Electromyography (EMG) is a technique that enables recording the electrical activity derived from muscle fibers, obtaining information for the study of neuromuscular disorders. Although considered a safe technique, monitoring through intramuscular needle electrodes carries potential risks, including pain, bleeding, and infection. When needle exploration is performed in muscles adjacent to the pleura, there is a risk of pneumothorax.1 We present a case of this rare adverse effect, which led to a referral to our center due to a distracting symptom.
A 42-year-old woman with a past medical history of scoliosis surgery was referred from a private center for urgent endoscopy due to suspicion of esophageal impaction. The patient presented in the emergency department (ED) reporting chest pain in the last 24h. The pain began suddenly in the right hemithorax associated with mild dyspnea, coinciding with the ingestion of ham and potatoes. After a few minutes, it partially subsided, presenting a pain of less intensity that increased with inspiration, unrelated to swallowing. Upon arrival to the ED, she no longer presented dyspnea, dysphagia or other accompanying symptoms. She added that the previous day she had undergone an EMG in another health center, of which she did not provide a report.
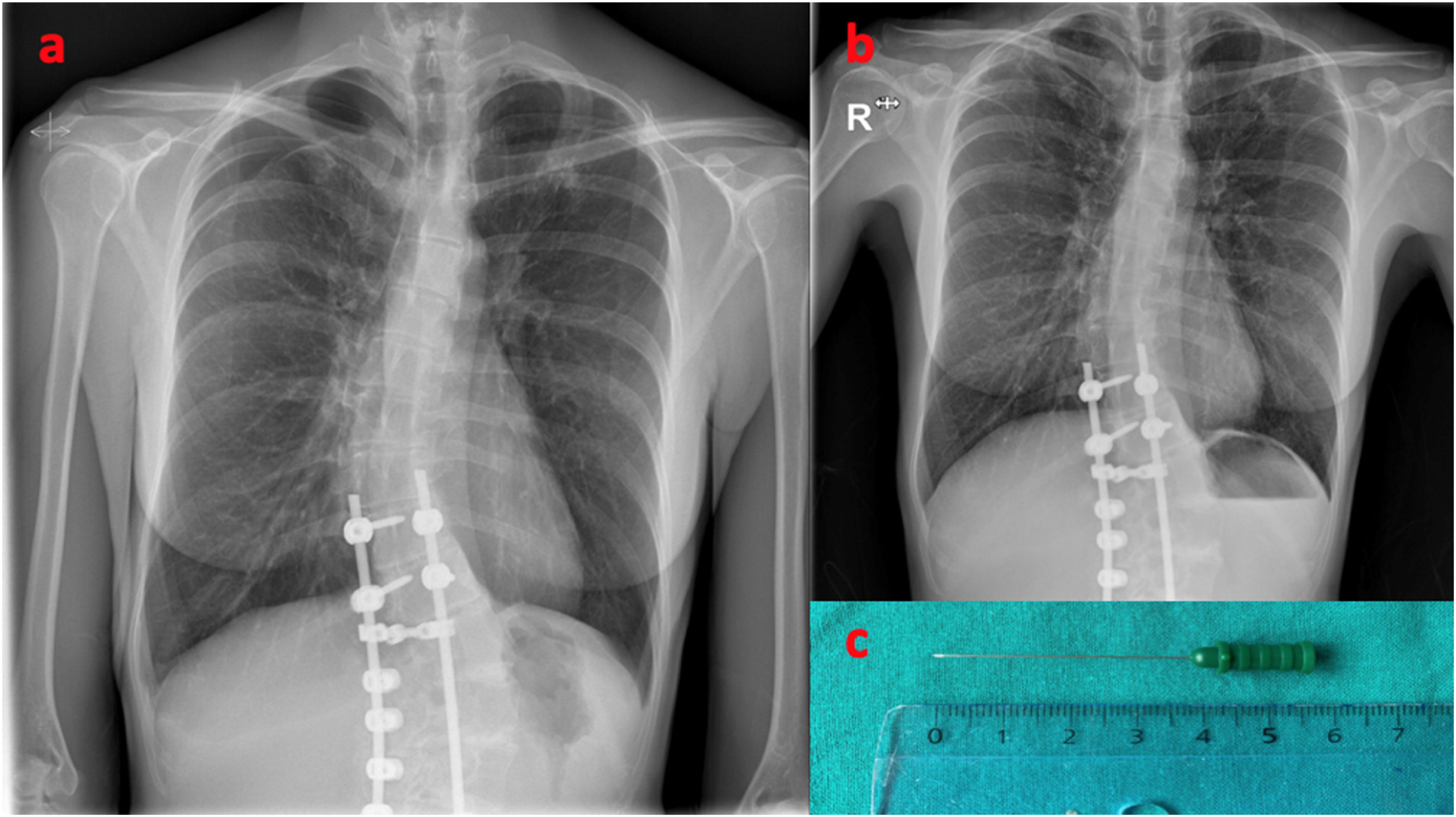
Her vital signs were as follows: blood pressure, 121/81mmHg; heart rate, 65bpm; temperature, 36°C and oxygen saturation 99% on room air. Lung auscultation showed mild hypoventilation in the right lung apex, without palpation of subcutaneous emphysema. An ECG showed normal sinus rhythm. The patient's chest X-ray (Fig. 1a) revealed a pneumothorax smaller than 15% in the apex of the right lung. The patient was questioned about the previous day's test, admitting needle puncture of the right periscapular muscle in the electrophysiological examination.
The thoracic surgeon was consulted, who advocated conservative approach with follow-up X-ray at 24h, showing no increase in pneumothorax. After 10 days, a new chest X-ray was performed (Fig. 1b), verifying radiological resolution. At the follow-up visit, the patient provided an EMG report confirming the exploration of the serratus anterior muscle (Fig. 1c).
The incidence of iatrogenic pneumothorax has recently increased due to the development of invasive procedures for multiple diagnostic and therapeutic purposes.2–4 Pneumothorax secondary to accidental puncture of the pleura by an EMG needle is a highly infrequent complication. In the study by Kassadjian et al.5 seven cases of pneumothorax were found out of the 64,490 EMGs that were evaluated. All patients were symptomatic within 24h of the procedure. Five of them presented a volume equal to or greater than 20%, requiring the placement of a drainage tube. The muscles most associated with pneumothorax under these circumstances are the serratus anterior, rhomboid, and diaphragm.5 The use of ultrasound-guided punctures allows the correct identification of the muscles and pleural space, and may reduce its incidence.1
We highlight the importance of a thorough history and physical examination, especially in patients undergoing invasive diagnostic techniques in the thoracic region, where emergency physicians must consider the possibility of pleural damage as a potentially serious complication.
Conflict of InterestsAuthors declare no conflict of interests for this article.