Patients with chronic obstructive pulmonary disease (COPD) perform limited physical activity. Surprisingly, there is a lack of research in COPD about the validity of physical activity questionnaires. Our aim was to validate the Yale Physical Activity Survey in COPD patients in order to quantify and classify their levels of physical activity.
Methods172 COPD patients from 8 university hospitals in Spain wore an accelerometer (SenseWear® Pro2 Armband) for 8 days and answered the questionnaire 15 days later. Statistical analyses used to compare both tools measures included: (i) Spearman's correlation coefficient, (ii) intraclass correlation coefficient (ICC) and Bland–Altman plots, (iii) distribution of accelerometer measurements according to tertiles of the questionnaire, and (iv) receiver operating characteristic (ROC) curves to detect sedentary patients.
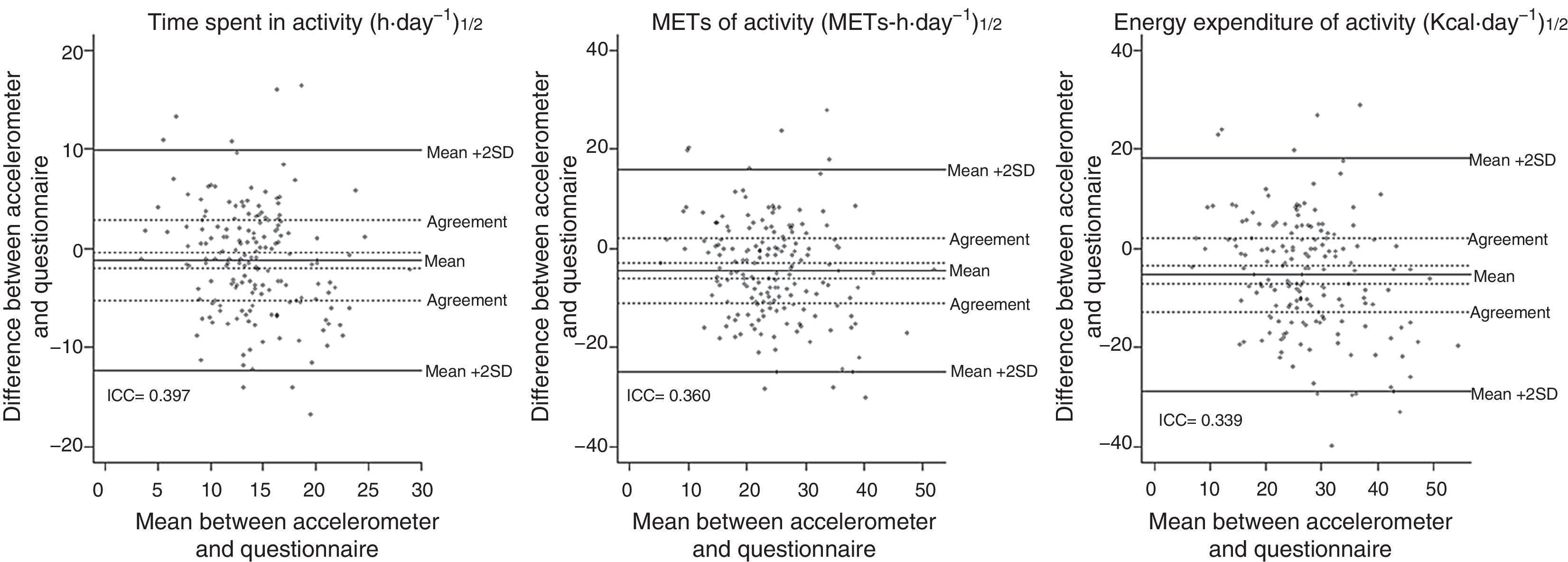
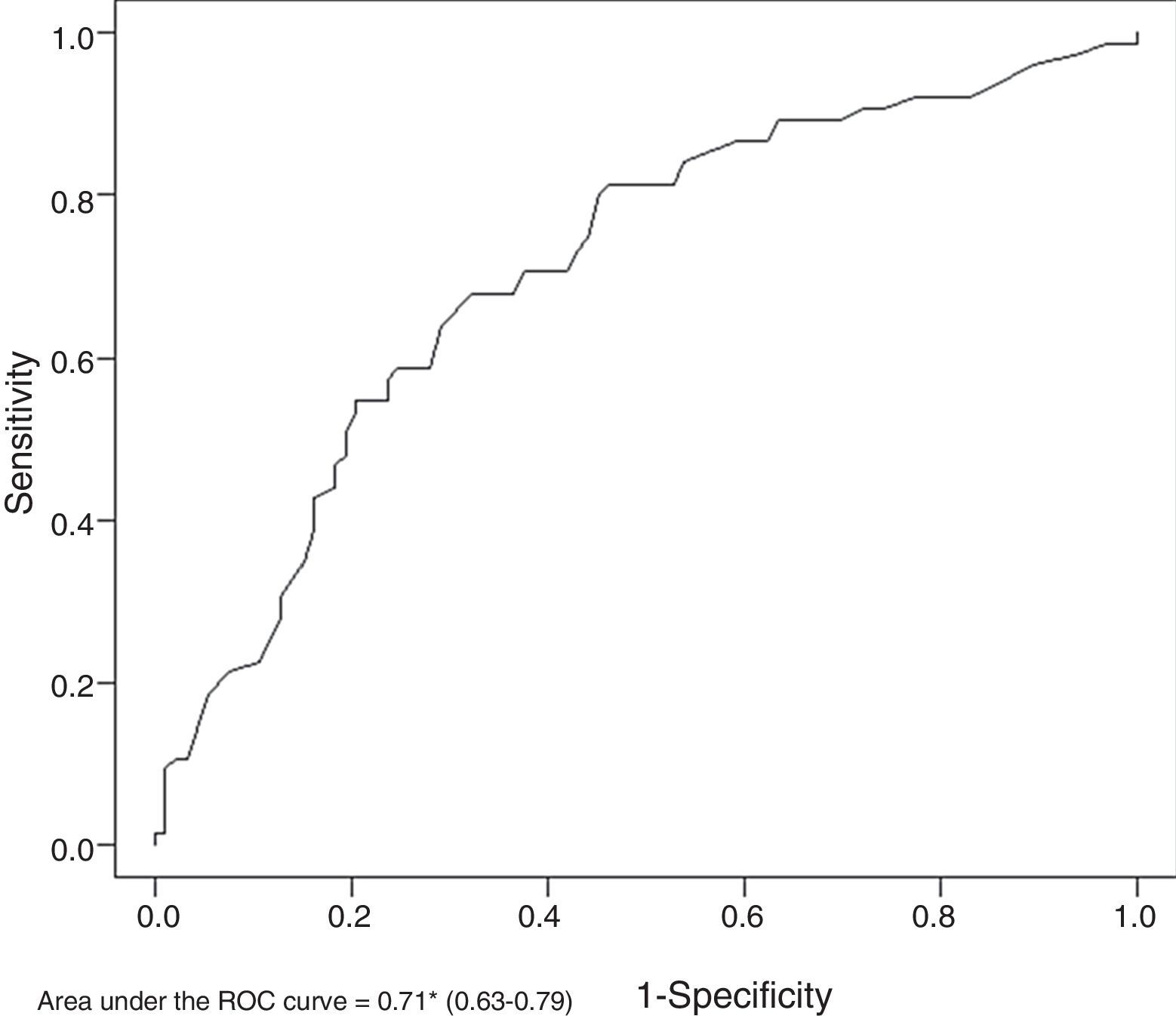
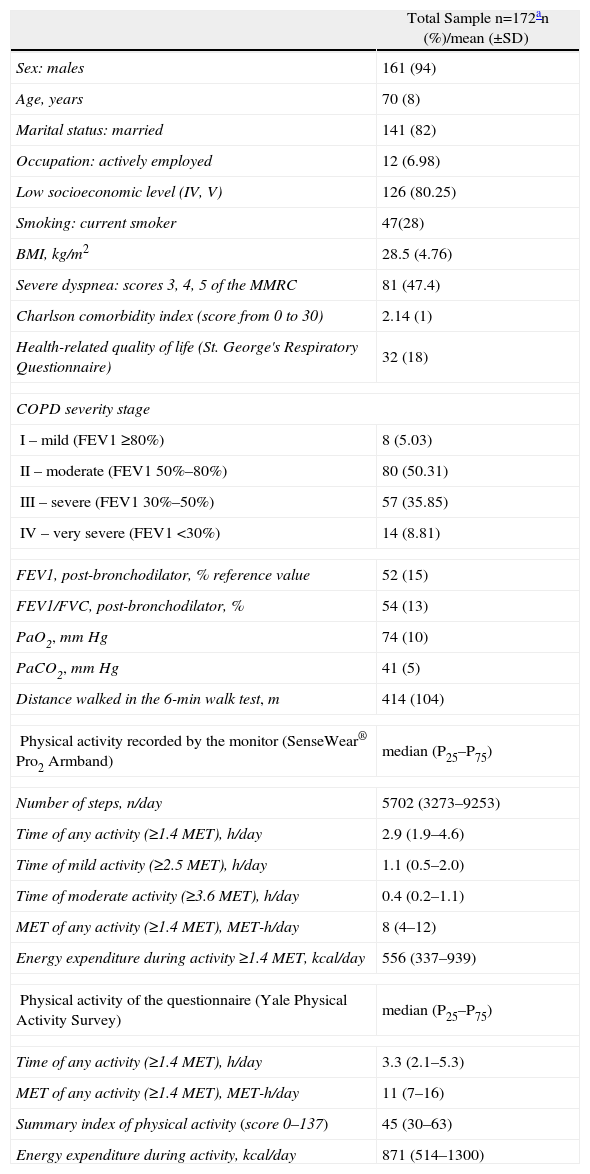
Results94% of participants were men, 28% were active smokers and 7% were currently working. Mean (standard deviation) age was 70 (8) years, mean post-bronchodilator FEV1 was 52 (15)% predicted, and median (p25–p75) steps taken was 5702 (3273–9253) steps per day−1. Spearman correlations were low to moderate (from 0.29 to 0.52, all P<.001). ICCs showed weak agreement (from 0.34 to 0.40, all P<.001). A wide variability in agreement was observed in the Bland–Altman plots. Significant differences in accelerometer measurements were found according to questionnaire tertiles (all P<.001). The area under the ROC for identifying sedentarism was 0.71 (95% CI: 0.63–0.79).
ConclusionsThe Yale Physical Activity Survey may be a valid tool to classify, but not to quantify, physical activity performed by COPD patients. The summary index of this questionnaire, based on seven short questions, shows the best validity properties. This suggests that it should be considered as a screening tool to identify patients at risk for sedentarism.
Los pacientes con enfermedad pulmonar obstructiva crónica (EPOC) se caracterizan por una actividad física limitada. Sorprendentemente, apenas se dispone de investigación sobre los cuestionarios para medir la actividad física en la EPOC. El objetivo del presente estudio fue validar el cuestionario Yale Physical Activity Survey en pacientes con EPOC.
MétodosUn total de 172 pacientes de 8 hospitales universitarios españoles usaron un acelerómetro (SenseWear® PrO2 Armband) durante 8 días y contestaron el cuestionario. Los análisis estadísticos de comparación de ambos instrumentos incluyeron: a) correlación de Spearman; b) coeficiente de correlación intraclase (CCI) y gráficos de Bland–Altman; c) distribución de las medidas del acelerómetro según los terciles del cuestionario, y d) la curva receiver operating characteristic (ROC) para detectar a los pacientes sedentarios.
ResultadosEl 94% de los participantes eran hombres, el 28% eran fumadores y el 7% eran trabajadores activos; la edad media (±DE) fue de 70 (8) años, el volumen espiratorio medio en el primer segundo (VEMS) posbroncodilatador fue de 52 (15) como porcentaje del valor de referencia, y la mediana (p25–p75) de pasos fue de 5.702 (3.273–9.253) pasos/día. Las correlaciones de Spearman fueron débiles o moderadas (desde 0,29 hasta 0,52, todas las p<0,001). Los CCI mostraron concordancias débiles (desde 0,34 hasta 0,40, todas las p<0,001). Los gráficos de Bland–Altman mostraron una gran variabilidad en la concordancia. Se encontraron diferencias significativas en las medidas del acelerómetro según los terciles del cuestionario (todas las p<0,001). El área bajo la curva ROC para identificar el sedentarismo fue de 0,71 (intervalo de confianza del 95%: 0,63–0,79).
ConclusiónEl cuestionario Yale Physical Activity Survey es una herramienta válida para clasificar la actividad física que realizan los pacientes con EPOC, pero no para cuantificarla. El índice resumen del cuestionario, originado de tan solo 7 preguntas, muestra los mejores resultados de validez, sugiriendo que debería considerarse un instrumento de cribado para identificar a los pacientes que corren riesgo de sedentarismo.
Frequent physical activity has been related with a reduction in risk for hospitalization and mortality in patients with chronic obstructive pulmonary disease (COPD).1–3 Consequently, there is a growing interest in measuring physical activity in these patients in order to study its determinants and effects as well as its clinical evaluation. There are several tools used to measure physical activity, and research on their ease of use, validity and reliability for monitoring physical activity in patients with COPD has grown exponentially. Similarly, the use of these monitors in clinical research of physical activity and COPD has increased,4 despite some disagreements about their interpretation.5 Nevertheless, there is a lack of research in COPD about the ease of use, validity or reliability of questionnaires,4 which are widely used instruments for measuring physical activity in other fields of research. Physical activity questionnaires have identified the health benefits of physical activity in numerous diseases and chronic processes. The questionnaires have a generalized applicability, are low-cost, easy to use and are the method of choice for measuring physical activity in large-scale epidemiological studies.6–8 The specific sociodemographic characteristics of COPD patients (seniors, retirees) and their functional limitations impede the use of any questionnaire that has not been previously validated in this population. We selected the Yale Physical Activity Survey (YPAS)9 because it is one of the most detailed, available for senior subjects and whose validity, reliability and sensitivity to change have been previously published.9–11 The YPAS reflects the volume, frequency and intensity of physical activity, expressed as metabolic equivalents of task (MET), meaning MET-h/week, which are able to estimate the effects of physical activity as a continuous parameter even in the lowest levels of activity (predictable in COPD).8
The objective of the present study is to validate the YPAS in COPD patients in order to quantify the levels of physical activity and classify the patients according to these levels using a physical activity monitor (accelerometer) as a reference.
MethodsStudy TypeA concurrent validity study.
ParticipantsThis study is part of the study entitled “Phenotypic Characterization and Evolution of Chronic Obstructive Pulmonary Disease (PAC-COPD)”.12,13 Briefly, the individuals were recruited during their first hospitalization due to COPD exacerbation and the diagnosis of COPD (post-bronchodilator forced expiratory volume in one second [FEV1] – forced vital capacity [FVC] ratio [FEV1/FVC]<0.70)14 was confirmed under stable clinical conditions at least 3 months after hospitalization. After 18 months, the patients were invited to participate in a validation protocol of physical activity in patients who continued to survive and were candidates (n=257) after a pilot test in a reduced sample of patients not included in the PAC-COPD.15 Among these, 75 patients (29%) did not participate (8 belonged to a hospital that did not participate in the study on physical activity, one patient could not use the monitor as he was missing his right arm, 58 refused to use the accelerometer and 8 did not answer the questionnaire). The comparison of the characteristics between participants and non-participants demonstrated that there was a greater proportion of retired individuals among the participants (93% vs 84%, P=.019) than among the non-participants. There were no differences in other variables for sociodemographics, dyspnea, quality of life, comorbidities, smoking, lung function, nutritional state or capacity for exercise. Lastly, out of the 182 patients who completed the validation study, 10 were excluded because they used the accelerometer less than the minimum previously defined time, which left a total of 172 patients for the analysis. The study was approved by the research committees of all the participating hospitals and informed consent was given by all the individuals. More details about the selection process have been previously described.16
Determination Tools and VariablesThe study was carried out under conditions of clinical stability and at least 3 months after the last COPD exacerbation. The data from the monitor were obtained before the survey was completed and, consequently, following the general recommendations that, when administering a sequence of measurements, the first should be the least sensitive to the objectives of the study, expectations of the researcher or knowledge about the following measurement.17 The questionnaire was administered 2 weeks later since the questions referred to the 4 weeks prior and included the period of the accelerometer.
Physical activity was determined with the SenseWear® Pro2 Armband monitor (SWA; Body Media, Pittsburgh, PA), which has shown to be a valid parameter for physical activity in COPD patients.18 The patients used the monitor for 8 consecutive days and the minimum use time was previously defined as at least 3 days registering more than 70% of the daytime hours (from 8a.m. to 10p.m.).19 The first and last days were not used for the analysis because they were not representative of usual physical activity.19 The congruency of the monitor data was tested using the intraclass correlation coefficient (ICC) of the steps taken per day among all the possible 3-day combinations (ICC=0.95, 95% CI: 0.93–0.96). Accelerometers measure the magnitude of the changes in acceleration of the center of the body mass during movement. The monitor used in this present study is biaxial, registering the movement on the axes X and Y. The armband system was placed on the right arm and it registered the movements of the upper and lower thirds of the subjects’ bodies, proving a minute-by-minute report of the two movement axes, thermal flow, galvanic response of the skin, skin temperature and environmental temperature near the body. For each patient, the data obtained included the number of steps taken per day as well as time (h/day), intensity (MET-h/day), and energy output (cal/day), physical activity of any, light or moderate intensity (defined as activities ≥1.4, ≥2.5 and ≥3.6MET, respectively). As an indicator of sedentarism, a cut-point was defined as <30min/day of moderate activity, as recommended by the American College of Sports and Medicine.20
Two weeks after the accelerometer register, two experienced interviewers administered the validated Spanish version10 of the Yale survey.9 This questionnaire compiles information (frequency, intensity and duration) for an extensive list of activities performed in the last 4 weeks (therefore it includes the period in which the accelerometer was used). Since some of the patients were actively working, we slightly modified the original questionnaire, adding a question about the physical activity done at work, as has been previously published.21 The final version of the questionnaire is available on our website (http://www.creal.cat). From the list of activities of the questionnaire, we obtained two summarizing parameters: time per day (in h) and daily intensity (MET-h) of the physical activity ≥1.4MET. The YPAS also includes 7 questions that combine the frequency and intensity of the activities in general, which provides an index that summarizes the activity with a score that varies between 0 and 137.9 In addition, we calculated the energy expenditure of the physical activity, multiplying the MET of each individual by body weight, following the formula 1MET=1kcal/h/kg.22
We obtained other pertinent variables, including sociodemographic factors, the Charlson comorbidity index, the St. George's Respiratory questionnaire in order to evaluate health-related quality of life, dyspnea, lung function (FEV1, FVC, FEV1/FVC and partial arterial oxygen and carbon dioxide pressures [PaO2, PaCO2]), nutritional state (body mass index), and 6-min walk test. The details about these procedures have been previously published.13,16
Statistical AnalysisIt was estimated that at least 107 individuals were necessary in order to identify correlations ≥0.3, accepting an alpha risk of 0.05 and a beta risk of 0.2 in a two-tailed test (bilateral) and anticipating a drop-out rate of 20%.
The characteristics of the individuals are presented as number (percentage) for the categorical variables, means (±standard deviation [SD]) for the continuous variables with normal distribution, or medians (P25–P75) for continuous variables with abnormal distribution.
The validation of the questionnaires was done with different strategies. First of all, in order to evaluate the linear relationship between the continuous variables of the questionnaire, the accelerometer and the distance walked in 6min, a Spearman's correlation was used. In accordance with the previous data of the physical activity questionnaires, the expected correlations ranged between 0.35 and 0.45.9,10,23
Secondly, the agreement between the questionnaire and the monitor for time, intensity (MET) and energy expenditure during activity ≥1.4MET was examined by means of the intraclass correlation coefficient (ICC) and Bland–Altman plots. For this effect, all the variables were transformed in order to approach normal distribution using the squared root. We used an ICC with random effect for a factor, which can be conceived as the ratio of the intra-individual variance over the total variance.24 The Bland–Altman plots show for each variable the difference between the accelerometer and the questionnaire compared with the mean value of both instruments. The limits of agreement between the accelerometer and the questionnaire were, by default, the mean difference ±2 SD. However, depending on the previous estimations of the intra-individual biological and analytical variation of the daily energy expenditure,24,25 we defined a priori a stricter limit of agreement, established at ±30% of the mean estimation of the accelerometer.
Thirdly, the distribution of the accelerometer parameters in accordance with the tertiles of the questionnaire parameters was evaluated using the Kruskal–Wallis test. Lastly, we tested the capability of the questionnaire for detecting sedentary individuals using the morphologic study of the receiver operating characteristic (ROC) curve.
In addition, we tested which are the possible determinants of the differences between the quantitative parameters of the questionnaire and the monitor, using a linear regression adjusted for the quantity of physical activity, as defined by the accelerometer. We constructed a stratified analysis of the validation analyses (correlations, Bland–Altman plots, ICC and ROC curves) according to the determinants identified in the previous linear regression models. As an analysis of sensitivity, we repeated all the analyses: (a) using only the individuals up until the 95th percentile in the questionnaire or accelerometer; and (b) with exclusion of the individuals with acute health problems during the administration of the questionnaire and/or the accelerometer (n=4). The analyses were done using the R 2.6.2 program (2008 The R Foundation for Statistical Computing).
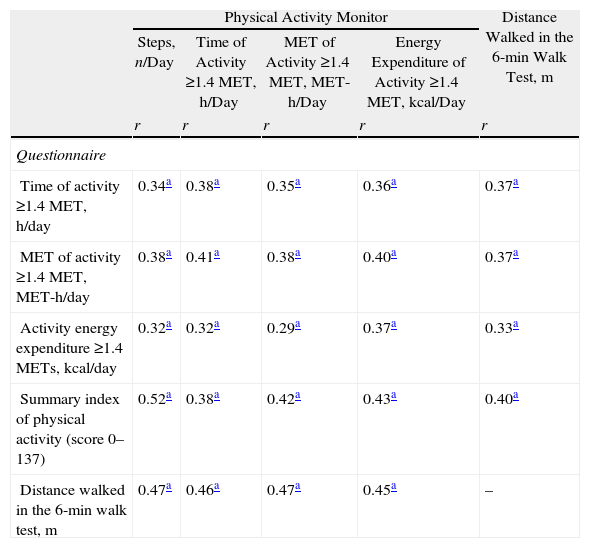
ResultsTable 1 demonstrates the characteristics of the sample. The patients used the accelerometer a mean of 6 days and registered a mean of 95% of the daytime hours (13.5h out of a maximum of 14h). A total of 79 (48%) patients did a minimum of 30min of at least moderate physical activity (56%, 45%, 49%, and 40%, in mild, moderate, severe and very severe COPD, respectively). All the physical activity parameters of the questionnaire positively correlated with the parameters of the accelerometer, with Spearman's coefficients that varied from 0.29 to 0.52 (all P<.001; Table 2).
Sociodemographic, Clinical and Physical Activity Data for 172 Patients With Chronic Obstructive Pulmonary Disease (COPD).
| Total Sample n=172an (%)/mean (±SD) | |
| Sex: males | 161 (94) |
| Age, years | 70 (8) |
| Marital status: married | 141 (82) |
| Occupation: actively employed | 12 (6.98) |
| Low socioeconomic level (IV, V) | 126 (80.25) |
| Smoking: current smoker | 47(28) |
| BMI, kg/m2 | 28.5 (4.76) |
| Severe dyspnea: scores 3, 4, 5 of the MMRC | 81 (47.4) |
| Charlson comorbidity index (score from 0 to 30) | 2.14 (1) |
| Health-related quality of life (St. George's Respiratory Questionnaire) | 32 (18) |
| COPD severity stage | |
| I – mild (FEV1 ≥80%) | 8 (5.03) |
| II – moderate (FEV1 50%–80%) | 80 (50.31) |
| III – severe (FEV1 30%–50%) | 57 (35.85) |
| IV – very severe (FEV1 <30%) | 14 (8.81) |
| FEV1, post-bronchodilator, % reference value | 52 (15) |
| FEV1/FVC, post-bronchodilator, % | 54 (13) |
| PaO2, mmHg | 74 (10) |
| PaCO2, mmHg | 41 (5) |
| Distance walked in the 6-min walk test, m | 414 (104) |
| Physical activity recorded by the monitor (SenseWear® Pro2 Armband) | median (P25–P75) |
| Number of steps, n/day | 5702 (3273–9253) |
| Time of any activity (≥1.4MET), h/day | 2.9 (1.9–4.6) |
| Time of mild activity (≥2.5MET), h/day | 1.1 (0.5–2.0) |
| Time of moderate activity (≥3.6MET), h/day | 0.4 (0.2–1.1) |
| MET of any activity (≥1.4MET), MET-h/day | 8 (4–12) |
| Energy expenditure during activity ≥1.4MET, kcal/day | 556 (337–939) |
| Physical activity of the questionnaire (Yale Physical Activity Survey) | median (P25–P75) |
| Time of any activity (≥1.4MET), h/day | 3.3 (2.1–5.3) |
| MET of any activity (≥1.4MET), MET-h/day | 11 (7–16) |
| Summary index of physical activity (score 0–137) | 45 (30–63) |
| Energy expenditure during activity, kcal/day | 871 (514–1300) |
MMRC: modified Medical Research Council dyspnea scale; BMI: body mass index.
Correlation Between the Physical Activity Parameters of the Monitor and the Questionnaire and the Distances Walked in the 6-min Walk Test in 172 Patients With Chronic Obstructive Pulmonary Disease (COPD).
| Physical Activity Monitor | Distance Walked in the 6-min Walk Test, m | ||||
| Steps, n/Day | Time of Activity ≥1.4MET, h/Day | MET of Activity ≥1.4MET, MET-h/Day | Energy Expenditure of Activity ≥1.4MET, kcal/Day | ||
| r | r | r | r | r | |
| Questionnaire | |||||
| Time of activity ≥1.4MET, h/day | 0.34a | 0.38a | 0.35a | 0.36a | 0.37a |
| MET of activity ≥1.4MET, MET-h/day | 0.38a | 0.41a | 0.38a | 0.40a | 0.37a |
| Activity energy expenditure ≥1.4METs, kcal/day | 0.32a | 0.32a | 0.29a | 0.37a | 0.33a |
| Summary index of physical activity (score 0–137) | 0.52a | 0.38a | 0.42a | 0.43a | 0.40a |
| Distance walked in the 6-min walk test, m | 0.47a | 0.46a | 0.47a | 0.45a | – |
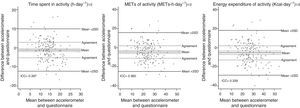
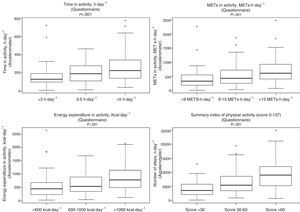
The intraclass correlation coefficients for the time spent performing activity, intensity (MET) and energy expenditure were 0.397, 0.360 and 0.339, respectively, showing that less than half of the variance of the concordance was attributable to the variability of the individuals. The corresponding Bland–Altman plots showed that the mean values were significantly different between the questionnaire and the accelerometer (Fig. 1). There was a wide variability in the agreement; in 45%, 56%, and 57% of the cases it was higher than the previously defined limit for agreement for the time spent in each activity, the intensity and the energy expenditure, respectively.
Intraclass correlation coefficients (ICC) and Bland–Altman plots of the physical activity parameters of the monitor and the survey in 172 patients with chronic obstructive pulmonary disease (COPD) (the ICC is a proper statistic for evaluating the degree of agreement between measurements of the same construct, and can be conceived as the ratio of the intra-individual variance over total variance).
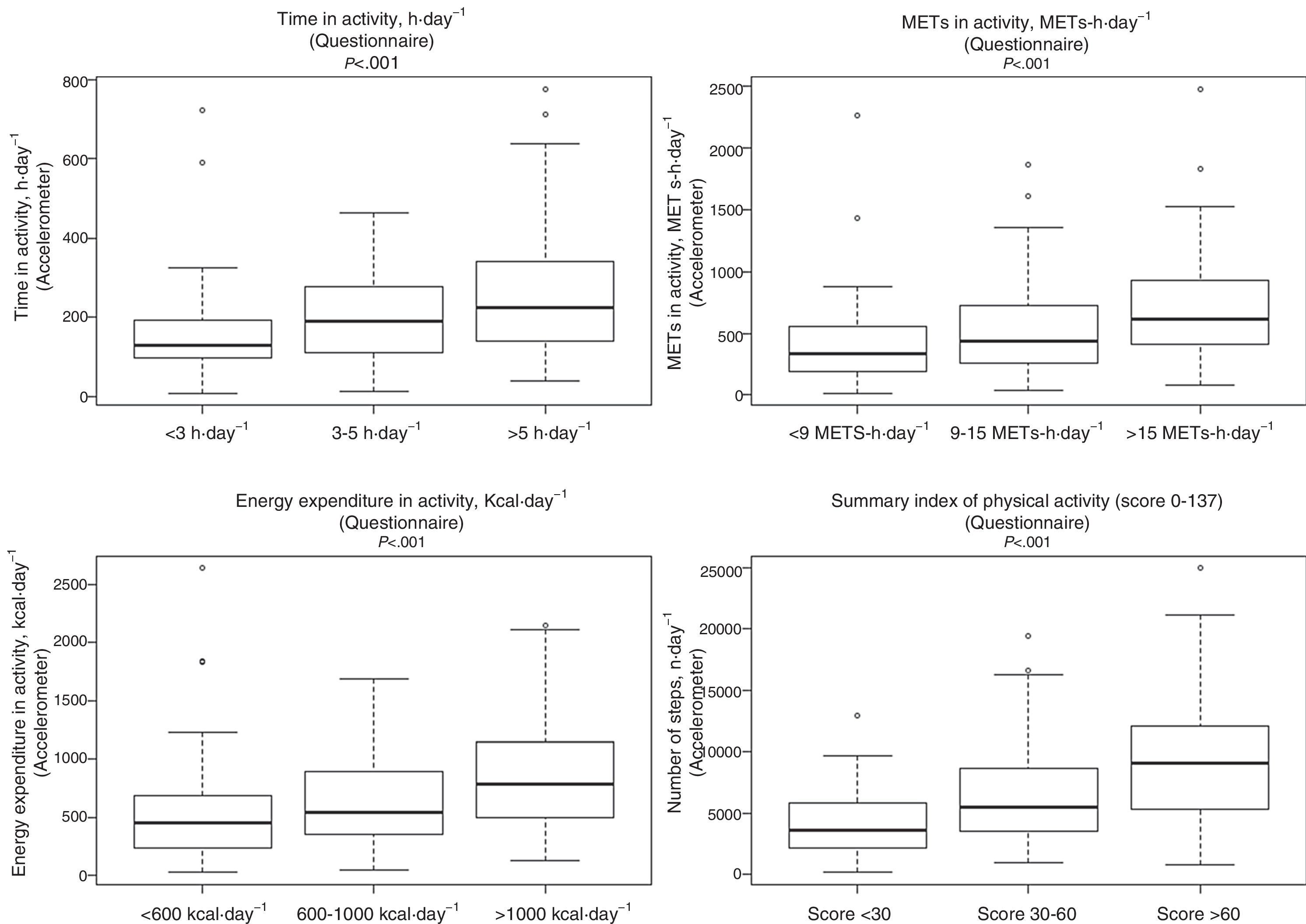
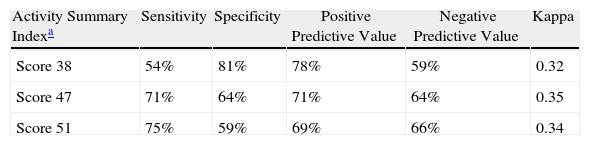
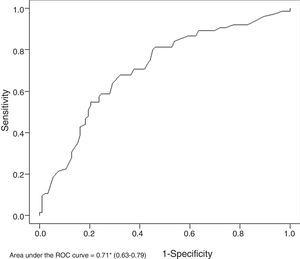
The mean values of the physical activity variables recorded by the monitor increased in accordance with the tertiles of the corresponding parameters in the questionnaire (all the P<0.001) (Fig. 2). Fig. 3 shows that the area under the ROC curve between the summary of the activity according to the questionnaire and sedentarism was 0.71 (95% CI: 0.63–0.79). Table 3 shows three different cut-points with high sensitivity and specificity for identifying the sedentary individuals based on the questionnaire.
Receiver operating characteristic (ROC) curve of the summary index of activity, determined from the questionnaire, compared with sedentarism, defined as <30min/day of moderate physical activity based on the monitor, in 172 patients with chronic obstructive pulmonary disease (COPD). An area under the curve of 0.71 means that, if two individuals are selected randomly (one above and another under the cut-points of the questionnaire), 71% of the time they will be correctly classified as sedentary/non-sedentary, in accordance with the monitor.
Performance of the Physical Activity Summary Index of the YPAS in Order to Identify the Sedentary Individuals (Defined as <30min/Day of Moderate Physical Activity) in 172 Patients With Chronic Obstructive Pulmonary Disease (COPD).
| Activity Summary Indexa | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | Kappa |
| Score 38 | 54% | 81% | 78% | 59% | 0.32 |
| Score 47 | 71% | 64% | 71% | 64% | 0.35 |
| Score 51 | 75% | 59% | 69% | 66% | 0.34 |
In theory, the summary index varies from 0 to 137, and in the sample of the present study, from 4 to 88. The analysis of the ROC curve identifies three cut-points with different sensitivities and specificities for detecting sedentary individuals based on the questionnaire. For instance, using a score of 38 as the cut-point (which means, defining as sedentary those patients with a score ≤38 in the questionnaire), 54% of the actual sedentary individuals (based on the monitor) would be identified as sedentary, 81% of the actual non-sedentary subjects (based on the monitor) would be identified as non-sedentary, and the proportion of sedentary/non-sedentary subjects correctly identified by the questionnaire would be, respectively, 78% and 59%.
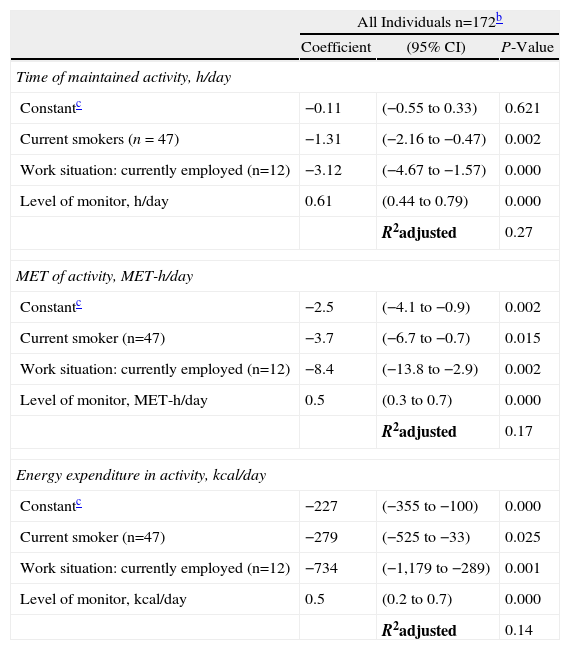
Table 4 shows that: (a) being a current smoker and being actively employed led to higher values in the questionnaire than in the accelerometer; and (b) growing levels of activity as defined by the accelerometer were related with a decrease in the differences between instruments. There was no statistically significant interaction or modification of the effect between being a smoker and active worker. Other potential determinants showed no association in the bivariate or multivariate models.
Mutually Adjusted Determinantsa of the Differences Between the Physical Activity Parameters of the Monitor and the Questionnaire (Multivariate Linear Regression) in 172 Patients With Chronic Obstructive Pulmonary Disease (COPD).
| All Individuals n=172b | |||
| Coefficient | (95% CI) | P-Value | |
| Time of maintained activity, h/day | |||
| Constantc | −0.11 | (−0.55 to 0.33) | 0.621 |
| Current smokers (n=47) | −1.31 | (−2.16 to −0.47) | 0.002 |
| Work situation: currently employed (n=12) | −3.12 | (−4.67 to −1.57) | 0.000 |
| Level of monitor, h/day | 0.61 | (0.44 to 0.79) | 0.000 |
| R2adjusted | 0.27 | ||
| MET of activity, MET-h/day | |||
| Constantc | −2.5 | (−4.1 to −0.9) | 0.002 |
| Current smoker (n=47) | −3.7 | (−6.7 to −0.7) | 0.015 |
| Work situation: currently employed (n=12) | −8.4 | (−13.8 to −2.9) | 0.002 |
| Level of monitor, MET-h/day | 0.5 | (0.3 to 0.7) | 0.000 |
| R2adjusted | 0.17 | ||
| Energy expenditure in activity, kcal/day | |||
| Constantc | −227 | (−355 to −100) | 0.000 |
| Current smoker (n=47) | −279 | (−525 to −33) | 0.025 |
| Work situation: currently employed (n=12) | −734 | (−1,179 to −289) | 0.001 |
| Level of monitor, kcal/day | 0.5 | (0.2 to 0.7) | 0.000 |
| R2adjusted | 0.14 | ||
The stratified validation analyses showed very similar results for the ex-smokers and/or retired individuals, while in current smokers (n=47 [28%]) and/or in those actively employed (n=12 [7%]) we observed lower correlations and a poorer classification of the physical activity parameters. The sensitivity analysis, detailed in Section “Methods”, showed very similar levels for all the analyses (data not shown).
DiscussionThe present study evaluated the validity of a self-administered physical activity questionnaire in a COPD population by means of the comparison of the YPAS questionnaire with the SenseWear® Pro2 Armband accelerometer. In order to evaluate the valid properties of the survey, several strategies were used that demonstrated the following: (a) positive correlations that were statistically significant between both tools; (b) a reduced agreement between instruments and a substantial overestimation of physical activity by the questionnaire; (c) statistically significant differences in the parameters of the monitor in accordance with the tertiles of the questionnaire; and (d) satisfactory performance for the identification of sedentary patients.
The correlations between the questionnaire and the monitoring system varied from low to moderate (0.30–0.48) in the sample of patients with COPD in the present study, which corresponds with the values from 0.35 to 0.45 that are predictable based on the studies published in healthy individuals of older age.9,10,23 In addition, it is much greater than the value of 0.14 observed in a small-scale study done in COPD patients which compared the units of movement of the vector of a tri-axial accelerometer and a questionnaire of the activity over the previous 4 days.26 The greatest correlation coefficient was obtained between the survey summary index and the steps taken as measured by the monitor, which are the most widely accepted parameters of each tool.4 As was expected, the 6-min walk distance (an objective parameter for exercise capacity) exhibited slightly higher correlation coefficients with the accelerometer (an objective parameter for physical activity) than with the questionnaire (a subjective parameter of physical activity). Nevertheless, it is interesting to comment that the questionnaire correlated better with the monitor than with the distance walked in 6min, which supports the opinion that physical activity is a concept different from that of capacity for exercise.27
Until now, no studies have ever examined the agreement between the quantitative parameters of the YPAS questionnaire and the parameters of the accelerometer. The data of the present study show statistically significant differences between instruments in the means of the physical activity parameters, all of which are higher in the questionnaire. The ICC estimations imply that half of the variance in the physical activity parameters can be attributed to the tool more than to the individual. In addition, the prevalence of cases that surpassed the previously defined limits of agreement (±30% of the mean estimation of the accelerometer) was around 50%. This great variability could be explained in part by the weakness of the questionnaire. The effect of social desireability28 when responding to a questionnaire (a self-administered instrument) could entail exaggerating socially accepted activities, which would lead to an overestimation of the time dedicated to the physical activity in the survey. Regardless of the cause, these data suggest that the YPAS should not be used for individual quantitative estimations of physical activity parameters.
It is worth mentioning that the analysis of the possible determinants for the differences between the accelerometer and the questionnaire only identified two variables in addition to physical activity. Being a current smoker or being actively employed increased the difference between the two instruments. One possible explanation of the first is that current smokers may over-report their physical activity due to the effect of what is socially desirable. As for the patients who were actively employed, it is possible that the questionnaire requires more direct, clear questions about the degree of physical activity done during work instead of the individual question that we added about activity at work. Lastly, it is reasonable that the levels of physical activity are also independently related with the differences between the questionnaire and the monitor, with fewer differences in the lower levels of physical activity. As a whole, and, although the variance in the differences of physical activity explained by these variables is lower than 30%, this analysis suggests that, in future research on the Yale survey in COPD patients, adjustments could be necessary for these specific populations.
The present study is the first that examines the capacity of the YPAS for discriminating physical activity among groups and for identifying sedentary individuals. As the health benefits of physical activity have been evaluated in general with physical activity in ordinal categories more than as a continuous variable,20 the results of the present study regarding the increase in mean accelerometer values in accordance with the tertiles of the questionnaire is exceedingly important. It is not known to what point the selection of cut-points (either statistically or clinically pertinent) could influence in these results. However, and given that the degrees of physical activity change through studies and questionnaires, the use of categories based on percentiles is a common practice. For the identification of sedentarism, the authors used an accepted cut-point,20 and the questionnaire seemed useful for identifying this circumstance. As long as COPD patients have a lower degree of physical activity than healthy adults of the same age29—related with their poorer state of health and poorer outcome30—the questionnaire could contribute to the early detection and treatment of sedentarism in clinical practice. From the several cut-points obtained in the analysis of the ROC curve with high sensitivity and specificity, it is proposed to use a cut-point score of 51 in the summary index of the YPAS questionnaire for the identification of sedentary patients. The reason for this choice is that the authors gave priority to the sensitivity over the specificity in the identification of sedentary individuals given the absence of harmful psychological effects associated with the diagnosis of sedentarism and the lack of adverse effects related with the recommendation of performing physical activity.
One limitation of the present study is that it does not evaluate reliability. Previous studies have demonstrated that the YPAS has an appropriate reliability in healthy individuals of older age (ICC=0.65), which could be very similar in the case of patients with COPD.10 Second, the calculation of the energy expenditure in the questionnaire could have led to an incorrect estimation of the energy expenditure in the COPD population due to the use of absolute intensities (MET values) derived from healthy individuals.22 In addition, the use of a physical activity monitor as a reference for energy expenditure could be debatable because the application of the reference algorithm of the monitor could translate into an erroneous estimation of physical activity.31 Other parameters, like the doubly labeled water method (DLW), provide more valid information about energy expenditure.7 Unfortunately, the DLW is limited to experimental studies due to its complexity, the material necessary and cost. The authors considered that the SenseWear® accelerometer is an appropriate instrument for validating the questionnaire because previous studies have demonstrated an appropriate agreement (ICC 0.54–0.73) in the physical activity parameters of its measurements and those using indirect calorimeter.32 It has been previously validated for low-intensity activities in COPD pacients,18 and it has been demonstrated that, for senior patients with low cultural levels, it is inoffensive and appropriate.15 Lastly, the sample of the present study included mostly men, which represents the actual distribution of sexes in COPD in Spain. Although it is probable that the degree of physical activity may be different in the sample of the present study than in others with a different male:female proportion, it is highly unlikely that this were to cause bias in evaluating the validity of the questionnaire.
It could be debated whether a validated questionnaire for physical activity in COPD patients is necessary or not, given the recent technological progress made in monitoring the activity of this population. Several authors coincide in affirming that the selection of the tool for measuring physical activity in COPD patients depends on the characteristics and the objectives of the research.4,5,19 Without belittling the relevance of monitoring activity, questionnaires (if these are validated and reliable) are still the most cost-efficient instruments for epidemiological research and control.33 This could also be the reason for discussion if the instruments that monitor physical activity provide data comparable to the self-evaluated experience of physical activity in COPD patients, which is unknown due to the lack of a conceptual physical activity framework in this population. One of the main advantages is the use of agreement and discrimination parameters to quantify and classify physical activity in COPD patients in addition to the generally used exclusive correlation analysis. An additional advantage comes from the use of the accelerometer for a mean of 6 days as a reference because recent studies have demonstrated systematic changes during the week19 that otherwise would have only been covered by the questionnaire. A final, novel advantage is that, in order to improve the results obtained with the questionnaire, we included patient body weight in the calculation of energy expenditure based on physical activity instead of assuming that all the subjects weighed 60kg, which is the usual strategy.9
We conclude that the Yale Physical Activity Survey is a valid tool for classifying the physical activity in patients with COPD, but not for quantifying it. Its use in large-scale epidemiological studies, including either COPD patients or patients with similar chronic processes, will provide an adequate and cost-efficient estimation of the effects of physical activity levels in these patients. Given that the summary index of the questionnaire demonstrated adequate capacity for discriminating sedentarism, the use of the series of questions that make up this index (which is a very small part of the questionnaire) should be considered a screening instrument for identifying patients who run the risk of sedentarism.
FundingThe present study was funded by the Health-Care Research Fund [FIS PI052292], the Spanish Society of Pulmonology and Thoracic Surgery [SEPAR 2004/136] and the College of Physiotherapists of Catalonia [R02/08-09]. Judith Garcia-Aymerich has a research grant from the Instituto de Salud Carlos III [CP05/00118], Ministry of Health, Spain. The PAC-COPD study is funded with grants from: the Health-Care Research Fund [FIS PI020541], Ministry of Health, Spain; the Agència d’Avaluació de Tecnologia i Recerca Mèdiques [AATRM 035/20/02], Catalonian regional government; Spanish Society of Pulmonology and Thoracic Surgery [SEPAR 2002/137]; Catalonian Pulmonology Foundation [FUCAP 2003 Beca Marià Ravà]; RESPIRA Network [RTIC C03/11]; RCESP Network[RTIC C03/09]; Health-Care Research Fund [PI052486]; Health-Care Research Fund [PI052302]; La Marató de TV3 Foundation [num. 041110]; DURSI [2005SGR00392]; Novartis Pharmaceuticals, Spain; AstraZeneca Pharmaceuticals, Spain. CIBERESP and CIBERES receive funding from the Instituto de Salud Carlos III, Ministry of Health, Spain. The sources of funding did not participate in either the study design, data collection, data analysis or interpretation, the drafting of the manuscript or the decision to present the article for publication. The researchers are independent from the funding sources.
The authors would like to express their thanks to Dr. Milo Puhan for his useful comments about the previous version of the manuscript, and to Ms. Esther Gracia for her help in processing the data from the monitors.
Center de Recerca en Epidemiologia Ambiental (CREAL), Barcelona: Josep M Antó (main researcher), Judith Garcia-Aymerich (coordinator of the project), Marta Benet, Jordi de Batlle, Ignasi Serra, David Donaire-González, Stefano Guerra; Hospital del Mar-IMIM, Barcelona: Joaquim Gea (coordinator of the center), Eva Balcells, Àngel Gayete, Mauricio Orozco-Levi, Iván Vollmer; Hospital Clínic-Institut d’Investigacions Biomèdiques August Pi i Sunyer (IDIBAPS), Barcelona: Joan Albert Barberà (coordinator of the center), Federico P. Gómez, Carles Paré, Josep Roca, Robert Rodríguez-Roisín, Àlvar Agustí, Xavier Freixa, Diego A. Rodríguez, Elena Gimeno, Karina Portillo; Hospital General Universitari Vall d’Hebron, Barcelona: Jaume Ferrer (coordinator of the center), Jordi Andreu, Esther Pallissa, Esther Rodríguez; Hospital de la Santa Creu i Sant Pau, Barcelona: Pere Casán (coordinator of the center), Rosa Güell, Ana Giménez; Hospital Universitari Germans Trias i Pujol, Badalona (Barcelona): Eduard Monsó (coordinator of the center), Alicia Marín, Josep Morera; Hospital Universitari de Bellvitge, Institut d’Investigació Biomèdica de Bellvitge (IDIBELL), l’Hospitalet de Llobregat: Eva Farrero (coordinator of the center), Joan Escarrabill; Hospital de Sabadell, Corporació Parc Taulí, Institut Universitari Parc Taulí (Universitat Autònoma de Barcelona), Sabadell: Antoni Ferrer (coordinator of the center); Hospital Universitari Son Dureta, Palma de Mallorca: Jaume Sauleda (coordinator of the center), Bernat Togores; Hospital Universitario de Cruces, UPV, Barakaldo: Juan Bautista Gáldiz (coordinator of the center), Lorena López; Instituto Nacional de Silicosis, Oviedo, Spain: José Belda.
Please cite this article as: Donaire-Gonzalez D, et al. Validación del cuestionario de actividad física de Yale en pacientes con enfermedad pulmonar obstructiva crónica. Arch Bronconeumol. 2011;47:552–60.