The high transmissibility and lack of specific treatment for coronavirus disease-2019 (Covid-19) has prompted the authorities of most countries to impose temporary lockdowns on their populations to contain the spread of the disease.1,2 The potential health consequences of home confinement in this setting are not well characterized.3 Home continuous positive pressure ventilation (CPAP) is the treatment of choice for patients with obstructive sleep apnea (OSA)4 although its effectiveness depends largely on therapeutic compliance.5 In this study, it was suggested that difficulties in accessing the healthcare system and the anxiety produced by the situation could have a negative impact on adherence to treatment. Given its known cardiovascular implications, OSA has been proposed as a risk factor for a negative outcome in Covid-19.6
The main objective of the study was to compare the degree of compliance and adherence during lockdown in OSA patients previously included in a CPAP home monitoring program, compared with compliance during the previous 3 months, analyzing the influence of sex, age, and severity of OSA.
Patients diagnosed with OSA treated with CPAP (AirSense 10, ResMed) participating in a telemonitoring program were included in the study. Two study periods were defined: 1) baseline, from December 15, 2019 to March 14, 2020; and 2) follow-up during the first month of lockdown, from March 15 to April 14, 2020. Patients had to have been receiving treatment for more than 3 months at baseline to avoid any learning bias. The protocol was approved by the Ethics Committee (CEIC PI090-20).
CPAP telemonitoring data were received and stored automatically on the MyOSA web platform (Oxigen Salud, Barcelona, Spain), from which the following variables could be estimated: 1) daily use (number of hours divided by number of calendar days); 2) relative use (number of hours divided by days of use); 3) percentage of nights of use; 4) percentage of nights of use >4h; 5) residual apnea-hypopnea index; 6) residual central apnea index; 7) residual obstructive apnea index; 8) mask leaks; and 9) 95% percentile of leaks. The criterion for adherence was use of CPAP for more than 4h on 70% of nights.7
Statistical differences between the study periods (baseline before lockdown vs. follow-up during lockdown) were analyzed using the Wilcoxon signed-rank test for paired samples. The threshold for statistical significance was set at a p value of <0.01.
A total of 2956 patients with a median age of 63 years (interquartile range 54–71) were included in the study, 77.7% of whom were men. In total, 75.1% of patients were compliant at baseline, while at follow-up this figure increased to 79.5% (p<0.0001). During lockdown, only a history of depression showed a trend towards worse adherence (p=0.017).
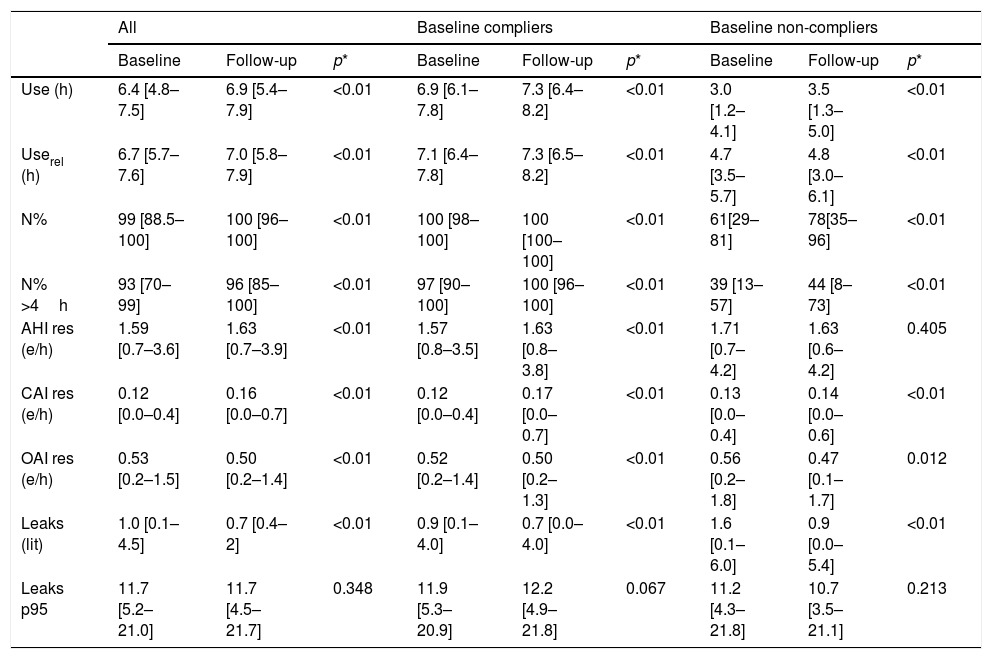
Table 1 shows CPAP use and efficacy parameters during the study periods (baseline vs. follow-up). Overall, during the lockdown period, patients used CPAP for significantly more hours. With regard to treatment effectiveness, a significant decrease in residual obstructive events was observed during lockdown, although central events were significantly increased. In absolute values, leaks were significantly lower during lockdown.
Use of CPAP in the study periods for the overall series and compliers and non-compliers in the baseline period.
| All | Baseline compliers | Baseline non-compliers | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | p* | Baseline | Follow-up | p* | Baseline | Follow-up | p* | |
| Use (h) | 6.4 [4.8–7.5] | 6.9 [5.4–7.9] | <0.01 | 6.9 [6.1–7.8] | 7.3 [6.4–8.2] | <0.01 | 3.0 [1.2–4.1] | 3.5 [1.3–5.0] | <0.01 |
| Userel (h) | 6.7 [5.7–7.6] | 7.0 [5.8–7.9] | <0.01 | 7.1 [6.4–7.8] | 7.3 [6.5–8.2] | <0.01 | 4.7 [3.5–5.7] | 4.8 [3.0–6.1] | <0.01 |
| N% | 99 [88.5–100] | 100 [96–100] | <0.01 | 100 [98–100] | 100 [100–100] | <0.01 | 61[29–81] | 78[35–96] | <0.01 |
| N% >4h | 93 [70–99] | 96 [85–100] | <0.01 | 97 [90–100] | 100 [96–100] | <0.01 | 39 [13–57] | 44 [8–73] | <0.01 |
| AHI res (e/h) | 1.59 [0.7–3.6] | 1.63 [0.7–3.9] | <0.01 | 1.57 [0.8–3.5] | 1.63 [0.8–3.8] | <0.01 | 1.71 [0.7–4.2] | 1.63 [0.6–4.2] | 0.405 |
| CAI res (e/h) | 0.12 [0.0–0.4] | 0.16 [0.0–0.7] | <0.01 | 0.12 [0.0–0.4] | 0.17 [0.0–0.7] | <0.01 | 0.13 [0.0–0.4] | 0.14 [0.0–0.6] | <0.01 |
| OAI res (e/h) | 0.53 [0.2–1.5] | 0.50 [0.2–1.4] | <0.01 | 0.52 [0.2–1.4] | 0.50 [0.2–1.3] | <0.01 | 0.56 [0.2–1.8] | 0.47 [0.1–1.7] | 0.012 |
| Leaks (lit) | 1.0 [0.1–4.5] | 0.7 [0.4–2] | <0.01 | 0.9 [0.1–4.0] | 0.7 [0.0–4.0] | <0.01 | 1.6 [0.1–6.0] | 0.9 [0.0–5.4] | <0.01 |
| Leaks p95 | 11.7 [5.2–21.0] | 11.7 [4.5–21.7] | 0.348 | 11.9 [5.3–20.9] | 12.2 [4.9–21.8] | 0.067 | 11.2 [4.3–21.8] | 10.7 [3.5–21.1] | 0.213 |
Data are displayed by median [interquartile range].
*Non-parametric Wilcoxon signed-rank test for repeated measurements.
AHI res: residual apnea-hypopnea index; CAI res: residual central apnea index; leaks p95: 95% percentile of leaks; N%: percentage of nights using CPAP; N%>4: Percentage of nights using CPAP at least 4h; OAI res: residual obstructive apnea index; Userel : relative use.
It is important to note that after 1 month of lockdown, 27.3% of patients initially considered non-compliant became compliant, while only 3.7% of previous compliers became non-compliers.
Both men and women showed significant differences between the 2 study periods, with significantly greater use during lockdown regardless of sex. However, it should be pointed out that the number of residual obstructive events was significantly lower in men (0.51 vs. 0.48 events/h; p<0.01) than in women (0.56 vs. 0.55 events/h); p<0.059).
Similarly, significantly greater compliance was observed during lockdown in all age ranges, particularly patients ≥65 years of age.
With regard to OSA severity, the same general trends toward increased CPAP use during lockdown were observed. In terms of effectiveness, significantly lower rates of residual obstructive events (0.54 vs. 0.50 events/h; p<0.01) and leaks (1.0 vs. 0.7 liters; p<0.01) were observed during lockdown in patients with moderate to severe OSA. The rate of residual central events was systematically higher during lockdown, irrespective of sex, age, and severity of OSA.
Our findings show that lockdown led to greater compliance. These results are consistent with a recent study conducted by Attias et al.8 Similarly, Altena et al. found that the absence of strict working hours and the reduction of social activities may have led to an improvement in sleep quality during lockdown.9 However, the fear of becoming ill may have promoted better CPAP adherence, despite the possibility of transmission of infection due to mask leaks.10,11
The pandemic has restricted the availability of healthcare for problems other than Covid-19, and this, combined with lockdown, has made it more difficult to access care. Telemedicine takes on special importance in this setting,12,13 since therapeutic monitoring can continue as it did before lockdown and patients can continue to receive healthcare.
The most important limitations of our study are that the degree of compliance with lockdown itself and the emotional, social, and employment status of patients are unknown, factors that could influence the observed trends.
In conclusion, the lockdown resulting from the Covid-19 pandemic has not negatively affected short-term CPAP adherence and compliance. Our results show significantly higher compliance during 1 month of lockdown irrespective of sex, age, and severity of OSA.
Conflict of interestsThe authors state that they have no conflict of interests.
This study has been partially funded by the Ministerio de Ciencia Innovación y Universidades and the European Regional Development Fund (ERDF) through the DPI2017-84280-R project, and by the 'CIBER de Bioingeniería, Biomateriales y Nanomedicina (CIBER-BBN)' of the 'Instituto de Salud Carlos III' , co-funded by ERDF funds.
Please cite this article as: del Campo F, López G, Arroyo CA, de Frutos JF, Crespo A, Cerezo-Hernández A, et al. Estudio de la adherencia al tratamiento con presión continua positiva en la vía aérea en pacientes con síndrome de apnea obstructiva del sueño en el confinamiento impuesto durante la pandemia de COVID-19. Arch Bronconeumol. 2020. https://doi.org/10.1016/j.arbres.2020.06.019