IIT.1,2
The epidemiology is unknown, presumably underdiagnosed extremely rare, with most publications being of isolated cases or small series with few patients.2–4 Known risk factors for IIT include advanced age, women, obesity, anatomical variations, multiple intubation attempts, rigid guidance and incorrect ETT size.1,2,4 Clinical presentation can be variable, ranging from asymptomatic to subcutaneous emphysema, pneumothorax, pneumomediastinum and acute respiratory failure.1,2
Imaging exams (CT with IV or double contrast) and endoscopic exams (gold standard) are essential to assess the size of the lesion, and the involvement of other organs.2 Based on the extent of the lesion, in 2010 Cardillo et al. (revised in 2022) proposed a morphological classification for risk stratification.1
IIT has significant morbi-mortality rates, requiring early diagnosis and effective treatment, followed by close monitoring. There are no guidelines for the treatment, which must be individualized.3,5
Traditionally, surgical treatment has been the gold standard (especially in symptomatic patients with IIT grade IIIa to IV, or any lesion with mediastinitis).1,4 However, less invasive options are increasingly being considered, such as endoscopic treatment (stenting over the tear) or conservative treatment.1,4 Conservative treatment consists of a multiplicity of options – observation, intubation, tracheostomy, and fibrin glue. Initially proposed for asymptomatic IIT grade I lesions, its indications are being extended to wider and deeper tears (up to 9cm or IIIa).1,4
The current evidence is non-consensual on the approach, even within the conservative aspect, with a variety of choices. It is therefore essential to create joint guidelines for the treatment of these injuries.
FundingThis article had no funding sources.
Conflict of interestNone.