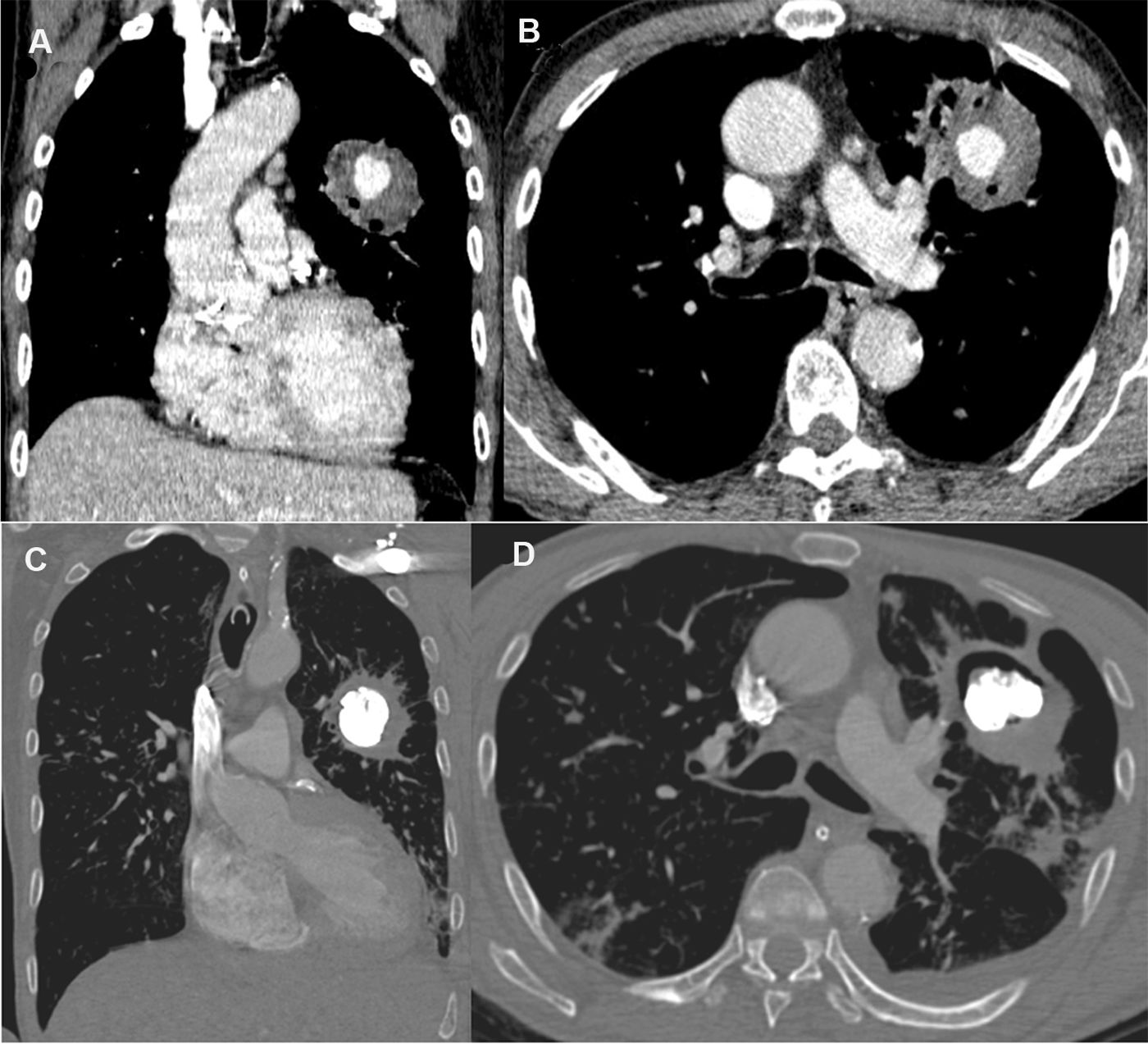
A 65-year-old man recently diagnosed with pulmonary tuberculosis presented to the emergency department due to cough and daily hemoptysis episodes (50–100ml blood/episode). While hospitalized, he experienced a severe massive bleeding episode, prompting emergency fiberoptic bronchoscopy that revealed a clot obstructing the left main bronchus. Chest computed tomography demonstrated the presence of a round opacity in the left upper lobe, with a nodular formation with intense contrast uptake inside, compatible with Rasmussen aneurysm (RA; Fig. 1A and B). The patient underwent angiography of the pulmonary and bronchial arteries, which did not demonstrate aneurysmal formation. Ultrasound-guided aneurysmal sac puncture using a 22G Chiba needle and percutaneous embolization with a cyanoacrylate/Lipiodol® solution under fluoroscopic visualization were performed. The RA was adequately filled with embolizing material (Fig. 1C and D). The patient was discharged 3 days after the procedure, and was completely asymptomatic after 1 year of follow up. Tuberculosis is a significant cause of hemoptysis globally, especially in developing countries, and RA is a rare but life-threatening complication. For most cases of RA, especially those with life-threatening hemoptysis, safer and less-invasive endovascular therapy with embolization has replaced surgical intervention. In some cases, however, percutaneous injection therapy can be considered because embolization of the pulmonary or bronchial arteries alone may fail to control the hemoptysis.1,2
Enhanced coronal (A) and axial (B) computed tomography images showing an inhomogeneous round opacity in the left upper lobe, with a nodular formation showing intense contrast uptake inside, compatible with Rasmussen's aneurysm. Enhanced coronal (C) and axial (D) computed tomography images acquired 48h after treatment demonstrated the adequate filling of the Rasmussen's aneurysm with embolizing material, with no indication of new bleeding.
The authors state that they have no conflict of interests.