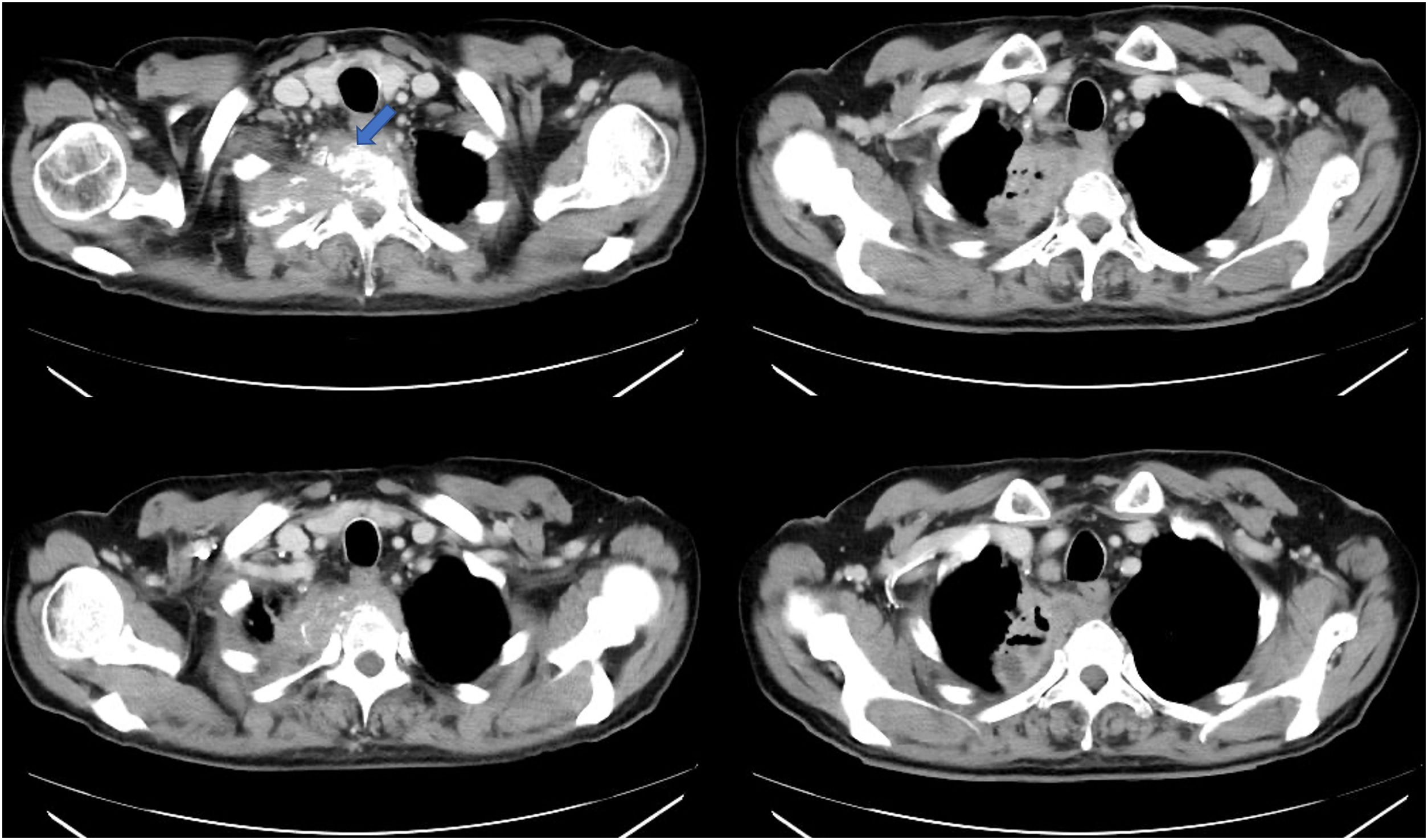
A 59-year-old man with no relevant medical or surgical previous history was admitted in the Emergency room referring hemoptysis and pleuritic chest pain radiating right arm and back, he also mentioned weight loss and night sweats in the previous month. Thoracic CT showed a necrotic-caved mass invading apical and mediastinal pleura, associating second rib and D2 vertebral-body osteolysis with medullary canal invasion (Fig. 1), suggesting Pancoast or superior pulmonary sulcus tumor.
Sputum samples were collected at first, endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) was performed to obtain tissue samples from the mass using endobronchial ultrasound. Pathological analysis of these samples and bronchoalveolar lavage described no signs of neoplasia infiltration or malignancy cells. Bronchoalveolar lavage was also remitted to Microbiology laboratory where bacilloscopic studies did not reveal acid-fast bacilli.
The Microbiology department reported both Nocardia abscessus and Mycobacterium tuberculosis complex isolation in sputum and bronchoalveolar lavage respectively, so intravenous antibiotic therapy with amoxicillin–clavulanic and amikacin, as well as quadruple anti-tuberculous therapy were initiated.
An immunosuppression study was performed in which underlying neoplasms, chronic infections (HIV, HCV, syphilis, etc.) and primary immunodeficiencies were ruled out. Combined intravenous antibiotic therapy was maintained for two months and completed eight months length with oral amoxicillin–clavulanic monotherapy. Anti-tuberculous treatment was also maintained for eight months meanwhile the patient went under several radiological controls showing progressive decrease and disappearance of the mass. Sputum samples were collected monthly with no further isolations.
Cancer, mostly non-small cell lung carcinoma, causes Pancoast tumor in 95% of cases, however, conditions such as Nocardia or Tuberculosis infections are described as unusual etiologies of this entity.1 Previous lung parenchymal disruption in patients with chronic lung disease is a common predisposing condition in cases of pulmonary nocardiosis. As pulmonary tuberculosis being one of the leading causes of this disruption and bronchiectasis development, patients with pulmonary tuberculosis may have an increased risk for nocardiosis.2
Nocardia and Tuberculosis pulmonary coinfection is an extremely rare condition that has been eventually described in patients with HIV infection, or another underlying grade of immunosuppression, living in regions with high tuberculosis incidence.2 Due to this rareness, no treatment strategy has been established, but combined antibiotic and anti-tuberculous therapy has been reported effective.3 As a pulmonary severe infection both antibiotic and anti-tuberculous therapy should be maintained from six months to twelve months and radiological test and cultures of sputum samples may be performed in order to prove recovery and microbiological cure.4
Patients with Tuberculosis and Nocardia mixed infection must be always studied in order to rule out acquired (HIV infection, cancer) or congenital immune-deficiency, as both infections, especially nocardiosis, are eventually found among those with some grade of immunosuppression.5
This is the first case report acknowledged of Nocardia and Tuberculosis coinfection mimicking a superior pulmonary sulcus tumor in an immunocompetent host. This case illustrates the importance of an adequate differential diagnosis over patients with thoracic and lung masses, reminding us that other conditions, such us infections or granulomatous diseases, must be always taken into consideration.
Funding sourcesNone.
Conflicts of interestThe authors have no conflict of interest to declare.
We would like to thank Dr. Pascual Val Adán for his teaching and support.