Our patient was a 30-year-old man undergoing investigation of dyspnea and polyglobulia. After being assessed by the hematology department, he was referred to the respiratory medicine department due to a finding of reduced lung diffusion capacity on lung function tests.
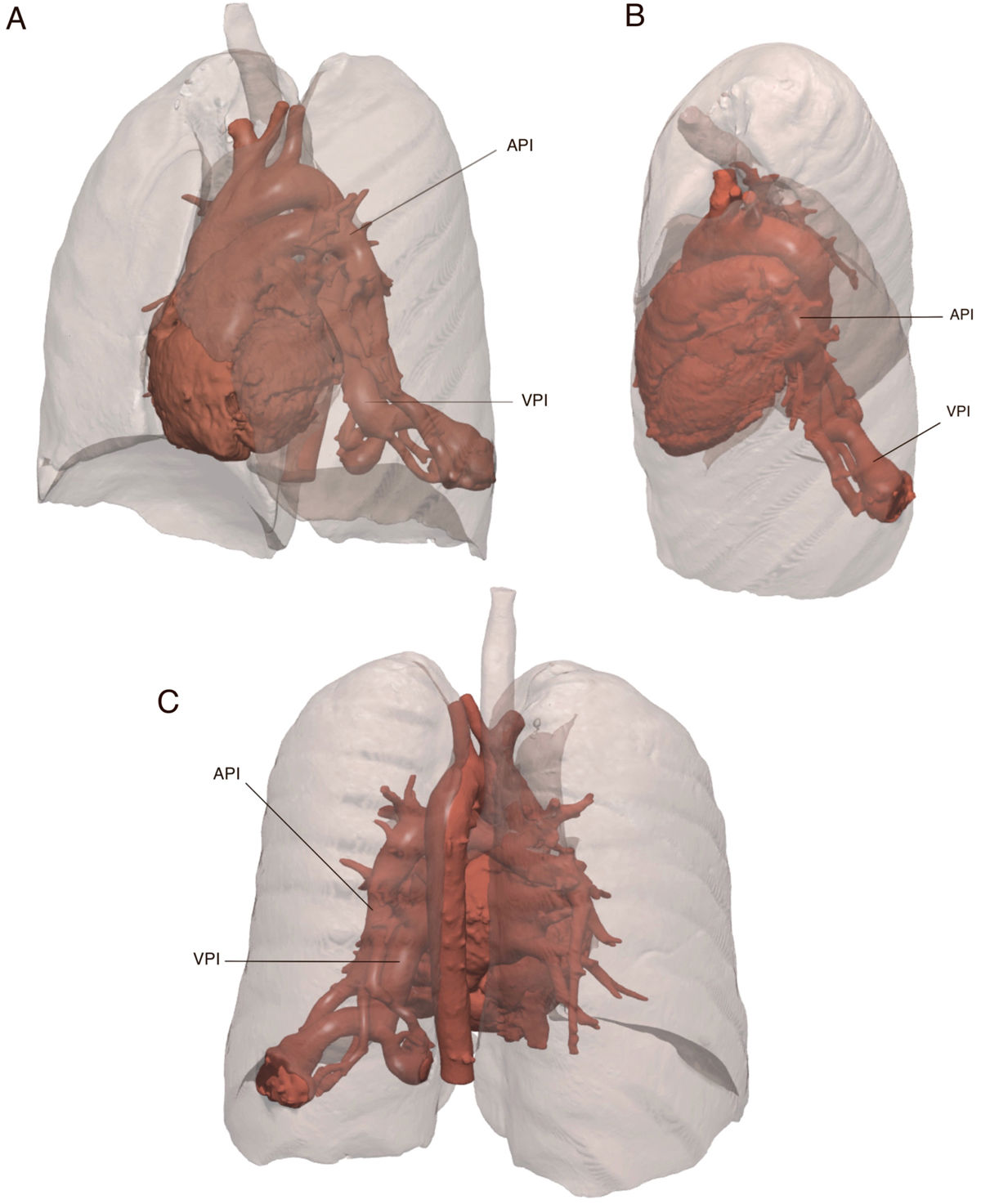
On physical examination, nail clubbing and cyanosis were observed. A CT angiogram was performed, revealing arteriovenous malformation in the left lower lung lobe (Fig. 1). Pulmonary arteriovenous fistula (PAVF) with right-left shunt was diagnosed, and evaluation by thoracic surgery was requested. Left lower lobectomy was performed by single-port video-assisted thoracoscopy. The patient progressed favorably, and at 2 months presented a marked improvement in cyanosis and dyspnea, and blood gases and hematocrit values had completely normalized.
Volumetric reconstruction of contrast-enhanced lung CT angiogram. Left pulmonary artery (LPA) arteriovenous malformation with a maximum caliber of 17mm and arterial branches draining to the left lower pulmonary vein (LPV) with a maximum proximal caliber of 19mm. Two 2 vascular sacs connected by pulmonary arterial and venous branches of 35mm×28mm and a medial sac of 27mm×20mm were also identified. (A) Left anterolateral view. (B) Left laterosuperior view. (C) Posterior view.
PAVFs are malformations that involve direct artery-vein fistula with no intermediate capillary bed.1 They present with an incidence of 2–3/100,000 inhabitants.2 The main clinical signs are hypoxemia with subsequent dyspnea, cyanosis and polycythemia. Surgery is rarely necessary because most are amenable to intravascular treatment. However, surgical resection is essential in cases such as ours, where a large PAVF severely compromises a pulmonary lobe, and embolization is not feasible.
Conflict of interestsThe authors declare that they have no direct or indirect conflict of interests related with the contents of this manuscript.