Primary pulmonary artery sarcoma (PPAS) is a rare disease with unclear clinical manifestations. Advances in imaging devices have improved diagnostic capabilities, potentially affecting clinical characteristics and overall survival (OS); however, details remain unclear. This study conducted a pooled analysis of case reports and series to analyse the clinical characteristics and OS of PPAS in the era of advanced medical devices.
MethodsData were sourced from PubMed and CINAHL, focusing on studies published between 1 January 2014 and 31 December 2023. The study included patients diagnosed with PPAS, with extracted data covering demographics, diagnosis, treatments, and survival.
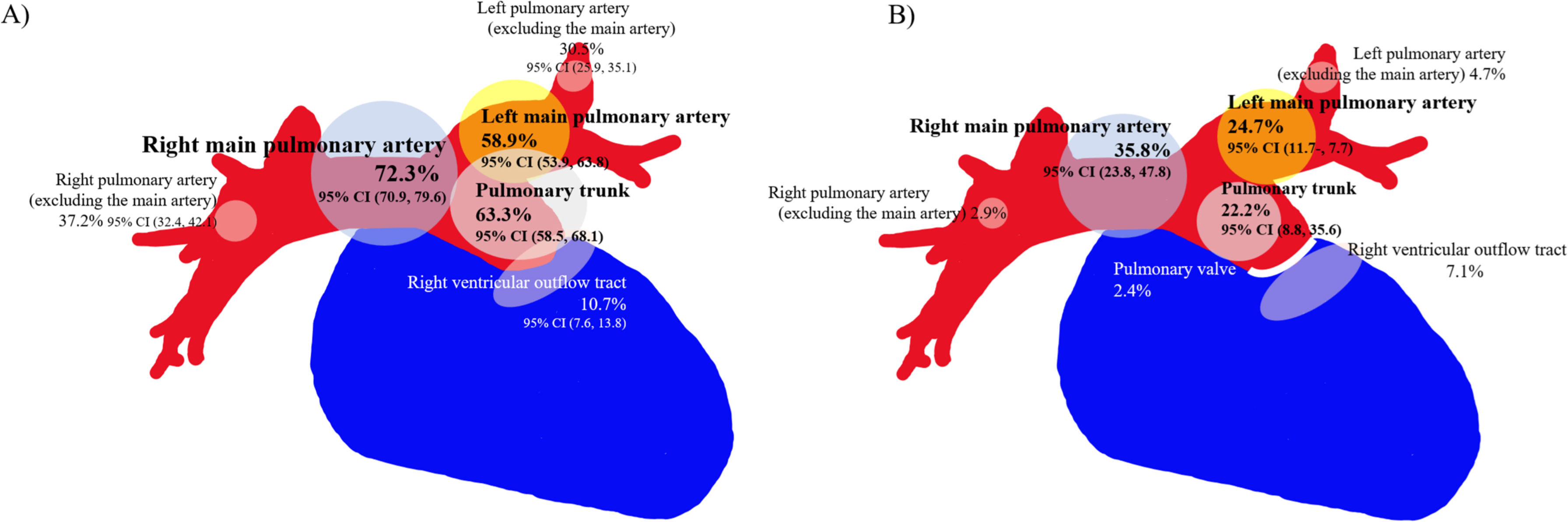
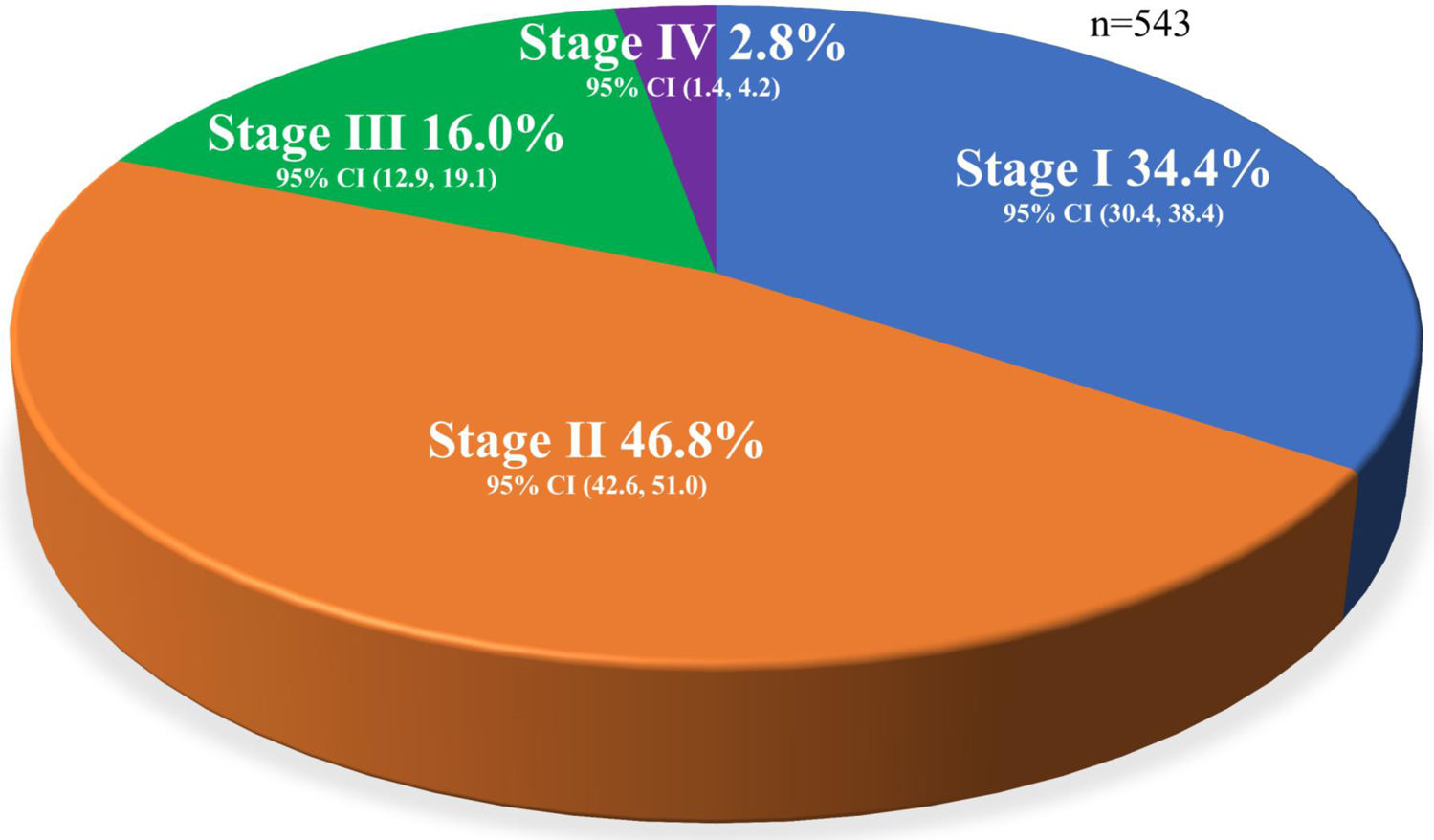
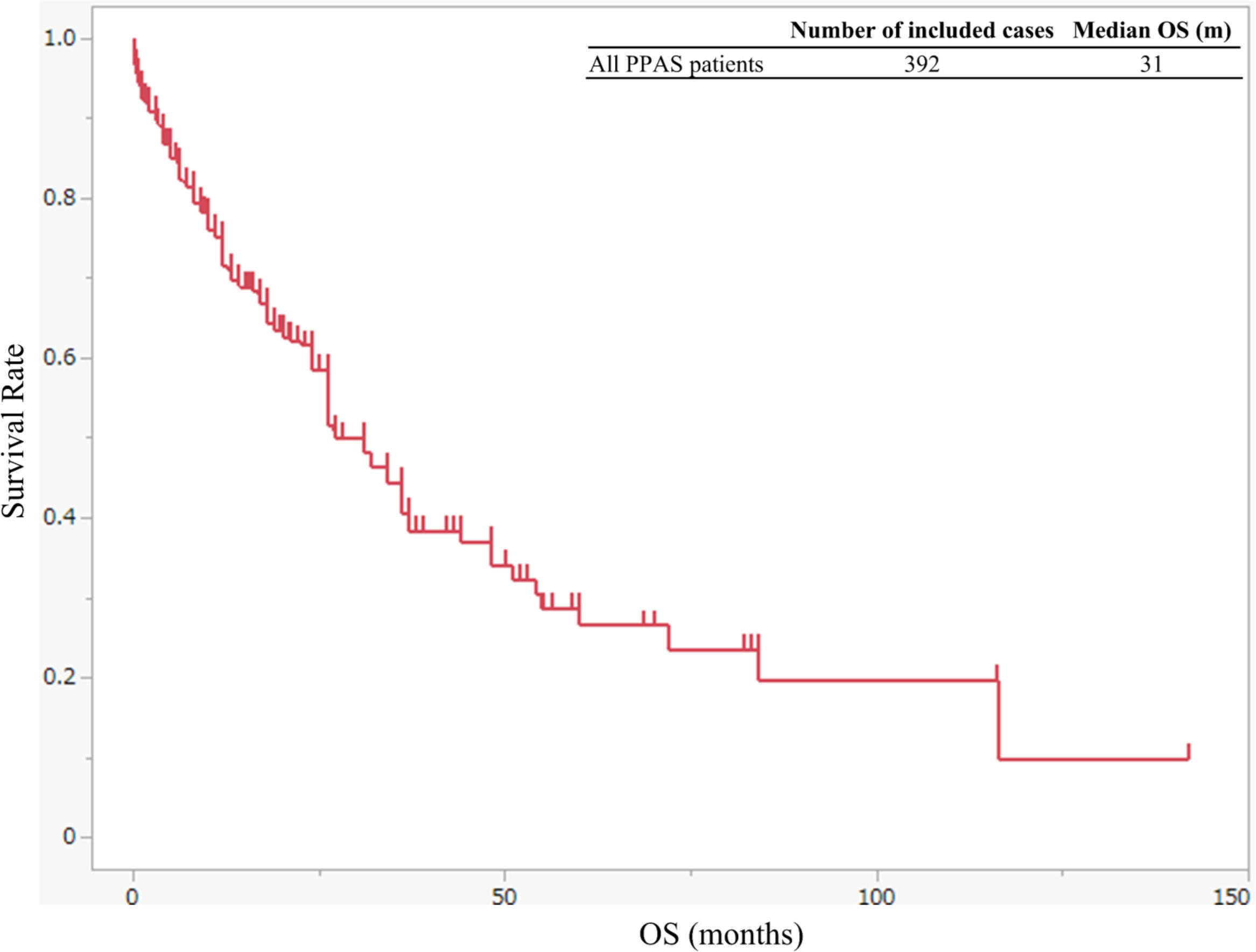
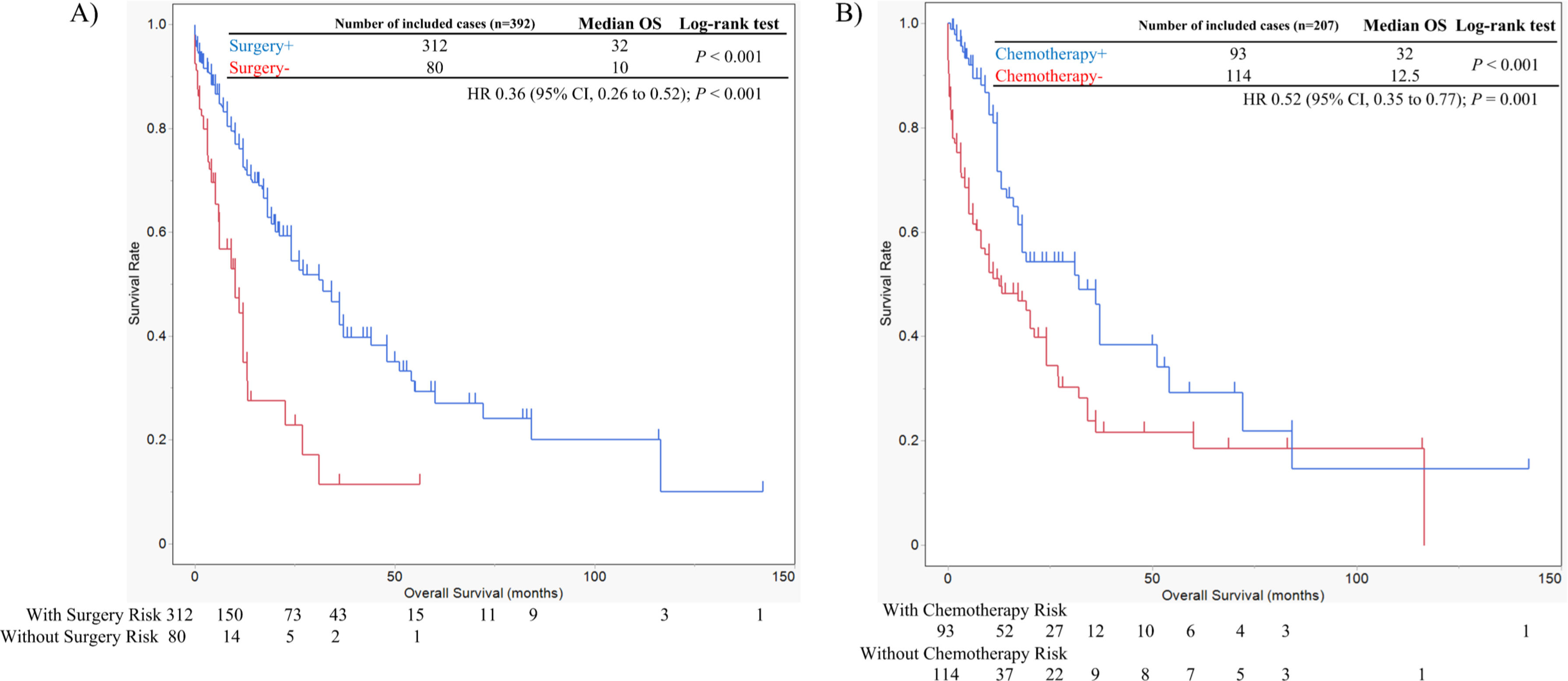
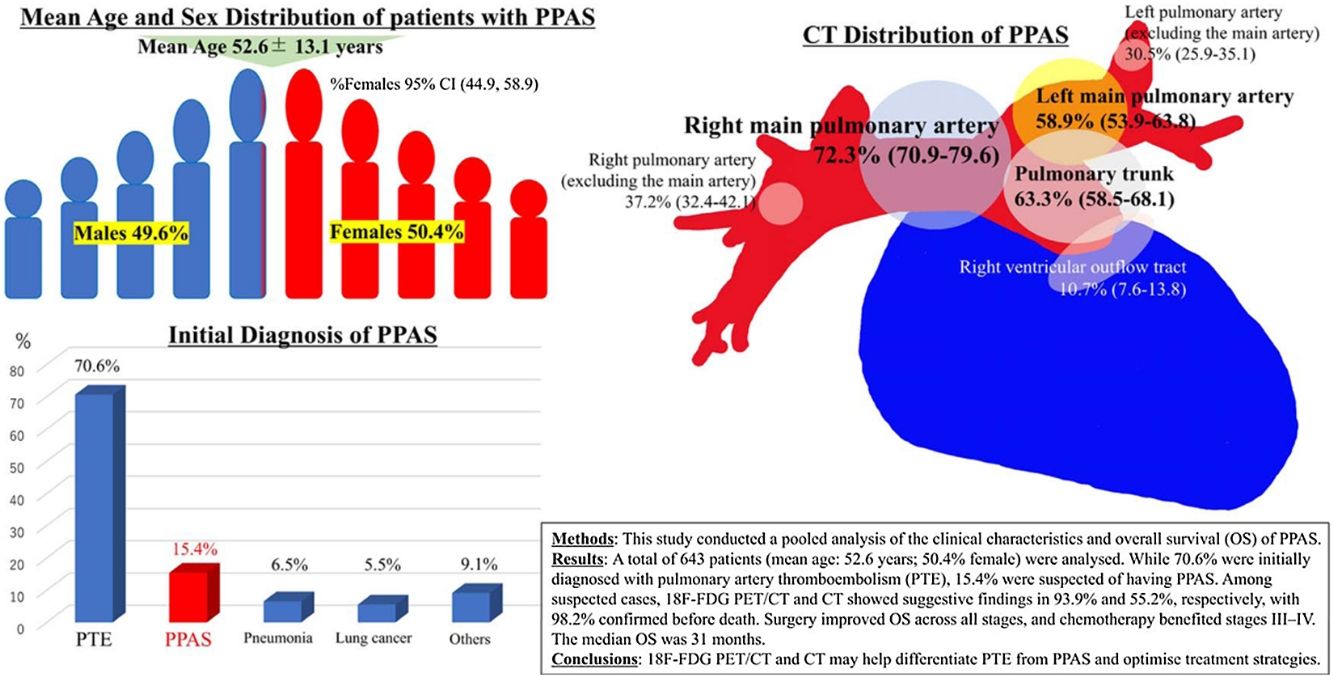
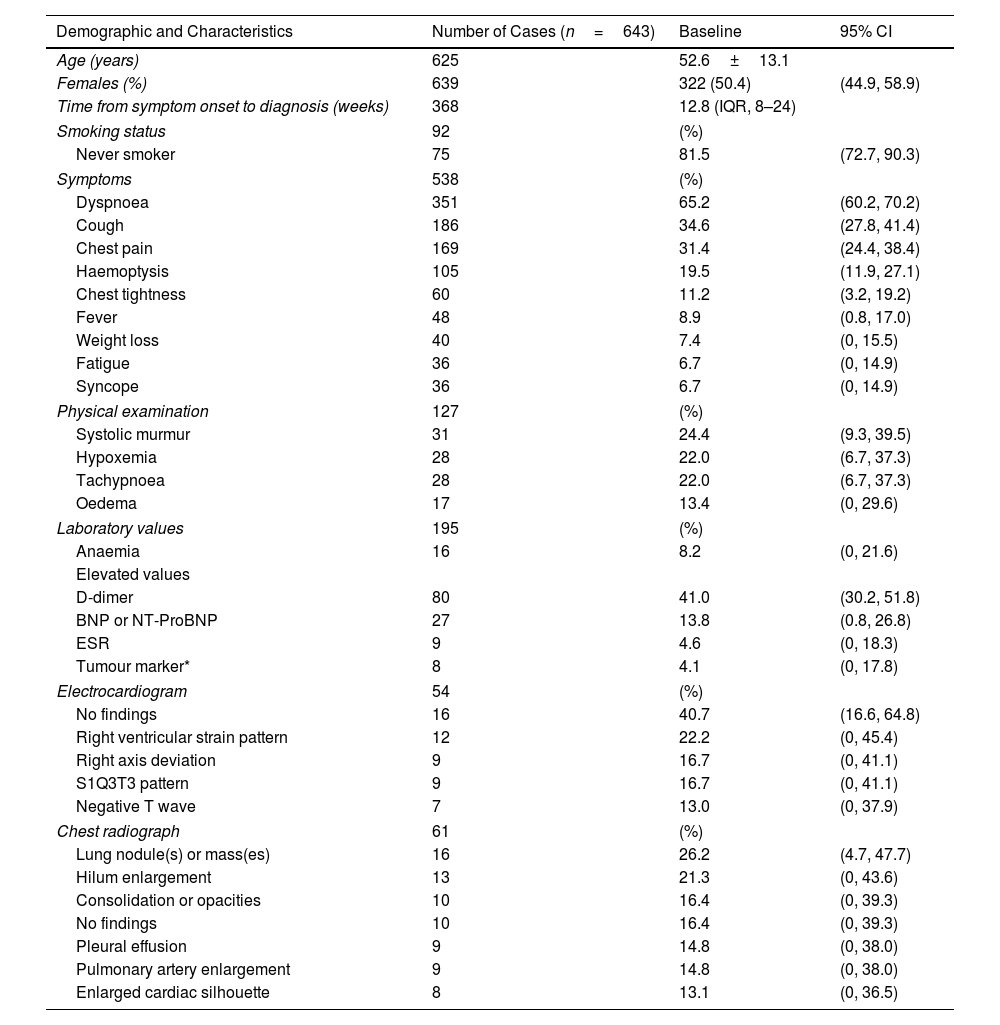
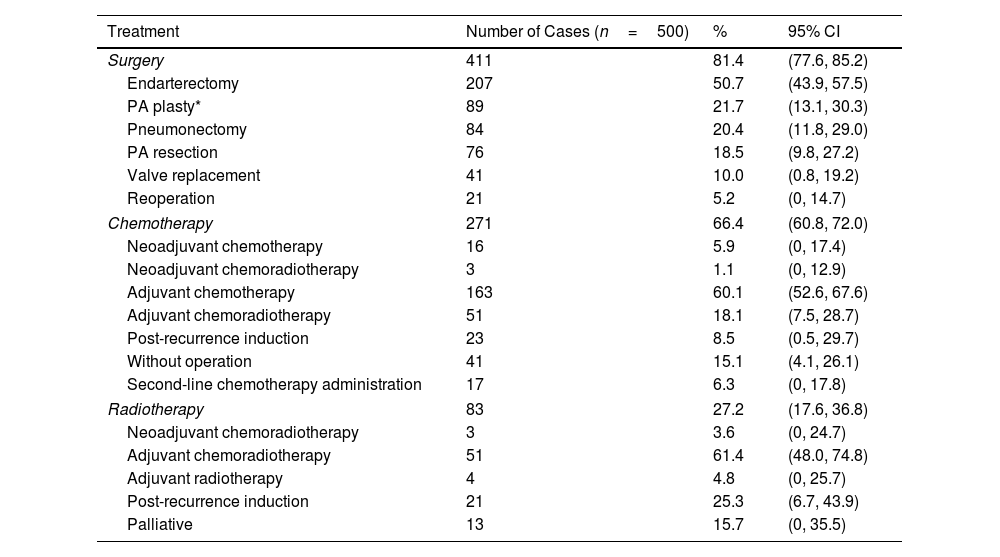
ResultsOverall, 643 patients were included (mean age: 52.6±13.1 years; 50.4% were female). Initially, 70.6% were diagnosed with pulmonary thromboembolism (PTE), and 15.4% were suspected of having PPAS. Among these, 93.9% and 55.2% showed suggestive findings on computed tomography (CT)-integrated positron emission tomography with 2-deoxy-2-18F-fluoro-d-glucose (18F-FDG PET/CT) and CT, respectively, with 98.2% confirmed before death. The right main pulmonary artery was the most affected site on CT (72.3%). Surgery and chemotherapy were performed in 81.4% and 66.4% of patients, respectively. The median OS was 31 months, with surgery extending OS across all stages and chemotherapy benefiting stages III–IV. Longer OS was achieved in patients who underwent complete surgical resection.
Conclusions18F-FDG PET/CT and multi-detector-row CT can differentiate PTE from PPAS. These medical devices may contribute to improved OS.