Various side effects during long-term penicillamine treatment have been described, especially dermatological reactions, such as exfoliative dermatitis, rash and alopecia.1 Other adverse events, such as vasculitis and thyroiditis, have also been reported. Respiratory effects have been documented, albeit less frequently, including cases of asthma, pulmonary fibrosis, interstitial pneumonitis and bronchiolitis obliterans.
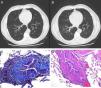
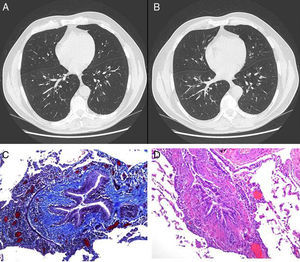
We present the case of a male patient, 47 years of age, never-smoker, with a clinical history of hypertension on medical treatment, dyslipidemia on treatment with statins, Graves–Basedow disease treated 8 years ago with radioiodine (currently receiving replacement therapy) and Wilson's disease diagnosed 20 years ago, initially treated with zinc and for the past 2 years with penicillamine. He had a work history as a salesman, with no contact with toxic substances or poultry. The patient consulted due to dyspnea on exertion. An initial lung function study was performed which showed severe airflow limitation, so treatment with inhaled corticosteroids was initiated. A computed tomography (CT) scan of the chest was requested, along with complete lung function testing, revealing severe irreversible obstructive changes with air trapping and reduced carbon monoxide diffusing capacity (DLCO). Discrete bronchiectasis and diffuse bronchiolectasis were observed on the CT scan (Fig. 1). A sweat test to rule out cystic fibrosis was negative and an immunoglobulin study was normal. During the follow-up visit, respiratory failure was observed, so the decision was taken to admit the patient for further tests. On physical examination, oxygen saturation (breathing room air) was remarkable due to pulse oximetry of 88% without signs of labored breathing and normal pulmonary auscultation. The rest of the physical examination was normal. General clinical laboratory tests were unchanged and the chest CT was the same as before. In view of suspected drug-induced bronchiolitis, a biopsy was obtained from the lingula by anterior thoracotomy. After an uneventful post-operative period, the patient was discharged with domiciliary oxygen therapy. The final diagnosis from the pathology study was follicular bronchiolitis associated with constrictive bronchiolitis obliterans.
(A and B) An increase in the bronchoalveolar ratio is seen in the high definition CT scan during inspiration and expiration, a radiological sign suggestive of bronchiectasis and diffuse bronchiolectasis. No radiological signs of air trapping are observed. (C) Histological sample obtained from lung biopsy: Masson's trichrome stain; bronchiolar submucosal fibrosis is seen, along with the appearance of small scars. (D) Histological sample obtained from the lung biopsy: hematoxylin–eosin stain: bronchial obliteration can be observed.
The decision was taken to discontinue penicillamine treatment and start treatment with bronchodilators and corticosteroids (methylprednisolone 40mg/day), and the patient was referred to a reference center for evaluation for lung transplantation. In May 2012, a double-lung transplant was successfully performed.
Bronchiolitis obliterans is a non-specific disorder of the small airways (<2mm in diameter). Its clinical presentation is very non-specific (cough and progressive dyspnea). Physical examination is unremarkable and signs of hyperinflation, prolonged expiration and non-specific breathing noises such as rhonchi, crackles or wheezing may be observed. A plain chest X-ray may be normal or show signs of air trapping. Additional information can be obtained from a high resolution CT scan during inspiration and expiration. Distinctive radiological signs in the expiration slices have been described on the CT scan which could guide diagnosis, whether direct (bronchiolar wall thickening with the typical “tree-in-bud” pattern, bronchiolectasis and centrilobar nodules) or indirect (subsegmental atelectasis and signs of air trapping). This syndrome can be classified by etiology or pathology.1,2 From an etiological point of view, idiopathic cases must be distinguished from those caused by secondary factors. These latter cases are usually acute, the causative agent (primarily drugs or toxic substances) is known, and there is a good response to bronchodilator treatment. The following histopathological classifications have been described: constrictive, proliferative and follicular bronchiolitis, central interstitial fibrosis and diffuse panbronchiolitis. Bronchiolitis can be diagnosed from the clinical signs and symptoms and appropriate complementary tests, but the definitive diagnosis is obtained from lung biopsy. Treatment is based on corticosteroid therapy, bronchodilators, macrolide antibiotic treatment and in the case of rapid progression, lung transplant.
Our patient presented a case of constrictive bronchiolitis obliterans which has an uncommon histological pattern, characterized by changes in the bronchiolar wall caused by inflammatory phenomena and fibrosis, leading to a reduction or obliteration of the bronchial lumen due to scarring processes. It is generally induced by drugs, systemic disease or infection.
To conclude, this clinical case is presented as an example of an infrequent but previously described side effect of a treatment which is commonly used in several diseases.3,4 Our case demonstrates the lack of specificity of the clinical presentation and complementary studies, the severity and irreversibility of the symptoms and the need for a definitive diagnosis by way of an invasive test. This condition may on occasions require treatment with lung transplantation.5,6
Please cite this article as: Bruguera-Àvila N, et al. Bronquiolitis obliterante en paciente tratado con d-penicilamina. Arch Bronconeumol. 2013;49:411–12.