The risk of developing a venous thrombotic event is 4 times greater among cancer patients than the general population.1 In fact, around 20% of deep venous thrombosis and pulmonary embolisms are a result of an active cancer (i.e., cancer diagnosed in the previous year or in active treatment).2 Venous thromboembolism (VTE) is the second cause of death among cancer patients.3 Moreover, cancer patients receiving anticoagulants due to VTE have a higher risk of recurrence and bleeding than anticoagulated patients without cancer.
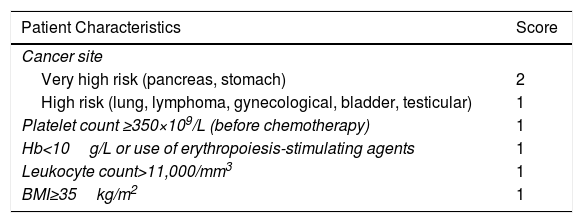
Pharmacological thromboprophylaxis is recommended in cancer patients who must be hospitalized due a medical condition, unless contraindicated. Similarly, patients with active cancer who are scheduled to undergo major surgery should receive pharmacological thromboprophylaxis. However, the evidence is much less consistent in cancer outpatients who are receiving chemotherapy. Scientific societies recommend the use of well-validated risk models, such as the Khorana model (Table 1) to identify subgroups of patients with a high risk of thrombotic events.4 Thromboprophylaxis with low molecular weight heparin (LMWH) should only be considered in patients with a score of ≥3 on the Khorana model or advanced pancreatic cancer, and patients with myeloma receiving thalidomide or lenalidomide may receive aspirin or LMWH.5
Khorana Risk Model.
| Patient Characteristics | Score |
|---|---|
| Cancer site | |
| Very high risk (pancreas, stomach) | 2 |
| High risk (lung, lymphoma, gynecological, bladder, testicular) | 1 |
| Platelet count ≥350×109/L (before chemotherapy) | 1 |
| Hb<10g/L or use of erythropoiesis-stimulating agents | 1 |
| Leukocyte count>11,000/mm3 | 1 |
| BMI≥35kg/m2 | 1 |
Hb: hemoglobin; BMI: body mass index.
Score: 0 points, low risk; 1–2 points, intermediate risk; ≥3 points, high risk.
Source: Khorana et al.4
In patients with VTE and cancer, LMWH during the first 3–6 months is associated with a significantly lower risk of recurrent thrombosis than warfarin.6 It is still not completely clear whether patients should receive therapeutic doses of LMWH throughout their treatment, so we recommend using the LMWH regimen that has been tested in clinical trials for each product (i.e., full doses of enoxaparin and tinzaparin, and a 75% dose reduction for dalteparin after the first month). After this 3–6 month period of anticoagulation, the decision to continue anticoagulants depends on a number of factors, such as tumor activity, indication for anticancer treatment, patient's tolerance of anticoagulation, patient preferences, and cost and availability of treatment. No clinical trials have been published on the efficacy and safety of LMWH in cancer patients with VTE beyond the first 6 months of treatment. Chai-Adisaksopha et al. used data from the RIETE registry and propensity score matching to compare the efficacy and safety of vitamin K antagonists with LMWH in cancer patients with VTE after the first 6 months of treatment.7 Patients receiving LMWH had a similar rate of recurrent deep venous thrombosis (relative risk [RR] 1.41; 95% confidence interval [CI] 0.68–2.93), recurrent pulmonary thromboembolism (RR 0.73; 95% CI 0.34–1.58), major bleeding (RR 1.15; 95% CI 0.55–2.40), and non-major bleeding (RR 0.96; 95% CI 0.51–1.79) compared with those who received vitamin K antagonists, and a higher mortality rate (RR 1.58; 95% CI 1.13–2.20).
Given the lack of consistent data to support their efficacy and safety in cancer patients, direct-acting anticoagulants (apixaban, dabigatran, edoxaban, and rivaroxaban) are not indicated in the treatment of VTE in these patients. However, data from the Hokusai VTE Cancer clinical trial8 have recently been published, comparing edoxaban with dalteparin for up to 12 months in 1050 cancer patients with VTE. The primary efficacy event (a composite of recurrent thrombosis and major bleeding) occurred in 67 patients (12.8%) who received edoxaban and in 71 patients (13.5%) who received dalteparin (hazard ratio for edoxaban of 0.97; 95% CI 0.70–1.36; P=.0056 for non-inferiority). Caravaggio (NCT03045406) is an open-label randomized clinical trial comparing apixaban vs dalteparin in the first 6 months of treatment of symptomatic or incidental VTE in cancer patients over the age of 18 years. The Select-D study (ISRCTN86712308) is an open-label randomized clinical trial which compares dalteparin vs rivaroxaban in patients with VTE and cancer. Moreover, patients with residual deep venous thrombosis in the sixth month of treatment will be randomized to rivaroxaban or placebo for an additional 6 months. CANVAS (NCT02744092) is an open-label randomized clinical trial that will compare the efficacy and safety of 6 months’ treatment with direct-acting oral anticoagulants vs warfarin in cancer patients with confirmed VTE.
Between 8% and 12% of patients with VTE (presumably idiopathic) are diagnosed with occult cancer in the early follow-up period. In view of the results of several studies that have evaluated the usefulness of exhaustive cancer screening in this group of patients,9 the International Society of Thrombosis and Hemostasis recommends limited screening, including clinical history, physical examination, basic clinical laboratory tests (complete blood count, coagulation, liver function tests), and chest X-ray.10 Recently, a risk prediction score has been developed for occult cancer in patients with VTE. This scale comprises the following variables: male (1 point), >70 years (2 points), chronic lung disease (1 point), anemia (2 points), platelets ≥350×109/L (1 point), previous surgery (minus 2 points), VTE (minus 1 point).11 In an external, retrospective validation of this scale, occult cancer was identified in 13.8% of high-risk patients (i.e., score≥3) compared to 3.6% of low-risk patients.
In conclusion, the treatment of VTE associated with malignant disease is a challenge in daily clinical practice. Well-designed studies are needed to identify patients receiving chemotherapy in an outpatient setting in whom pharmacological thromboprophylaxis has an acceptable risk-benefit balance. In addition, ongoing clinical trials are needed to establish the role of direct-acting anticoagulants in the initial and long-term treatment of VTE associated with cancer.
Conflict of InterestsDJ is a member of the Data and Safety Monitoring Board of the Caravaggio clinical trial.
Please cite this article as: Barrios D, Jara-Palomares L, Jiménez D. Enfermedad tromboembólica venosa y cáncer: un reto para los clínicos. Arch Bronconeumol. 2018;54:359–360.