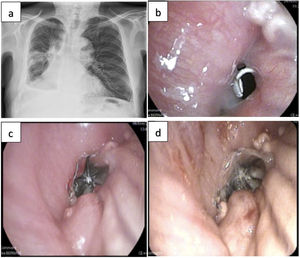
Our patient was a 74-year-old male, operated 10 months previously for epidermoid carcinoma with a right bilobectomy (middle lobe and right lower lobe) with double thoracotomy. Fifteen days after surgery, the patient developed empyema, with evidence of a fistula due to dehiscence of the bilobectomy suture, which required 2 new interventions that did not achieve closure of the fistula. A third surgery in this situation involved a high surgical risk and offered very little chance of success. Since at that time the patient showed no signs of endobronchial infection and the fistula orifice measured>1cm on endoscopy, the placement of the largest commercially available intrabronchial valve (9mm) was proposed.1 Anchoring the device was very difficult and, in addition, there was a risk of complication with migration via the patient's thoracotomy (Fig. 1a and b).
(a) Posteroanterior chest X-ray showing post-surgical changes, right hydropneumothorax with air-fluid level at the most basal part of the right hemithorax and right pleural effusion; (b) endoscopic view of the fistula orifice in the central area of the right lower bilobectomy stump; (c) endoscopic view after implantation in the fistula orifice of the 9mm Spiration® Olympus intrabronchial valve; and (d) intrabronchial valve implanted in the fistula orifice after instillation of platelet-rich plasma. Note the surrounding granulation tissue.
One month after the last attempt at surgical closure, the valve was implanted into the fistula orifice under conscious sedation, and correct positioning was confirmed by endoscopy (Fig. 1c).2 Fifteen days after the procedure, an endoscopic revision was conducted, showing that the occlusion was not complete, so we decided to use endoscopy to instill 10ml of platelet-rich plasma over the mucosa bordering the valve. This prompted a fibrotic reaction (Fig. 1d), which facilitated the complete closure of the fistula and the disappearance of the air leak in one week.