Occasionally, some neoplasia are associated with a hypercoagulable state (HCS) that increases the likelihood of thrombi formation (Trousseau sign) in the venous territory1; arterial involvement is uncommon.
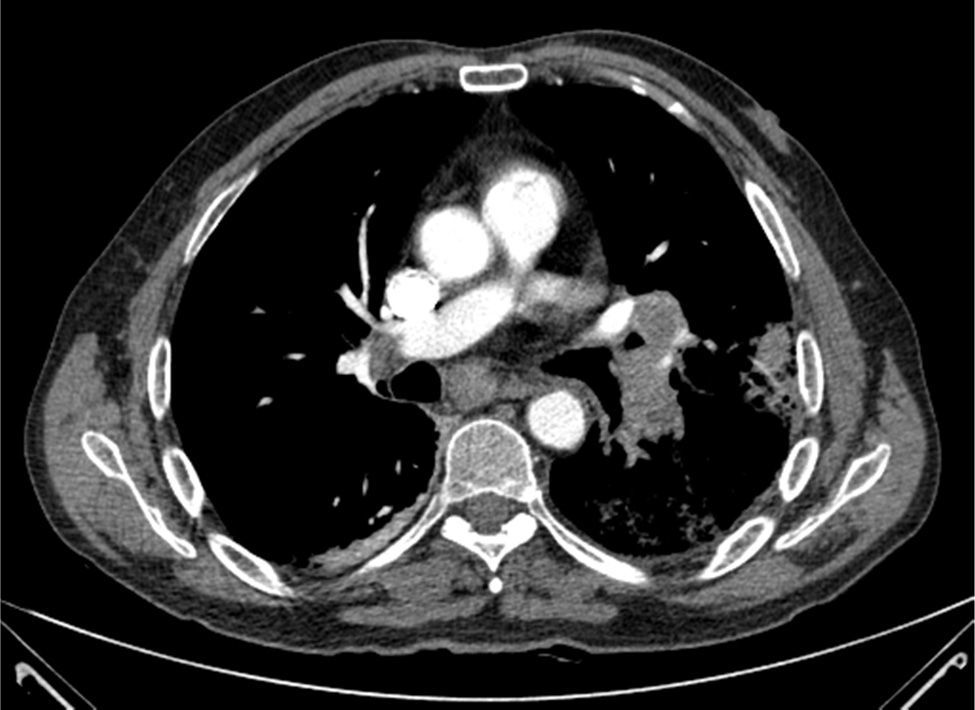
We present the case of a 58-year-old man who was seen in the emergency department of our hospital for symptoms of pleuritic pain in the right hemithorax, low-grade fever and hemoptoic expectoration. He was diagnosed with a pulmonary embolism (PE) in the right basal pyramid and a left parahilar mass infiltrating the left main pulmonary artery and tracheal carina; he also had bilateral mediastinal lymphadenopathies (Fig. 1).
Bronchoscopy revealed an infiltrated carina, from which an underlying lesion protruded; a biopsy was taken, which was positive for lung adenocarcinoma.
We requested Doppler ultrasound of the lower limbs, which confirmed deep vein thrombosis (DVT) in the right deep femoral/popliteal territory.
Forty-eight hours after admission to Respiratory Medicine, in spite of anticoagulant doses of low molecular weight heparin (LMWH), the patient experienced an episode of intense pain, with coldness and loss of pulse in the right foot. He was assessed by the Vascular Surgery department and diagnosed with acute arterial ischemia (AAI). An emergency thrombectomy was performed (histopathology of the thrombus was negative for malignancy), and sodium heparin infusion was started. The episode recurred at 5 and 14 days after admission. Repeat thrombectomy was performed after the second episode, but given the subsequent functional state of the right lower limb (RLL), pain that could not be controlled with opiate infusion, and in view of possible complications due to the start of chemotherapy (CT) treatment, we decided to amputate the RLL.
The patient subsequently began chemotherapy, and has had no further episodes of arterial ischemia to date.
The association between AAI and neoplasia is not as well defined as in the case of those of venous origin. Some neoplasia, particularly those that originate in the pancreas, lung and gastrointestinal tract, produce an HCS or cause a deficiency of some coagulant substances (proteins C and S, anti-thrombin III).2 In this patient, we found an HCS of malignancy with both venous (PE/DVT) and arterial (AAI right foot) manifestations. This HCS is usually resistant to LMWH treatment,3 and can be worsened by previous atherosclerosis and CT treatment.4
The primary treatment indication is surgery (thrombectomy), followed by anticoagulation with heparin, but these are generally ineffective in a high percentage of patients. Conservative treatment has a poor prognosis, and a significant number of patients require amputation, with survival rates of 50% at 3 months and 17% at 1 year after the first event. In a study by Rigdon,5 all patients eventually required amputation, despite surgical and anticoagulation treatment.
In conclusion, HCSs of malignancy are uncommon, especially vascular manifestations, but in these cases it is important to rule out the existence of an occult neoplasm as part of the diagnostic algorithm.
Please cite this article as: Segrelles Calvo G, García Pérez S, Cabrera I. Manifestaciones vasculares del adenocarcinoma pulmonar: a propósito de un caso. Arch Bronconeumol. 2015;51:201–202.