Emergency medicine and critical care have evolved dramatically in the last 50 years. Most patients are discharged quickly and recover within the first days after ICU admission.1 However, approximately 7–43% have a slow progression and develop a chronic critical illness (CCI).2 This condition constitutes a syndrome of persistent multisystem dysfunction, which arises when critical care interventions cannot return patients to good health and function,3 leading to worse outcomes after discharge.2,4 For instance, patients with CCI have in-hospital mortality of up to 60%, and in those discharged alive, mortality rates are up to 50% at six months.3–5 Furthermore, survivors with CCI develop permanent disabilities and sequelae (cognitive, psychiatric, or physical dysfunctions). This situation affects patients’ quality of life, including their families, defining the post-intensive care syndrome (PICS).3,5,6 Risk factors for developing CCI include age, comorbidities (i.e., hypertension and diabetes), prolonged mechanical ventilation, surgical interventions, and multi-organ failure.4,6
The COVID-19 pandemic challenges critically ill patients worldwide. Limited social support (restricted visits, intrafamily infection, among others), prolonged mechanical ventilation (MV), and reduced physical therapy during hospitalization may contribute to CCI in patients with COVID-19.7,8 Nevertheless, the influence of COVID-19 on CCI is unknown. This study aimed to estimate the association between COVID-19 and CCI, including 90-day mortality.
A prospective cohort study included adult patients admitted to ICU in two tertiary centers in Cartagena, Colombia, between July and November 2020. We compared COVID-19 versus non-COVID-19 patients using multiple logistic regression and survival analyses. The two primary outcomes were progression to CCI and 90-day mortality, and the secondary outcomes were patient independence, prolonged oxygen requirements, and hospital readmission.
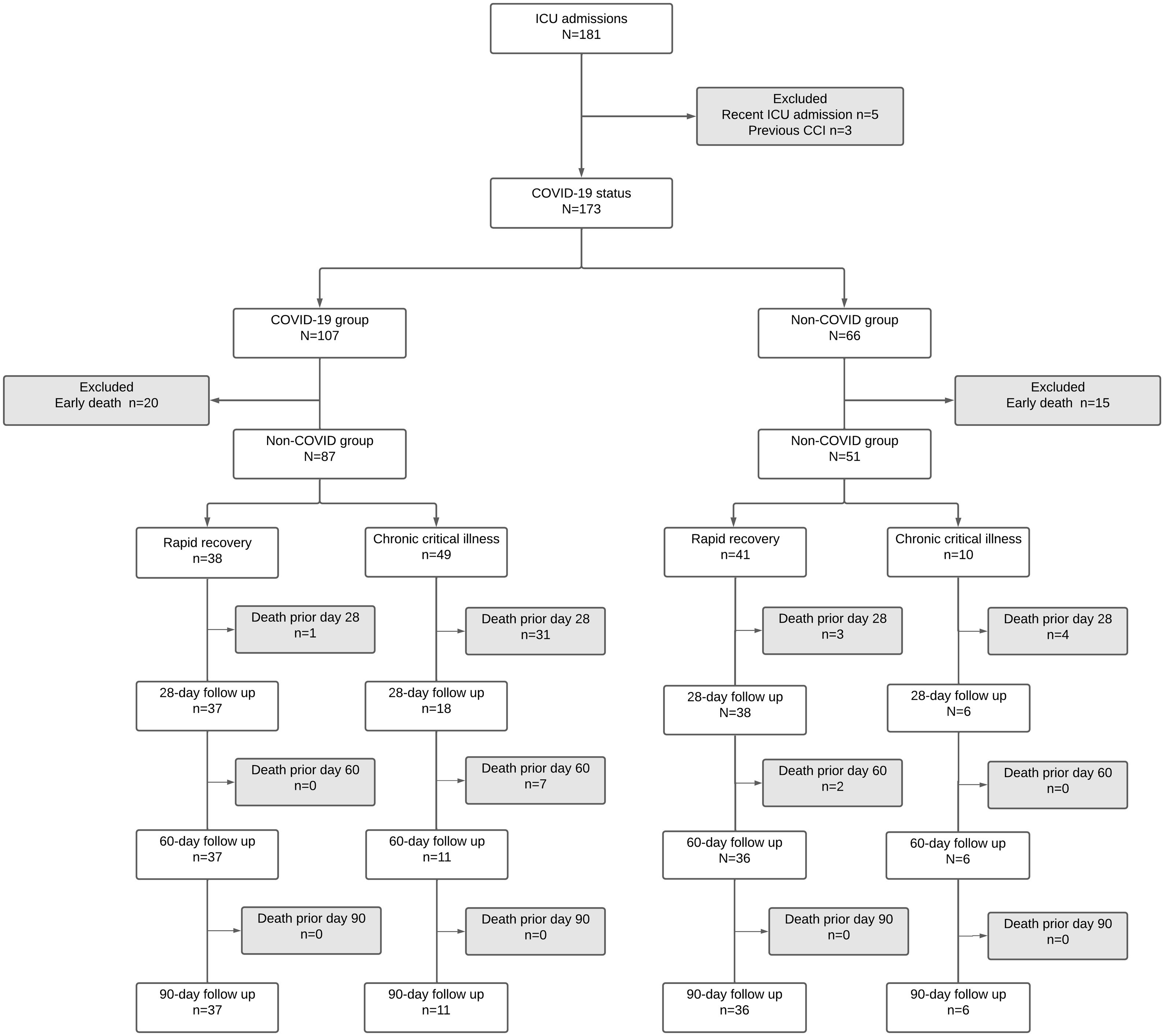
We excluded patients with an ICU admission in the previous 90 days, CCI history, and early death (death within the first eight days following admission). We classified patients according to COVID-19 status (with positive RT-PCR) into COVID or non-COVID groups.
The final analysis included 138 patients, 87(63%) with COVID-19 and 51(37%) without COVID-19 (Fig. 1). The frequency of chronic critical illness was 42.7%(59/138), with a higher rate in the COVID group (83.1% [49/59] vs. 16.9% [10/51] in the non-COVID group; p<0.001). After the adjusted analysis, COVID-19 (OR 5.23; 95% CI 1.83, 14.95) and SOFA score (OR 1.38; 95% CI 1.11, 1.74) were independent predictors for chronic critical illness. The in-hospital mortality was 34.8% (48/138), with higher 90-day mortality in patients with chronic critical illness and COVID-19 (79.2% [38/48] vs. 12.2% [111/90] in non-COVID patients; p<0.001). Patients with chronic critical illness had higher dependency levels at 90 days (29.4%, 5/17 vs. 0%; p<0.001) and requirements of supplementary oxygen (23.5%, 4/17 vs. 2.7%, 2/73; p<0.001). The readmission rate was 6.7%(6/90), including 5(5.4%) patients with ICU readmission
We found that CCI is common in the ICU, mainly in critically ill COVID-19 patients. Additionally, CCI was associated with increased in-hospital mortality. Likewise, CCI was associated with higher ICU and hospital stays, duration of mechanical ventilation, and a bad disposition. COVID-19 and CCI were associated with higher hospital mortality on Day 90 of follow-up; however, only CCI increased mortality in this cohort after adjustments in survival analysis.
CCI is associated with increased morbidity and mortality in the short and long term. This result is consistent among studies, although they differ in follow-up periods in COVID and non-COVID settings.9–13
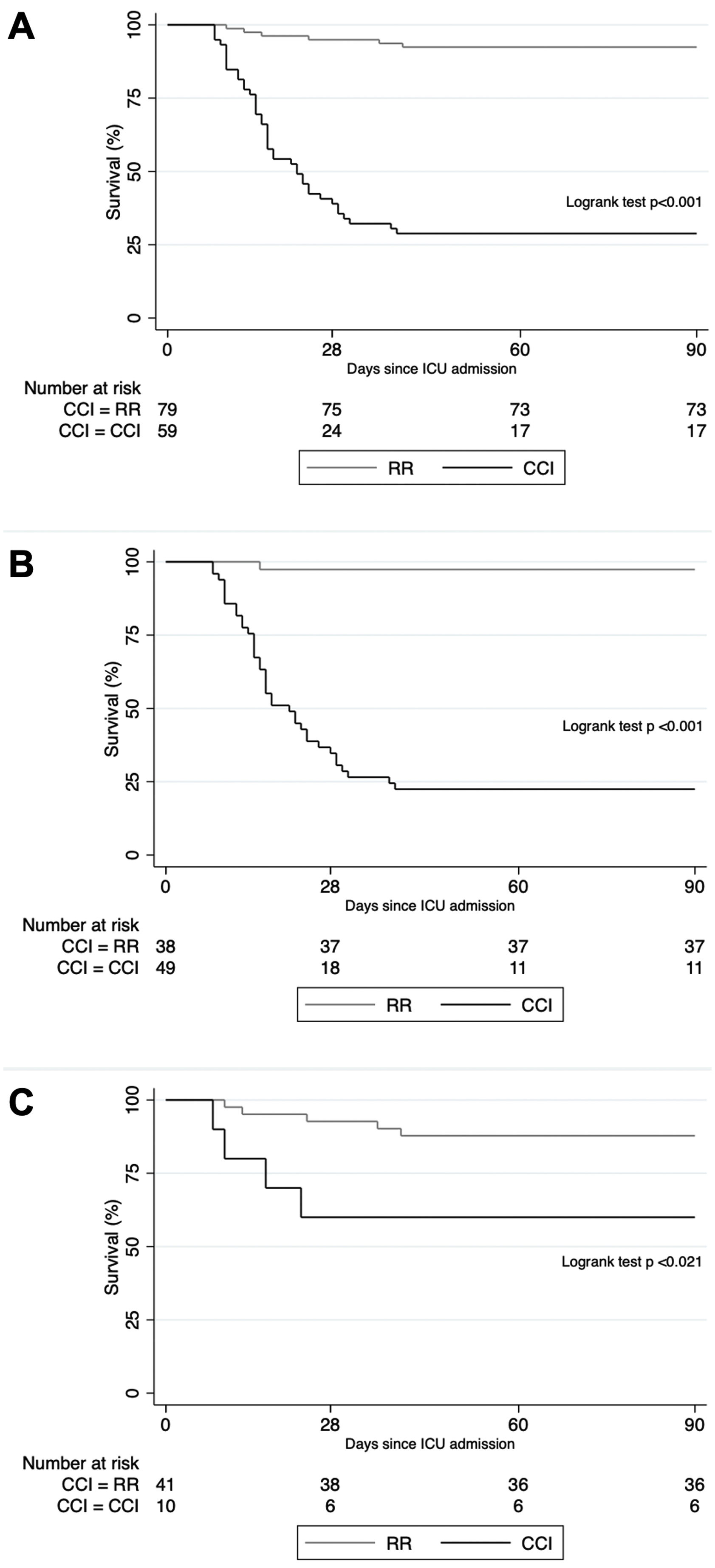
The Kaplan–Meier survival analysis showed that in the complete sample (p<0.001), non-COVID group (p=0.021), and COVID group (p<0.001), survival was lower in those participants with CCI. Differences in survival were more comprehensive in the COVID group than in the non-COVID group (Fig. 2).
Given the heterogeneity of CCI definitions, its prevalence is variable. Two large national series reported a prevalence of 7.6% and 9%,4,14 but others described 33–49%,14,15 close to 42.7% in our study. Studies with septic patients reported a higher prevalence.16
In addition, the high frequency of COVID-19 in our study explains the high prevalence of CCI during the ICU stay and adverse outcomes in the medium and long term. Data related to the long-term morbidity of COVID-19 in patients admitted to the ICU are currently under analysis. An alternative diagnosis, designated as “post-COVID-19 syndrome” or “long COVID,” defines severe respiratory sequelae and symptoms such as fatigue or muscle weakness, sleep difficulties, psychiatric and neurological complications persisting after 12 weeks of acute infection and not explained by.11,12,17 Before the pandemic, some authors defined this new entity as PICS depending on physical, cognitive, and mental health impairment, assessed with a different diagnostic tool depending on the category evaluated.18 Other studies have considered the presence of PICS in the context of COVID-19.19 A recent study reported that 95% of COVID-19 ICU survivors fit the diagnostic criteria for PICS.18 Even though these conditions are essential factors for the patient's quality of life, these studies did not assess variables defining CCI or short-term mortality and its relationship with COVID-19. Identifying “long COVID-19” phenotypes must elucidate the pandemic's impact on CCI.
The occurrence of a CCI involves multiple risk factors, including APACHE II, SOFA, the presence of severe sepsis or septic shock, chronic obstructive pulmonary disease (COPD), heart failure, neurological conditions, the need for vasopressors, renal replacement therapy, parenteral nutritional support, and the need for tracheostomy.3,8,13 However, in the present study, only COVID-19 and the SOFA score were associated with CCI in multivariate analysis. The high rate of an independent population before admission to the ICU further supports the impact of COVID-19 on critically ill patients. In general, patients with COVID-19 in the ICU have high requirements for MV, tracheostomy, hemodialysis, and other interventions associated with worse outcomes, including higher mortality, more extended ICU stay, and a higher frequency of pressure ulcers.17,20
Regarding our secondary outcomes, we found an increased need for hospitalization in chronic care centers in the CCI group at the end of the 90-day follow-up. The literature reporting hospitalization in chronic care units describes a higher prevalence of a “bad disposition” in surviving patients. This finding is essential due to the increased cost of medical care after CCI reported in the literature, ranging from US$2.3 to US$26 billion in expenses related to hospital costs alone, with higher expenses in CCI patients.3,5 However, the combined economic burden of CCI and COVID-19 is still unknown.
To the authors’ knowledge, this is the first prospective study including patients with CCI and RR who survive critical care in the context of COVID-19 (Roedl). However, the heterogeneity of definitions for CCI may hinder the comparability of our findings. Despite this, the criteria used are similar to those of more extensive international CCI-related studies.3,5 Additionally, the study was conducted during the first COVID-19 pandemic peak, before vaccination programs in Colombia, impacting the increased prevalence of CCI in our findings. However, the impact of COVID-19, even in mild presentations in the postvaccination era, has yet to be elucidated. The burden of COVID-19 on the CCI, including the effect of vaccination, should be further studied.
This study shows that CCI is common in our ICU. Additionally, SOFA and COVID-19 were independent risk factors for CCI. Finally, the combination of CCI and COVID-19 was associated with worse clinical outcomes, including mortality and morbidity, at the 90-day follow-up.
Financial supportThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.