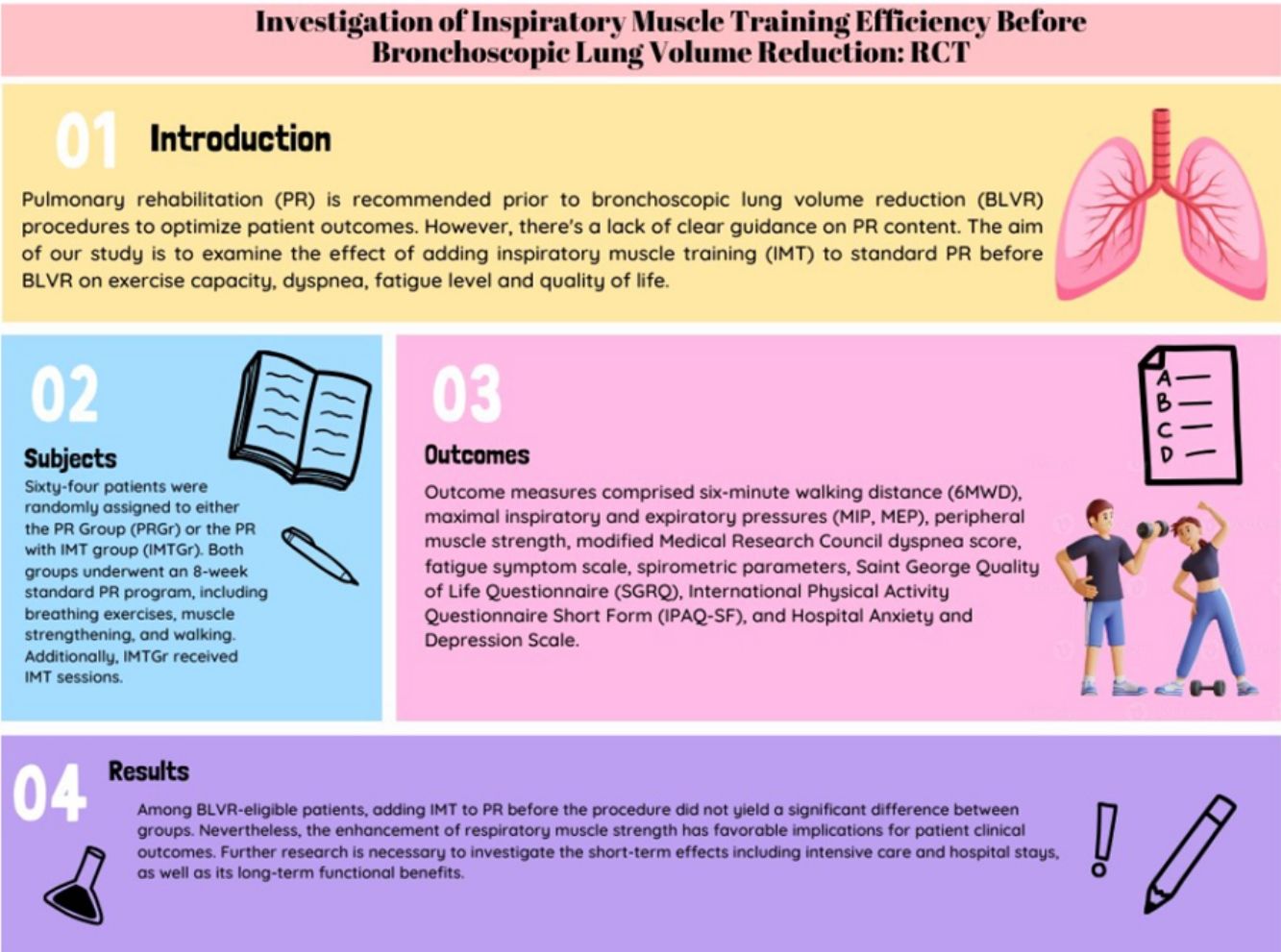
Pulmonary rehabilitation (PR) is recommended prior to bronchoscopic lung volume reduction (BLVR) procedures to optimize patient outcomes. However, there's a lack of clear guidance on PR content. The aim of our study is to examine the effect of adding inspiratory muscle training (IMT) to standard PR before BLVR on exercise capacity, dyspnea, fatigue level and quality of life.
MethodsSixty-four patients were randomly assigned to either the PR Group (PRGr) or the PR with IMT group (IMTGr). Both groups underwent an 8-week standard PR program, including breathing exercises, muscle strengthening, and walking. Additionally, IMTGr received IMT sessions. Outcome measures comprised six-minute walking distance (6MWD), maximal inspiratory and expiratory pressures (MIP, MEP), peripheral muscle strength, modified Medical Research Council dyspnea score, fatigue symptom scale, spirometric parameters, Saint George Quality of Life Questionnaire (SGRQ), International Physical Activity Questionnaire Short Form (IPAQ-SF), and Hospital Anxiety and Depression Scale.
ResultsOur study found no significant difference in exercise capacity improvement between IMTGr and PRGr. However, IMTGr showed significant improvement in MIP compared to PRGr. Both groups experienced improvements in dyspnea, fatigue, and depression scores, as well as enhancements in 6MWD, MEP, peripheral muscle strength, IPAQ-SF and SGRQ scores.
ConclusionAdding IMT to PR did not show a significant difference between groups among BLVR-eligible patients. However, improved respiratory muscle strength may have positive clinical implications. Further research is needed to explore short and long-term effects.
Emphysema, a common feature of Chronic Obstructive Pulmonary Disease (COPD), is strongly linked to disease severity and prognosis. Patients with emphysematous COPD often experience dyspnea, limited exercise capacity, cardiac issues, and poor outcomes due to lung hyperinflation.1,2 To address this, bronchoscopic lung volume reduction (BLVR) therapies like valve and coil treatments have gained prominence in COPD research. These procedures aim to alleviate hyperinflation, leading to improved lung function, exercise capacity, and quality of life. BLVR procedures were integrated into the GOLD guidelines in 2017.3
Hyperinflation can have significant repercussions on respiratory muscle function, particularly impacting the diaphragm. This crucial muscle experiences a mechanical decrease in activity, primarily due to compression.4 Moreover, structural alterations occur within the respiratory muscles under such circumstances. Biopsies of the diaphragm reveal a decline in Type II (fast) fibers, accompanied by an increase in Type I (slow, fatigue-resistant) fibers. Studies have demonstrated that during hyperinflation, the length of the diaphragm can decrease by up to 40% compared to normal levels at Functional Residual Capacity. This alteration in length profoundly affects the force–capacity relationship of the diaphragm.4,5 Furthermore, systemic factors prevalent in hyperinflation cases, such as weight loss, electrolyte imbalances, hypercapnia, hypoxia, and oxidative stress, also exert a considerable influence on respiratory muscle function.5
Inspiratory Muscle Training (IMT), one of the components of pulmonary rehabilitation (PR), has been used in chronic lung diseases for years. There is data showing that IMT reduces diaphragmatic activation by strengthening the respiratory muscles, and that reduced excessive diaphragmatic activation also reduces the perceived level of dyspnea.6–8 It improves patients’ ability to sustain high levels of ventilation. In the ATS/ERS guideline published in 2013, it is stated that IMT applied in addition to PR in patients with respiratory muscle weakness will provide additional benefit by increasing respiratory muscle strength.7 The benefits mentioned here are not detailed, and the patient group primarily includes respiratory diseases such as COPD.
Preoperative PR programs are recommended for BLVR procedures.9 Guidelines in this area emphasize the importance of implementing PR or a comprehensive exercise program prior to making decisions regarding procedures such as BLVR.10 The primary objective is to assess the potential benefits of PR on patients’ clinical outcomes, particularly in alleviating dyspnea and improving quality of life.11 PR has the potential to either eliminate the need for procedures or enhance the success rate of such interventions. Pulmonary functions and exercise capacity play pivotal roles in determining the necessity of procedures for individuals with COPD. Literature consistently reports the beneficial impact of PR on these parameters.12 Consequently, understanding the positive effects of PR on pulmonary functions and exercise capacity is paramount in guiding clinical decisions regarding appropriate interventions for COPD patients. However, there is a lack of information regarding the specific content of the program for this patient group, and standard PR programs are typically applied. In the literature, there is only one study that examines the effectiveness of home-based and hospital-based PR programs before the bronchoscopic procedure.13 No study investigating the effectiveness of IMT in this patient group has been found. In the study, the aim was to investigate whether IMT might increase the gains of the PR program or not. Our study holds the distinction of being the first to explore this aspect. The hypothesis of our study is that adding IMT to PR will reduce perceived dyspnea levels, improve exercise capacity, physical activity level and also quality of life.
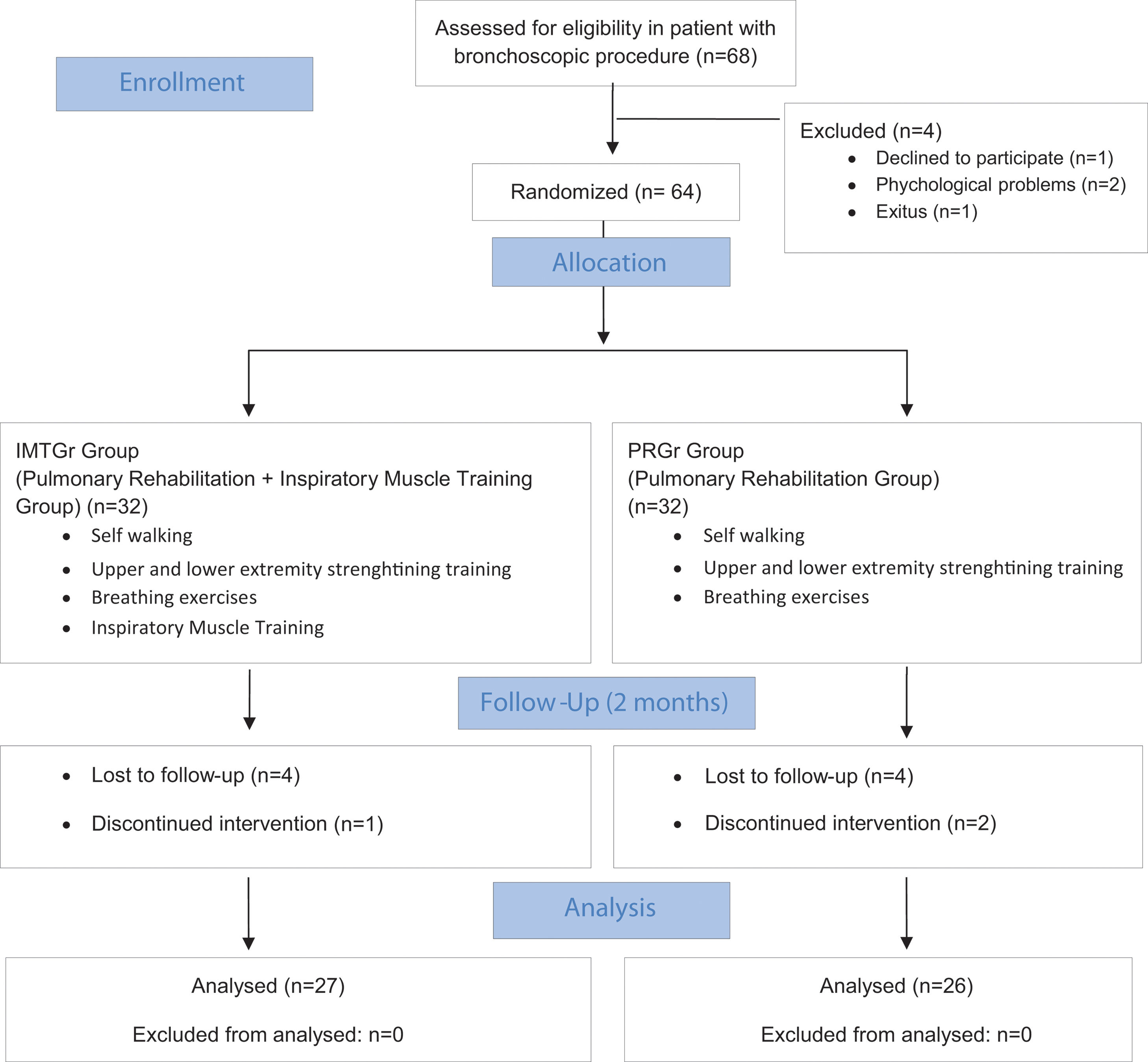
MethodsStudy designA prospective, non-blinded, randomized controlled study was conducted. The study was approved by the local ethics committee (Protocol number: 2022/238) and registered to ClinicalTrials.gov website (registration number: NCT05540054). It was carried out between September 2022 and June 2023. The study was conducted in accordance with the Helsinki Declaration. A written informed consent was obtained from each patient.
The study included individuals with COPD who were listed to undergo a BLVR by the pulmonary diseases council and who were in consultation with PR program. All cases had a modified Medical Research Council Dyspnea score (mMRC) of at least 2 and a forced expiratory volume in 1s (FEV1) percentage below 45%. The planned bronchoscopic procedures were valve or coil. The patients were eligible for inclusion if they had: a diagnosis of pulmonary emphysema; were listed for bronchoscopic procedures; had been medically stable for the past 4 weeks; had no orthopedic or cardiac problems that would prevent them from exercising; showed the presence of dyspnea on exertion; and had the ability to use a smartphone. Patients with severe comorbid disease, unstable coronary artery disease, collagen vascular diseases, and requiring high oxygen therapy (>3–4L/min), a history of exertional syncope, or any comorbidity that interferes with exercise training (severe orthopedic or neurological deficits or unstable heart disease) and those who had participated in a pulmonary rehabilitation program in the last 12 months were excluded from the study.
Participants who met the study inclusion criteria and completed the baseline assessments were randomly allocated into one of the two groups: namely, the Pulmonary Rehabilitation Group (PRGr) or the Pulmonary Rehabilitation plus Inspiratory Muscle Training Group (IMTGr), in a 1:1 ratio using the randomization website (https://www.randomizer.org/). All assessments were performed on the same day before and after rehabilitation.
Medical follow-up of all patients was continued by a pulmonology specialist. All patients were given an education on the definition of their disease, the importance of regular medical follow-up and physical activity, and the role of PR in ensuring disease control. Exercise training was carried out by an experienced physiotherapist. The first exercise sessions and all evaluations of all cases were conducted at the hospital. The 2nd and 3rd training sessions were carried out in patients’ homes via online synchronized videoconferencing. Those who completed the three training sessions received exercise videos on their smartphones and continued exercising on their own. Participants received weekly phone calls for exercise follow-up.
InterventionsAll patients underwent a PR exercise program 3 days a week for 8 weeks, including breathing exercises, muscle strengthening, and walking training. The program also included inspiratory muscle training for the IMTGr. Breathing exercises targeted chest, diaphragmatic, and lateral basal lobes, with 10 repetitions performed twice daily. Peripheral muscle strengthening utilized a TheraBand for resistance. Strengthening exercises were applied to major muscle groups in both the upper and lower extremities with 10 repetitions each. Progression was made by increasing the number of repetitions and sets weekly. Self-walking intensity was determined at 60% workload utilizing data derived from the six-minute walking test (6MWT).14 Furthermore, participants were instructed to maintain a perceived level of fatigue between 12 and 14 on the Borg Rating of Perceived Exertion (RPE) scale during walking and were educated on the specifics of this instruction. IMTGr received additional training Powerbreath Classic device (POWERbreathe International Ltd., England, UK), progressively increasing workload to 30–50% of maximum inspiratory pressure over 8 weeks. For the IMT exercise session, patients were instructed to sit on a chair with back support, place the device with adjustable resistance in their mouth, take a deep and strong breath in, and exhale comfortably all the way down to residual volume. This regimen, comprising 7 sets of 2min work and 1min rest, aimed to enhance inspiratory muscle strength and endurance.15 To ensure program adherence and enable the progression of exercise load, weekly online video calls were conducted with patients.
Outcome measurementsAll assessments of the patients were conducted at the hospital both at baseline and after 8 weeks. Exercise capacity, dyspnea level, and respiratory muscle strength were primary outcome measurements. Functional capacity was evaluated using the 6MWT following the guidelines of the American Thoracic Society (ATS), wherein patients were instructed to walk as quickly as possible between two cones positioned 30m apart, and the distance covered in 6min was recorded. Additionally, oxygen saturation and heart rate were measured before and after the test using a pulse oximeter.16 Dyspnea perceptions during daily activities were assessed using the modified Medical Research Council scale.17 Dyspnea was also scored by the patient using the modified Borg scale.18
Pulmonary Function Tests were conducted using the Pony Fx Desktop Spirometer (Cosmed; Italy), adhering to ERS/ATS guidelines.19 The maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP) measurements were performed with the Pony Fx instrument from Cosmed (Cosmed; Italy). The test was conducted following ERS statement.20 The patient placed a rubber mouthpiece with flanges on the device, sealed their lips firmly around the mouthpiece, exhaled/inhaled slowly and completely, and then tried to breathe as hard as possible.21 The patient was allowed to rest for approximately one minute, and the maneuver was repeated until the peak value was achieved. Verbal or visual feedback was provided after each maneuver, and the aim was to achieve a variability between measurements of less than 5cmH2O. The maximum value was recorded.22 Hand grip strength was assessed using a hydraulic dynamometer, while upper and lower extremity muscle strength measurements were obtained using a hand-held dynamometer (Lafayette Instrument Company, USA) on the dominant side, with each measurement performed three times and the highest value analyzed.23 The International Physical Activity Questionnaire Short Form (IPAQ-SF) involved summing reported minutes spent in different intensity levels of physical activity over the past seven days, categorized into vigorous, moderate, and walking activities. Scores for each category were obtained by multiplying time spent in minutes per day by a corresponding metabolic equivalent of task (MET) value standardized relative to resting metabolic rate.24 The Saint George Respiratory Questionnaire (SGRQ) was utilized as a quality of life scale specific to respiratory diseases, with scores ranging from 0 (no impairment) to 100 (highest impairment).25 Fatigue levels were assessed using the Fatigue Severity Scale (FSS),26 and patients’ anxiety and depression levels were evaluated using the Hospital Anxiety Depression Scale (HADS), with 7 items for each subscale.27
Data analysis and sample sizeStatistical analysis was carried out using the SPSS software program (version 25, USA). The normality of variable distributions was assessed through the utilization of the Shapiro–Wilk statistic. Nonparametric tests were employed for comparisons. The Mann–Whitney U test was used to compare baseline features. Specifically, the pre- and post-treatment data of the groups were compared using the Wilcoxon Signed Rank Test. Median values with the range from minimum to maximum were used to express nonparametric variables, while percentages were used for descriptive variables. Categorical variables were analyzed using the chi-square test. To explore potential differences in the effects of interventions between groups, a mixed ANOVA (repeated measures ANOVA with a between-subjects factor) was utilized. A significance level of p<0.05 was considered to indicate statistical significance. The effect size was assessed using Cohen's d for six minute walking distance. According to Cohen,28 Cohen's d values of 0.2, 0.5, and 0.8 represent small, medium, and large effect sizes, respectively.
The sample size for the study was determined based on the study conducted by JF Liu et al.,29 which reports a significant difference with an effect size of 0.91 between inspiratory muscle training and control groups at 6 weeks in 6MWT distance (360±70 vs 419±60m). Accordingly, to be able to detect such difference with a power of 90% at a confidence level of 95%, we calculated that 27 patients are needed in each group for the study. However, considering that there may be dropouts throughout the study, sample size was increased by 20% and 32 patients were included in each group.
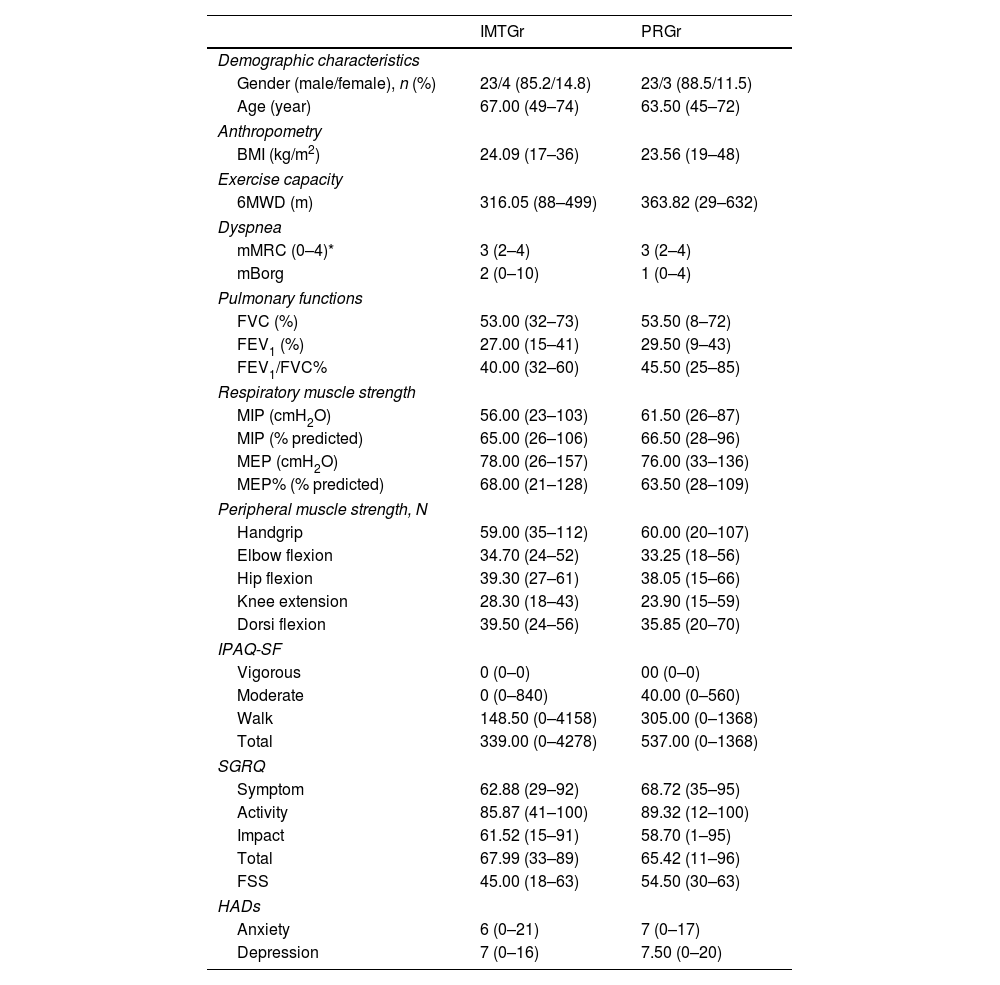
ResultsA total of 68 emphysema patients were referred for PR before BLVR. Sixty-four were randomized into study groups, while eleven were excluded for various reasons (Fig. 1). The average age was 64 years, with 86.8% males. Baseline characteristics showed no significant differences between groups, except for fatigue scores (p=0.028). Refer to Table 1 for detailed demographic and baseline clinical data.
Demographic and clinical baseline characteristics and clinical baseline study outcomes of the groups.
| IMTGr | PRGr | |
|---|---|---|
| Demographic characteristics | ||
| Gender (male/female), n (%) | 23/4 (85.2/14.8) | 23/3 (88.5/11.5) |
| Age (year) | 67.00 (49–74) | 63.50 (45–72) |
| Anthropometry | ||
| BMI (kg/m2) | 24.09 (17–36) | 23.56 (19–48) |
| Exercise capacity | ||
| 6MWD (m) | 316.05 (88–499) | 363.82 (29–632) |
| Dyspnea | ||
| mMRC (0–4)* | 3 (2–4) | 3 (2–4) |
| mBorg | 2 (0–10) | 1 (0–4) |
| Pulmonary functions | ||
| FVC (%) | 53.00 (32–73) | 53.50 (8–72) |
| FEV1 (%) | 27.00 (15–41) | 29.50 (9–43) |
| FEV1/FVC% | 40.00 (32–60) | 45.50 (25–85) |
| Respiratory muscle strength | ||
| MIP (cmH2O) | 56.00 (23–103) | 61.50 (26–87) |
| MIP (% predicted) | 65.00 (26–106) | 66.50 (28–96) |
| MEP (cmH2O) | 78.00 (26–157) | 76.00 (33–136) |
| MEP% (% predicted) | 68.00 (21–128) | 63.50 (28–109) |
| Peripheral muscle strength, N | ||
| Handgrip | 59.00 (35–112) | 60.00 (20–107) |
| Elbow flexion | 34.70 (24–52) | 33.25 (18–56) |
| Hip flexion | 39.30 (27–61) | 38.05 (15–66) |
| Knee extension | 28.30 (18–43) | 23.90 (15–59) |
| Dorsi flexion | 39.50 (24–56) | 35.85 (20–70) |
| IPAQ-SF | ||
| Vigorous | 0 (0–0) | 00 (0–0) |
| Moderate | 0 (0–840) | 40.00 (0–560) |
| Walk | 148.50 (0–4158) | 305.00 (0–1368) |
| Total | 339.00 (0–4278) | 537.00 (0–1368) |
| SGRQ | ||
| Symptom | 62.88 (29–92) | 68.72 (35–95) |
| Activity | 85.87 (41–100) | 89.32 (12–100) |
| Impact | 61.52 (15–91) | 58.70 (1–95) |
| Total | 67.99 (33–89) | 65.42 (11–96) |
| FSS | 45.00 (18–63) | 54.50 (30–63) |
| HADs | ||
| Anxiety | 6 (0–21) | 7 (0–17) |
| Depression | 7 (0–16) | 7.50 (0–20) |
Data are reported as median (minimum-maximum).
IMTGr: The standard pulmonary rehabilitation plus inspiratory muscle training group; PRGr: The standard pulmonary rehabilitation group, 6MWD: 6-Minute Walking Distance, BMI: body mass index, mBorg: modified Borg Scale, mMRC: modified Medical Research Council Association dyspnea score, FVC: forced vital capacity, FEV1: forced expiratory volume in one second, MIP: maximum inspiratory pressure, MEP: maximum expiratory pressure, IPAQ-SF: International physical activity questionnaire short-form, SGRQ: Saint George Respiratory Questionnaire, FSS: fatigue symptom scale, HADs: hospital anxiety and depression scale.
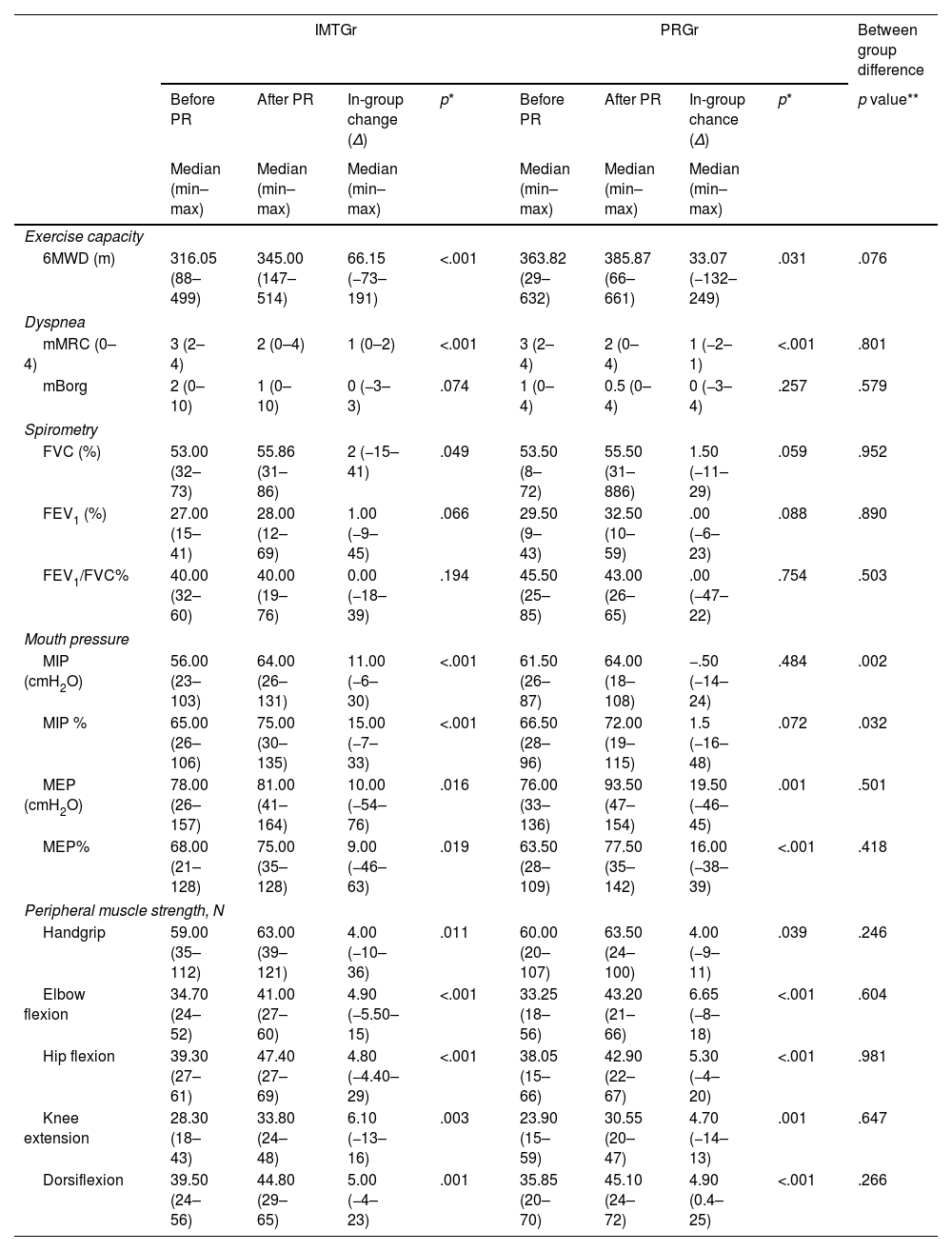
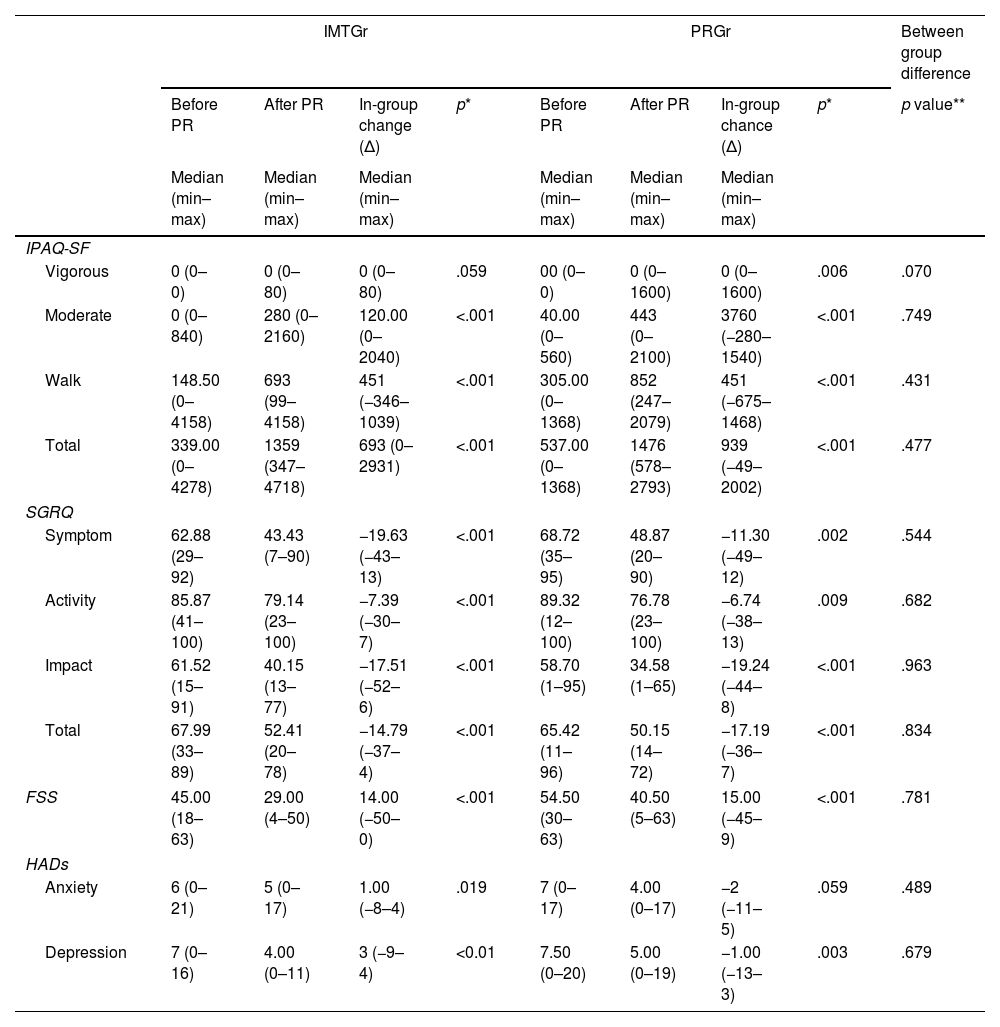
In the comparison between the PR group and the group with IMT added to PR, except for MIP, the groups were similar; there were no superiority of one group over the other (Tables 2 and 3).
The effect of treatment on functional exercise capacity, dyspnea, respiratory functions and muscle strength.
| IMTGr | PRGr | Between group difference | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Before PR | After PR | In-group change (Δ) | p* | Before PR | After PR | In-group chance (Δ) | p* | p value** | |
| Median (min–max) | Median (min–max) | Median (min–max) | Median (min–max) | Median (min–max) | Median (min–max) | ||||
| Exercise capacity | |||||||||
| 6MWD (m) | 316.05 (88–499) | 345.00 (147–514) | 66.15 (−73–191) | <.001 | 363.82 (29–632) | 385.87 (66–661) | 33.07 (−132–249) | .031 | .076 |
| Dyspnea | |||||||||
| mMRC (0–4) | 3 (2–4) | 2 (0–4) | 1 (0–2) | <.001 | 3 (2–4) | 2 (0–4) | 1 (−2–1) | <.001 | .801 |
| mBorg | 2 (0–10) | 1 (0–10) | 0 (−3–3) | .074 | 1 (0–4) | 0.5 (0–4) | 0 (−3–4) | .257 | .579 |
| Spirometry | |||||||||
| FVC (%) | 53.00 (32–73) | 55.86 (31–86) | 2 (−15–41) | .049 | 53.50 (8–72) | 55.50 (31–886) | 1.50 (−11–29) | .059 | .952 |
| FEV1 (%) | 27.00 (15–41) | 28.00 (12–69) | 1.00 (−9–45) | .066 | 29.50 (9–43) | 32.50 (10–59) | .00 (−6–23) | .088 | .890 |
| FEV1/FVC% | 40.00 (32–60) | 40.00 (19–76) | 0.00 (−18–39) | .194 | 45.50 (25–85) | 43.00 (26–65) | .00 (−47–22) | .754 | .503 |
| Mouth pressure | |||||||||
| MIP (cmH2O) | 56.00 (23–103) | 64.00 (26–131) | 11.00 (−6–30) | <.001 | 61.50 (26–87) | 64.00 (18–108) | −.50 (−14–24) | .484 | .002 |
| MIP % | 65.00 (26–106) | 75.00 (30–135) | 15.00 (−7–33) | <.001 | 66.50 (28–96) | 72.00 (19–115) | 1.5 (−16–48) | .072 | .032 |
| MEP (cmH2O) | 78.00 (26–157) | 81.00 (41–164) | 10.00 (−54–76) | .016 | 76.00 (33–136) | 93.50 (47–154) | 19.50 (−46–45) | .001 | .501 |
| MEP% | 68.00 (21–128) | 75.00 (35–128) | 9.00 (−46–63) | .019 | 63.50 (28–109) | 77.50 (35–142) | 16.00 (−38–39) | <.001 | .418 |
| Peripheral muscle strength, N | |||||||||
| Handgrip | 59.00 (35–112) | 63.00 (39–121) | 4.00 (−10–36) | .011 | 60.00 (20–107) | 63.50 (24–100) | 4.00 (−9–11) | .039 | .246 |
| Elbow flexion | 34.70 (24–52) | 41.00 (27–60) | 4.90 (−5.50–15) | <.001 | 33.25 (18–56) | 43.20 (21–66) | 6.65 (−8–18) | <.001 | .604 |
| Hip flexion | 39.30 (27–61) | 47.40 (27–69) | 4.80 (−4.40–29) | <.001 | 38.05 (15–66) | 42.90 (22–67) | 5.30 (−4–20) | <.001 | .981 |
| Knee extension | 28.30 (18–43) | 33.80 (24–48) | 6.10 (−13–16) | .003 | 23.90 (15–59) | 30.55 (20–47) | 4.70 (−14–13) | .001 | .647 |
| Dorsiflexion | 39.50 (24–56) | 44.80 (29–65) | 5.00 (−4–23) | .001 | 35.85 (20–70) | 45.10 (24–72) | 4.90 (0.4–25) | <.001 | .266 |
IMTGr: The standard pulmonary rehabilitation plus inspiratory muscle training group; PRGr: The standard pulmonary rehabilitation group. 6MWD: 6-minute walking distance, mBorg: modified Borg Scale, mMRC: modified Medical Research Council Association dyspnea score, FVC: forced vital capacity, FEV1: forced expiratory volume in one second, MIP: maximum inspiratory pressure, MEP: maximum expiratory pressure. The decrease in mMRC scores are better results.
The effect of treatment on physical activity level, quality of life, fatigue, anxiety and depression, and cognitive functions.
| IMTGr | PRGr | Between group difference | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Before PR | After PR | In-group change (Δ) | p* | Before PR | After PR | In-group chance (Δ) | p* | p value** | |
| Median (min–max) | Median (min–max) | Median (min–max) | Median (min–max) | Median (min–max) | Median (min–max) | ||||
| IPAQ-SF | |||||||||
| Vigorous | 0 (0–0) | 0 (0–80) | 0 (0–80) | .059 | 00 (0–0) | 0 (0–1600) | 0 (0–1600) | .006 | .070 |
| Moderate | 0 (0–840) | 280 (0–2160) | 120.00 (0–2040) | <.001 | 40.00 (0–560) | 443 (0–2100) | 3760 (−280–1540) | <.001 | .749 |
| Walk | 148.50 (0–4158) | 693 (99–4158) | 451 (−346–1039) | <.001 | 305.00 (0–1368) | 852 (247–2079) | 451 (−675–1468) | <.001 | .431 |
| Total | 339.00 (0–4278) | 1359 (347–4718) | 693 (0–2931) | <.001 | 537.00 (0–1368) | 1476 (578–2793) | 939 (−49–2002) | <.001 | .477 |
| SGRQ | |||||||||
| Symptom | 62.88 (29–92) | 43.43 (7–90) | −19.63 (−43–13) | <.001 | 68.72 (35–95) | 48.87 (20–90) | −11.30 (−49–12) | .002 | .544 |
| Activity | 85.87 (41–100) | 79.14 (23–100) | −7.39 (−30–7) | <.001 | 89.32 (12–100) | 76.78 (23–100) | −6.74 (−38–13) | .009 | .682 |
| Impact | 61.52 (15–91) | 40.15 (13–77) | −17.51 (−52–6) | <.001 | 58.70 (1–95) | 34.58 (1–65) | −19.24 (−44–8) | <.001 | .963 |
| Total | 67.99 (33–89) | 52.41 (20–78) | −14.79 (−37–4) | <.001 | 65.42 (11–96) | 50.15 (14–72) | −17.19 (−36–7) | <.001 | .834 |
| FSS | 45.00 (18–63) | 29.00 (4–50) | 14.00 (−50–0) | <.001 | 54.50 (30–63) | 40.50 (5–63) | 15.00 (−45–9) | <.001 | .781 |
| HADs | |||||||||
| Anxiety | 6 (0–21) | 5 (0–17) | 1.00 (−8–4) | .019 | 7 (0–17) | 4.00 (0–17) | −2 (−11–5) | .059 | .489 |
| Depression | 7 (0–16) | 4.00 (0–11) | 3 (−9–4) | <0.01 | 7.50 (0–20) | 5.00 (0–19) | −1.00 (−13–3) | .003 | .679 |
IMTGr: The standard pulmonary rehabilitation plus inspiratory muscle training group; PRGr: The standard pulmonary rehabilitation group. IPAQ-SF: International physical activity questionnaire short-form, SGRQ: Saint George Respiratory Questionnaire, FSS: fatigue symptom scale, HADs: hospital anxiety and depression scale.
In the assessment conducted at the end of the rehabilitation program, intragroup changes in the IMTGr showed an increase in 6MWT distance, FVC, FEV1, all peak mouth pressure measurements, peripheral muscle strength, and physical activity level scores, except for the IPAQ-SF vigorous subcategory. Furthermore, there was a decrease in mMRC dyspnea, FSS fatigue, anxiety, and depression levels. Fatigue level was higher in baseline scoring in PRGr. At the end of the program, it dropped from 45 to 29 in IMTGr and from 54 to 40 in PRGr. Although baseline levels were different, the groups were similar at end-of-program evaluation (Tables 2 and 3).
In contrast, intragroup changes in PRGr showed improvements in 6MWT distance, peripheral muscle strength, and only MEP among maximal mouth pressure measurements. PRGr also demonstrated increased scores in all IPAQ-SF subparameters and a decrease in mMRC, FSS, and depression levels. However, no significant changes were observed in spirometric parameters (Tables 2 and 3).
The IMT group exhibited a median increase in walking distance of 66 meters, whereas the PRGr group showed a median increase of 33 meters (Table 2). Both groups achieved an increase in walking distance above the MCID (25m) value; however, the increase in walking distance in the IMT group is significantly greater.30 Despite this, the effect size, as measured by Cohen's d, was d=0.151, indicating a small effect size.
In current literature, respiratory muscle weakness was defined with a cutoff value of 62cmH2O for female and 83cmH2O for male.31 The number of cases with identified respiratory muscle weakness at baseline were 21 in IMTGr and 24 in PRGr. At the end of the program, these numbers were 18 in IMTGr and 21 in PRGr. There was no statistically significant difference between the groups at baseline (p=.140) or at the end of the program (p=.244).
In the intergroup analysis, statistically significant differences were observed in the maximal mouth pressure measurement parameter MIP (p=0.003) in favor of IMTGr. However, no statistically significant differences were observed in other parameter changes (p>0.05) (Tables 2 and 3).
No complications were encountered related to the practices conducted during the assessment and exercise program. But during the 2-month follow-up period, a total of 5 subjects were excluded from the IMTGr, and 6 from the PRGr. Four patients in both groups could not continue the exercise program due to COPD attacks. One participant from IMTGr and two from PRGr expressed their intention to come to the hospital for their final evaluations. The dropout rates in both groups were comparable, with a dropout rate of 16% in IMTGr and 19% in PRGr.
DiscussionThe study investigated whether the addition of IMT to the PR program had any additional impact on program outcomes. The main findings show that IMT does not provide any additional benefit other than increased respiratory muscle strength. The study results revealed that PR prior to BLVR leads to an increase in exercise capacity, peripheral muscle strength, quality of life, and physical activity level, while reducing perceived dyspnea and fatigue. Furthermore, the patients’ psychological well-being experiences a positive impact. Adding inspiratory muscle training to the standard PR program may have a positive effect on respiratory muscle strength and lung volumes. Although the addition of IMT to the PR exercise program did not reach statistical significance overall, an increase in percentages of measured and expected values for parameters such as FVC and FEV1 was observed. Importantly, a statistically significant increase in the measured liter quantity of FEV1 was achieved. Although the increase in FEV1 is modest, given that spirometric values typically do not increase with PR gains and tend to worsen in these patients, it can be concluded that this gain represents a small yet valuable improvement. This study marks the first investigation of the effects of adding IMT to the PR program in emphysema patients eligible for BLVR.
The observed differences between the groups, while expected, are statistically significant within-group changes. Although the increase in 6MWD observed in the PRIMT group compared to the PRGr did not reach statistical significance, the mean increase in the IMT group was 66m compared to 33m in the PRGr group. This indicates a clinically relevant difference exceeding the 25-m minimal clinically important difference. However, this clinically relevant difference has a small effect size, as measured by Cohen's d=0.151. The greater improvement in walking distance observed in the IMTGr could be attributed to enhanced respiratory muscle strength, leading to a reduction in perceived dyspnea levels and potentially resulting in better performance during the tests. This finding aligns with a previous randomized controlled trial involving lung transplant candidates, which also reported a similar pattern of greater improvement in exercise capacity with the addition of IMT to the standard PR exercise program.15 This reference suggests that improved respiratory muscle strength could potentially enhance exercise capacity. However, beyond this article, no other studies have been found demonstrating a direct correlation between IMT and increased exercise capacity specifically in individuals with COPD. Nevertheless, there are indications that IMT may have a positive impact on exercise capacity in other patient populations.32,33 In our study, the increase in inspiratory muscle strength was noted to be 11cmH2O in the group receiving IMT, whereas the median change in this parameter was negative in the group not undergoing IMT. Comparing our findings with previous studies employing similar methodologies, the IMT groups demonstrated increases ranging from approximately 15cmH2O to 19cmH2O,34 while the non-IMT groups showed increases ranging from 9cmH2O to 10cmH2O.35 In the first study, the exercise program was conducted as a supervised inpatient regimen using ergometers. The supervision and the use of ergometers for aerobic training likely contributed to a greater effect on respiratory muscle strength. In contrast, the second study did not include home-based or supervised aerobic training, although IMT was performed under supervision. Consequently, the increase in respiratory muscle strength observed in the second study was less than that seen in our study. Notably, despite the considerably lower median change in respiratory muscle strength observed in the non-IMT group in our study, it is intriguing that no significant difference was observed between the two groups. The positive effect of increased MIP on walking distance may involve mechanisms such as reduced accessory respiratory muscle activity due to strengthened major respiratory muscles, thereby alleviating shortness of breath and fatigue. Our findings are consistent with moderate-certainty evidence presented in the Cochrane systematic review,36 particularly regarding the significant increase observed in MIP in the IMTGr. The Cochrane review suggests a similar trend of improvement in 6MWD following IMT, although not statistically significant. This consistency lends support to the potential benefits of IMT in enhancing respiratory muscle strength and functional exercise capacity in COPD patients. Furthermore, our study contributes to existing evidence by demonstrating the magnitude of change in MIP, thereby enhancing our understanding of the efficacy of IMT interventions in COPD management.
One of the key benefits of PR programs is the reduction in perceived dyspnea and fatigue levels.37 The PR exercise program achieves symptomatic improvement through gains in aerobic capacity, peripheral muscle strength, and a change in the perception of dyspnea.38 In our study, individuals with severe dyspnea perception were included. Similar to the literature, a decrease in dyspnea perception was observed in both groups. The lack of significant differences between the groups in terms of dyspnea perception may be due to the fact that respiratory muscle weakness, one of the causes of dyspnea, is not present in every case. It is observed that the expected MIP values of both groups are above 60%. Additionally, literature reports suggest that the response to IMT tends to be more pronounced in individuals with MIPmax below 60cmH2O.34,35 This information further corroborates our findings and provides additional support for our results.
In PR programs, not all patients may achieve spirometric improvements.39 In cases of advanced respiratory failure and parenchymal damage, obtaining improvements in spirometric values through PR can be challenging. The primary expectation from PR is often symptomatic improvement.40 In our study, there was a statistically significant increase in spirometric values in the IMTGr. However, in the PRGr, no improvement in lung volumes was observed. While there was a slight increase in spirometric values in the IMTGr group, the observed change in FEV1 (delta: 0.03L) was relatively small and below the Minimal Clinically Important Difference (MCID) for FEV1, which is typically considered to be 100ml. Therefore, the improvement in spirometric values is not clinically relevant. The literature presents varying results regarding the effects of PR13,41 and IMT15,42 on lung volumes, with some studies reporting significant changes while others do not. This inconsistency highlights the need for further research to better understand the impact of these interventions on lung function.
In a randomized controlled study investigating the benefits of adding IMT to PR in COPD, it was found that IMT provided no additional benefits, except for an increased MIP.34 Another study, implementing PR with additional IMT for three weeks in COPD cases without inspiratory muscle weakness, reported an improvement trend in dyspnea sensory intensity, particularly in cases with FEV1 values below 50% of predicted. However, IMT showed no impact on dyspnea and functional parameters in COPD cases with a maximum MIP exceeding 60cmH2O.43 In current studies, cut-off points for respiratory muscle weakness based on T-scores≥2.5 SD below the peak mean value were determined to be 62cmH2O for females and 83cmH2O for males for MIPmax.31 In our study, it appears that the majority of cases have respiratory muscle weakness. Moreover, the increase in MIP obtained was somewhat lower compared to existing literature examples.36,44 According to our results, the fact that adding IMT to the program did not make a difference may be due to insufficient training time or the fact that the exercises were performed unsupervised throughout the week, although weekly follow-ups were made.
Psychological issues, such as anxiety and depression, are common in patients with chronic respiratory conditions. A review on the relationship between COPD exacerbations and depression-anxiety identified them as significant risk factors. In a randomized controlled trial exploring controlled breathing techniques in hospitalized COPD patients, respiratory control positively impacted anxiety and depression during exacerbations.45 Preoperative PR, administered for at least 3 weeks to lung transplant candidates, reduced depression levels.39 In another randomized controlled study investigating PR and IMT for terminally ill respiratory patients preoperatively, IMT was found not to provide additional benefits to psychological status, although the overall program improved depression levels.15 In our study, the IMT group showed a statistically significant improvement in anxiety and depression levels, while anxiety levels in the standard PR group remained unchanged. However, not detecting a difference between the groups provides insufficient evidence to reveal the effect of IMT on psychological state.
Our study has several limitations that should be acknowledged. Firstly, ethical considerations regarding the necessity of PR before BLVR precluded the inclusion of a placebo group without an exercise program, which could have provided valuable comparative data. Secondly, the lack of long-term follow-up after BLVR limits our understanding of the sustained effects of the interventions. Due to the problems experienced in health expenses, BLVR procedure could not be performed in our country for a while, and this caused deficiencies in the follow-up of our cases after BLVR. Additionally, the use of the mMRC scale to assess dyspnea levels may be limited in its sensitivity. Employing additional, more sensitive dyspnea scales could have offered a more comprehensive evaluation of outcomes. Another limitation of our study is the underpowering to detect such clinically relevant between-group differences in 6MWD. Although an increase in walking distance above the MCID value was achieved in both groups, no significant difference was observed in the IMTGr group. Additionally a statistically significant difference favoring the IMTGr was observed in the MIP parameter in the intergroup analysis, no statistically significant differences were noted in other parameter changes. The fact that IMT was not performed under supervision may have caused this and is a limitation.
ConclusionIn conclusion, our study sheds light on the potential benefits of integrating IMT into standard PR programs, particularly for enhancing respiratory muscle strength. However, it's noteworthy that our findings did not reveal a significant difference between the IMT and PR-alone groups in terms of exercise capacity or other patient-reported outcomes. This suggests that while IMT integration holds promise, its additional benefits over standard PR alone may not be statistically significant based on our study results. Nonetheless, our study underscores the positive effects of PR on the clinical status of BLVR-eligible patients, consistent with existing literature. This reaffirms the value of PR as a standalone intervention in optimizing patient outcomes in this population. Furthermore, our results emphasize the importance of PR as a precursor to BLVR procedures, indicating its role in optimizing patient outcomes. Nevertheless, it's important to acknowledge the limitations of our study, particularly its ability to detect significant differences between groups. Therefore, further research with larger sample sizes is warranted to fully elucidate the potential benefits of IMT integration and PR preceding BLVR. Such research could provide valuable insights into optimizing patient care and treatment strategies.
Registration number: NCT05540054.
Study locationThe study was carried out at Yedikule Chest Diseases and Thoracic Surgery Training and Research Hospital.
Statement of ethicsThis study protocol was reviewed and approved by the Ethics Committee of the Yedikule Chest Diseases and Chest Surgery Education and Research Hospital, approval number 2022-238 (05/12/2022).
FundingNone.
ContributorsEsra Pehlivan conceived and designed the study, supervised patient training, interpreted the data, and drafted the manuscript. Zeynep Betül Özcan and Fulya Senem Karaahmetoğlu conducted the patient evaluations and exercises. Erdoğan Çetinkaya, Mustafa Çörtük, and Halit Çınarka contributed to the study's design, coordination, and manuscript review.
Conflict of interestThe authors declare that there is no conflict of interest.
The author(s) thank to their gratitude to all the patients who participated in the study and to the clinical staff involved in the conduct of the research.