Healthcare providers performing endoscopic procedures are at risk for poor ergonomic positioning and musculoskeletal strain/injury for numerous reasons, likely related to repetitive, forceful, and prolonged maneuvers.1,2 Limited literature suggests that musculoskeletal pain related to endoscopy3–7 is indeed a phenomenon, but the etiologies generally remain undiscovered. It is likely many factors play a role in modifying ergonomics within the bronchoscopy suite. Monitor screens and positioning providing some impact and represent a potentially easily correctable solution. Important literature from video-assisted surgery describes optimum monitor position being at least 1 meter from the surgeon's eyes with slight declination (0–15°) from a neutral gaze height.8,9 There remains minimal data reflecting the role this may play within bronchoscopy and/or the ergonomic impact monitor height may play during bronchoscopy. We sought to prospectively observe the monitor height selected by bronchoscopists during a randomized trial of ergonomics related to bronchoscope design.
A prospective trial of different bronchoscopy designs was performed on a low-fidelity simulation bronchoscopy mannequin and has previously been reported.10 Within this trial, additional data regarding monitor height during bronchoscopy was collected. As previously described, bronchoscopies were performed on a mannequin utilizing an adjustable-height, standard-sized patient gurney, targeting three pre-defined areas. All bronchoscopies were performed from the head of the bed with the video monitor located toward the foot of the bed on adjustable ceiling mounted boom monitors. All subjects were verbally prompted to adjust the height of the gurney and the monitor to their personal preference prior to each bronchoscopic examination. Subjects were otherwise encouraged to perform bronchoscopy as they typically would perform in their clinical practice.
Subject height measurement was obtained prior to testing for the day with eye height calculated from anthropometric averages.11 Monitor and bed height were obtained immediately prior to each bronchoscopy with no additional feedback offered to the subjects performing bronchoscopy. Monitor height remained untouched and unadjusted by study staff. Suggested monitor height was calculated from each subjects measured body height with a 10° declination of gaze and used as the reference height for their monitor height. All procedures and data collection were performed within the endoscopy suite (IRB Approval – IRB00063334).
All data was de-identified, collected and stored within the REDCap12 database system. Baseline demographics are described using means, standard deviations and percentages. All analysis of data was performed using Excel (Microsoft, Redmond, WA).
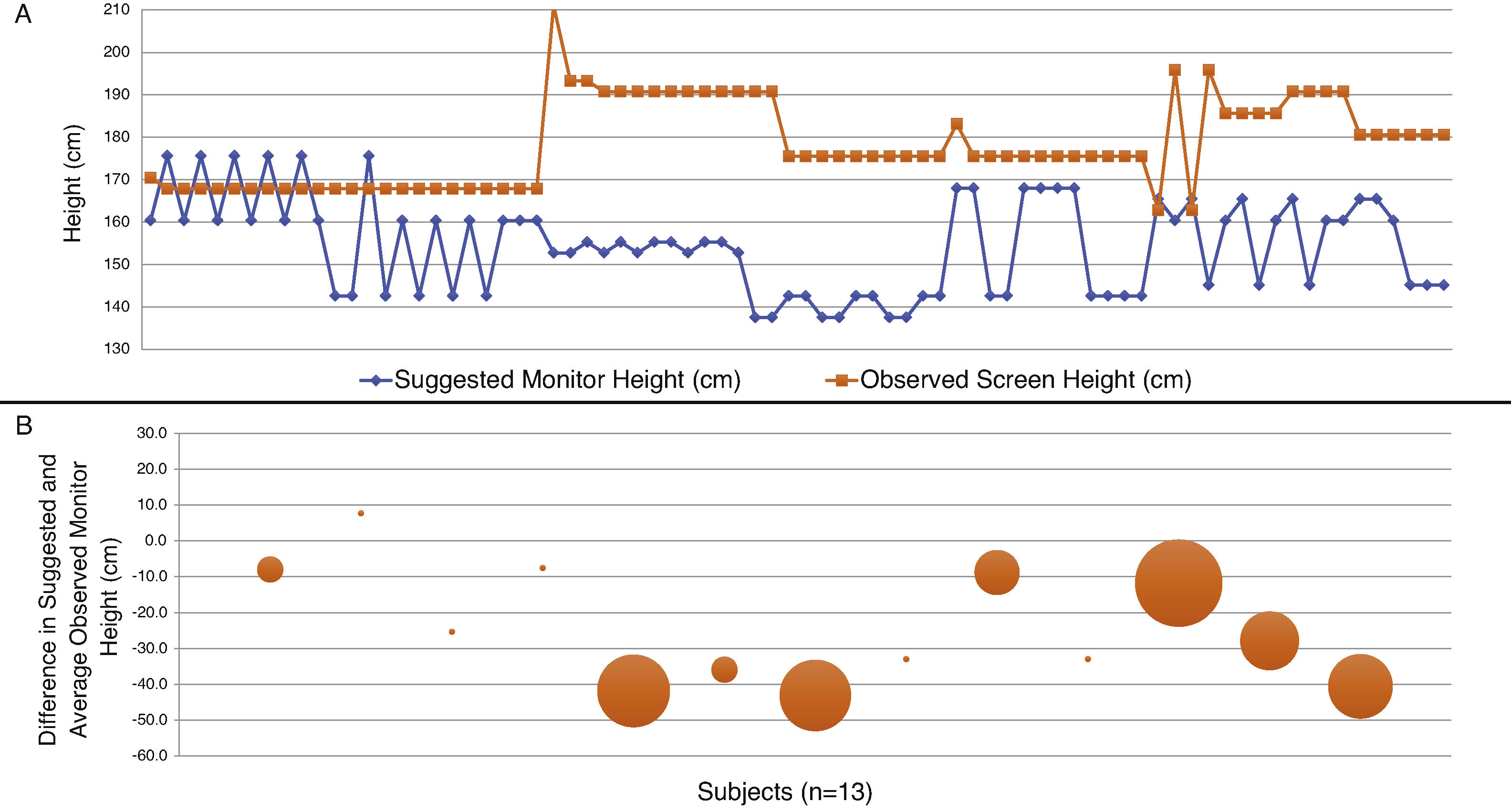
A total of 13 subjects were enrolled within the trial, with each subject performing six separate bronchoscopies, thus providing a total of 78 bronchoscopic exams. Measurements were available for all subjects and bronchoscopy procedures. The mean age of the group was 41.3 (SD 12.9) years with seven males and six females. The mean height of participants was 174.5 (SD 11.68, range 157.5–195.6) cm and the mean body mass index was 24.6 (SD 4.0)kg/m2. During bronchoscopy procedures, the suggested monitor height was incorrect (inclined and above eye line of site) in 89.7% (70/78) of the time (Fig. 1A). Prior to each bronchoscopy, monitor height was adjusted by bronchoscopists only 17.9% (14/78) of the time, with four of the thirteen (30.8%) bronchoscopists never changing the monitor height during their entire testing period. Only five of the thirteen bronchoscopists maintained persistent screen height during their six bronchoscopy procedures, however only one bronchoscopist had an average appropriate screen height (Fig. 1B).
Graphical and pictorial representation of suggested monitor height versus observed monitor height. (A) Graphical display of all 78 bronchoscopies with the suggested monitor height displayed in one line (
) against the observed monitor height in one line (). (B) Graphical display of the difference in suggested and average observed monitor heights by subjects (n=13). Smaller sized dots represent a smaller average difference between the suggested and observed monitor height, consistent with monitor heights that remain similar for each of the six bronchoscopies performed by the subject. Larger dots represent a larger average difference between the suggested and observed monitor height, consistent with varying monitor heights for each of the six bronchoscopies performed by the subject. The presence of a negative number indicates a higher average observed monitor height than suggested by their body height, consistent with poor ergonomic positioning.This study of bronchoscopy related ergonomics remains an exciting one, in particular with the little data published to date. We report somewhat disturbing data on the likely poor ergonomic practices of bronchoscopists during multiple simulated bronchoscopies. Our data suggest that bronchoscopists, despite verbal prompting otherwise, often elect to leave monitor heights unchanged prior to initiation of bronchoscopy and also with the vast majority electing to utilize poorly positioned monitor heights. The most striking abnormality is the apparent preference of an inclined monitor height for bronchoscopy and that many bronchoscopists utilized monitor heights that varied between bronchoscopic procedures. Previous work in ergonomics (including video monitor use during surgery) suggests that the ideal gaze direction should be in the 10–15° downward plane, leading us to conclude that many of our observed bronchoscopists place themselves in poor ergonomic position during bronchoscopy.
It remains unclear as to the basis for our observation of poor ergonomic positioning, highlighting the need for further study to help identify etiologies for poor ergonomic positioning of equipment during bronchoscopic procedures. One of the most likely theories for this observation includes physician education/awareness. It also appears that this may be one of the potentially easiest interventions to help remediate this problem. While many physicians are likely “aware” of ergonomics related to their daily activities, it remains unclear as to how aware they may be when performing specific activities that have a high risk of ergonomically impacting them. A limitation of our study was that we did not query our subjects on their perception of ergonomics prior to initiating the study. Additional limitations of our study include the small sample size, and the fact that it was nested within another prospective trial, however we believed this would be an opportune time to prospectively collect data on bronchoscopists within a controlled and reproducible environment. Strengths of this study include its prospective data collection and the wide range of subjects in regards to age, gender, and height. The use of a fully mobile, ceiling mounted video monitor also adds strength to this project as any height/modification could be easily accommodated. We also purposefully prompted each bronchoscopist to make them aware of the potential to modify monitor height each time they were performing bronchoscopy.
In conclusion we present a novel report on the disturbing observation of poor ergonomic positioning of monitor height during bronchoscopy. We hope this report serves as an overall warning and educational opportunity to bronchoscopists (and potentially other endoscopists) regarding potential interventions that can improve ergonomics. We also hope this report will prompt additional research within this oft neglected topic.
Authors ContributionsCRG, JT, AC, NJP, ACA, ADL, HJL, and LBY all contributed to study design, data acquisition, and analysis, drafting of the manuscript, final approval of the manuscript. All authors agree to be accountable for all aspects of the final submitted manuscript.