Primary tracheal tumours are uncommon, with an incidence of 0.2/100000 population.1 In adults, only 10%–20% of tracheal tumours are benign, including chondroma, papilloma, fibroma, haemangioma. Tracheal lipoma is extremely rare and only few cases have been reported in the literature.1–8 This tumour typically presents with non-specific symptoms and signs as dry cough and wheezing and infrequently with respiratory failure. Its resection is required and it can be achieved by both endoscopically and open surgery.
Here we report the case of an incidental tracheal lipoma successfully treated by rigid tracheobronchoscopy.
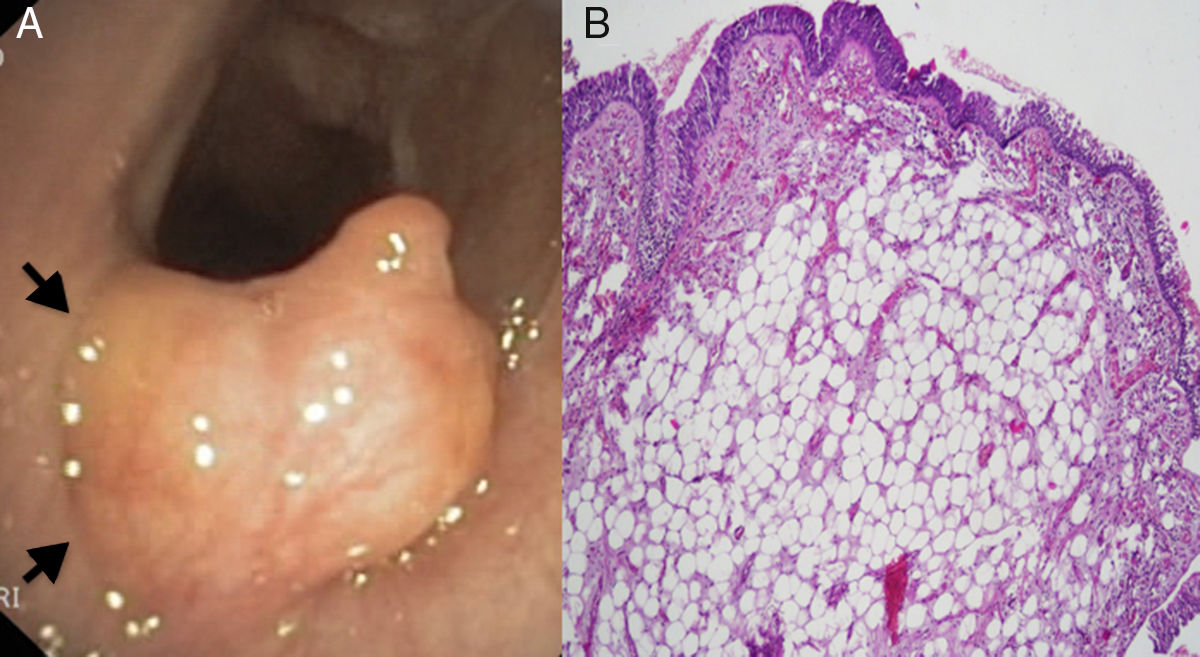
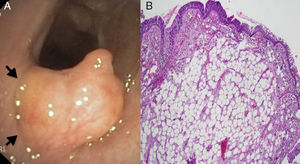
A 79-year-old male, former smoker with a history of arterial hypertension, right Meckel's cave meningioma and previous retroperitoneal non-Hodgkin's lymphoma, was admitted to our Thoracic Surgery Unit to evaluate a broad-based polypoid tracheal lesion incidentally discovered during the endoscopic CO2 laser cordectomy performed for an in situ squamous cell carcinoma of the left true vocal cord. The patient reported no cough, dyspnoea, wheezing, stridor or haemoptysis. The physical examination was unremarkable. Chest X-ray was normal. Computed tomography (CT) scan showed an intratracheal polypoid growth arising from the anterolateral tracheal wall. Flexible tracheobronchoscopy confirmed the presence of a broad-based polypoid lesion growing from the anterior tracheal wall, in correspondence of the IV–V tracheal rings. The tumour was about 7mm in diameter with a smooth and yellowish surface. It obstructed about 50% of the tracheal lumen (Fig. 1A). The uneventful endoscopic biopsy revealed chronic tracheitis with squamous hyperplasia and mild dysplasia. Despite the benign histological finding and the patient's asymptomatic status, we decided to remove the lesion because of the recent history of glottis carcinoma. The patient underwent tumour excision with diode laser by rigid tracheobronchoscopy. Complete clearance of the airways was obtained. The postoperative course was unremarkable. Histopathological examination revealed a subepithelial lipoma (Fig. 1B). The flexible tracheobronchoscopy follow-up revealed no local recurrence 12 months after the endoscopic treatment.
(A) Flexible tracheobronchoscopy showing a well defined, yellowish, smooth, lobulated, broad-based tumour rising from the mucosal layer (arrows) of the anterior tracheal wall. (B) Microscopic image of the resected specimen showing a not encapsulated tumour localized in the subepithelial layer, composed of mature adipocytes without cellular atypia (hematoxylin-eosin).
Airways lipoma is a remarkably rare tumour, representing only 3.2%–9.5% of tracheobronchial tree benign neoplasms.3 It primarily involves the main stem bronchi and, infrequently, the tracheal wall. In a series reported by Politis et al only 3 of 50 tracheobronchial tree lipomas were located in the trachea.5 Lipoma arises from the submucosal fat of the tracheobronchial tree and can extend between the cartilage rings into the peritracheal tissue.4
Patients with tracheal lipoma are primarily middle-aged men.3 They are generally symptomatic, presenting with dry cough, wheezing, dyspnoea and stridor. Haemoptysis is unusual because lipoma is not typically ulcerative. These symptoms usually occur late, when the tracheal lumen is occluded by 50%–70%, and they are frequently misinterpreted as asthma or chronic bronchitis. To date, ours is the second case of asymptomatic tracheal lipoma reported in the literature. The previous one was occasionally discovered during a flexible tracheobronchoscopy performed for a solitary pulmonary nodule.3
Regarding radiological imaging, chest X-ray is usually normal, but it is always performed in presence of respiratory symptoms to exclude other differential diagnosis.4 Chest CT scan or chest magnetic resonance imaging, with their high specificity for fat, should be suggested for the diagnostic management of tracheal lipoma since they can give information not only about the location and the nature of this endotracheal growth but also about its extension into the peritracheal tissues.9
The gold standard in the diagnosis of tracheal lipoma is the flexible tracheobronchoscopy. Macroscopically airways lipoma looks as a yellowish, lobulated, pedunculated or broad-based, fatty submucosal growth. Preoperative biopsy by flexible tracheobronchoscopy is still controversial. Some authors believe that a preoperative histologic diagnosis is essential for an accurate treatment planning. Conversely, others consider it a dangerous manoeuvre because of the risk of bleeding with consequent airways occlusion.2–4 Additionally, endoscopic biopsy sometimes results in a non-diagnostic histopathological report due to the tracheal lipoma capsule resistance to the biopsy forceps.10 In our opinion, if the bleeding risk is acceptable, a biopsy should be performed preoperatively by flexible tracheobronchoscopy in order to exclude other differential diagnosis like lipomatous hamartomas. Otherwise, it should be performed together with the tumour resection via rigid tracheobronchoscopy.
The treatment of tracheal lipoma is its excision by tracheobronchoscopy or, in select cases, by tracheal resection with end-to-end anastomosis. The endoscopic excision can be successfully performed with laser or electrosurgical snaring forceps, cryotherapy or argon plasma coagulation via flexible or rigid tracheobronchoscopy.1,3,7,8 The choice of one of these endoscopic techniques should be left to the operator's experience and preference. So far, no local recurrence has been reported after endoscopic treatment. Only few cases of tracheal lipoma have been treated by tracheal resection and reconstruction.2,4 In these cases preoperative biopsy was not performed and the tracheal lipoma appeared as a wide broad based polypoid tumour, with extension beyond the tracheal wall only in one case.2,4 Despite full and uneventful recovery in all published cases, tracheal resection is generally related to an overall morbidity and mortality of 12%–44% and 0.2–4% respectively.11,12 Moreover, about 5% of patients with postoperative complications requires tracheostomy or further surgical procedure to treat post-operative stenosis or anastomotic dehiscences.12 Thus, surgical resection should be performed only in selected cases.
Tracheal lipoma is an infrequent finding that may be considered as one of the possible alternative diagnoses of treatment-resistant asthma and chronic bronchitis. The endoscopic treatment of tracheal lipoma is effective and safe. It should be recommended as the first approach to restore tracheal clearance. Tracheal resection and reconstruction should be considered only in selected cases when the histopathological examination provides evidence of malignancy or the radiological imaging shows tumour extension through the tracheal wall and the endoscopic treatment fails.