Traditionally cold biopsy forceps were used for endobronchial biopsy, and recently electrocautery (hot) bronchoscopy biopsy forceps are introduced. It is hypothesized that hot biopsy forceps may decrease procedure-related bleeding and also may decrease the quality of obtained samples.
Patients and methodsPatients with different indications for endobronchial biopsy during fiberoptic bronchoscopy underwent three hot and three cold biopsies with a random fashion. All biopsies were obtained with a single biopsy forceps with and without the application of an electrocoagulation current, set on soft coagulation mode (40W). A four point scale was used for the quantification of bleeding. A single pathologist blinded to the patients’ history was requested to review all samples. A three point scale was used to assess electrocoagulation damage.
ResultsA total of 240 biopsies were obtained from 40 patients. Frequency of positive concordance between the two methods was 85%. The degree of electrocoagulation damage of the samples was as follows: grade 1=52.5%, grade 2=32.5%, and grade 3=15%. The average bleeding score following hot biopsy was significantly lower compared to the cold biopsy (P=.006). The concordance between diagnostic yield of hot and cold biopsies was 85%. There was no significant difference between the diagnostic yields of two biopsy methods (P=.687).
ConclusionsHot biopsy forceps significantly decreased the procedure related bleeding. The quality of samples was not impaired significantly. Regarding low prevalence of bleeding following endobronchial biopsy, routine use of hot bronchoscopy forceps is not reasonable. However, familiarity of bronchoscopists with this method may improve bronchoscopy safety.
Tradicionalmente, para la biopsia endobronquial se utilizaban las pinzas de biopsia fría, y recientemente se ha introducido la biopsia broncoscópica con pinzas de electrocauterio (caliente). Formulamos la hipótesis de que las pinzas de biopsia caliente pueden reducir la hemorragia relacionada con el procedimiento y también disminuir la calidad de las muestras obtenidas.
Pacientes y métodosPacientes con diferentes indicaciones de biopsia endobronquial durante una fibrobroncoscopia se sometieron aleatoriamente a tres biopsias calientes y a tres biopsias frías. Todas las muestras biópsicas se obtuvieron con pinzas de biopsia, con y sin la aplicación de una corriente de electrocoagulación, ajustada en modo de coagulación suave (40W). Para cuantificar la hemorragia se utilizó una escala de cuatro puntos. Se solicitó la revisión de todas las muestras a un anatomopatólogo enmascarado para los antecedentes del paciente. Para valorar la lesión de electrocoagulación se usó una escala de tres puntos.
ResultadosSe obtuvo un total de 240 muestras biópsicas de 40 pacientes. La frecuencia de concordancia positiva entre ambos métodos fue del 85%. El grado de lesión de electrocoagulación de las muestras fue: grado 1=52,5%, grado 2=32,5%, y grado 3=15%. Después de la biopsia caliente, la puntuación media de la cuantía de hemorragia fue significativamente más baja en comparación con la de biopsia fría (p=0,006). La concordancia entre el rendimiento diagnóstico de ambas biopsias fue del 85%. No se detectó una diferencia significativa entre los rendimientos diagnósticos de ambos métodos biópsicos (p=0,687).
ConclusionesLas pinzas de biopsia caliente redujeron significativamente la cuantía de la hemorragia relacionada con el procedimiento. La calidad de las muestras no se deterioró significativamente. Por lo que respecta a la baja prevalencia de hemorragia después de biopsia endobronquial, no es razonable el uso sistemático de pinzas para broncoscopia caliente. No obstante, la familiaridad de los broncoscopistas con este método puede mejorar su tolerabilidad.
Despite the development of laboratory techniques and advanced imaging instruments, such as computed tomography (CT), magnetic resonance imaging (MRI) and positron emission tomography (PET), during an examination with flexible bronchoscopy, biopsy with forceps is still the diagnostic method of choice in cases of endobronchial lesions.1 In fact, these new tools can provide information about the location and extension of the mass, rather than its nature.
Bronchoscopy is accompanied by complications like bronchial spasm, arrhythmias, pneumonia and dysphonia; after biopsy, additional complications include increased risk for pneumothorax, hemorrhage, infections and even death.2,3
Traditionally, cold biopsy forceps have been used for endobronchial biopsy, but recently bronchoscopic biopsy forceps with electrocautery (hot biopsy) have also been introduced. It has been hypothesized that hot biopsy forceps may reduce procedure-related hemorrhage after biopsy.1 However, it has also been postulated that electrocautery may reduce the quality of the samples obtained.4
Unfortunately, only a few published studies have dealt with the response to these questions, and their results are controversial.1,4,5
The aim of this present study was to evaluate the effect of hot biopsy forceps on the quality and diagnostic value of the samples, and also to compare procedure-related hemorrhage after biopsy with hot and cold biopsy forceps.
MethodsThe present prospective, controlled study included 40 patients. Each patient was also a control. The objectives and the risks of the study were explained to all the participating patients, and written informed consent was obtained. The research committee from the University of Teheran reviewed and approved the study protocol.
PatientsIncluded for study were successive, cooperative patients over the age of 18, with a visible mass or another indication for endobronchial biopsy during bronchoscopy.
Excluded from the study were those patients treated with anticoagulants, those with uncontrolled obstructive pulmonary disease and/or forced expiratory volume in 1s (FEV1)<800ml, patients in Goldman criteria class 46 and/or an ejection fraction <30%, those with severe hypoxemia (O2 saturation ≤80%), and patients with pacemakers or implanted defibrillators.
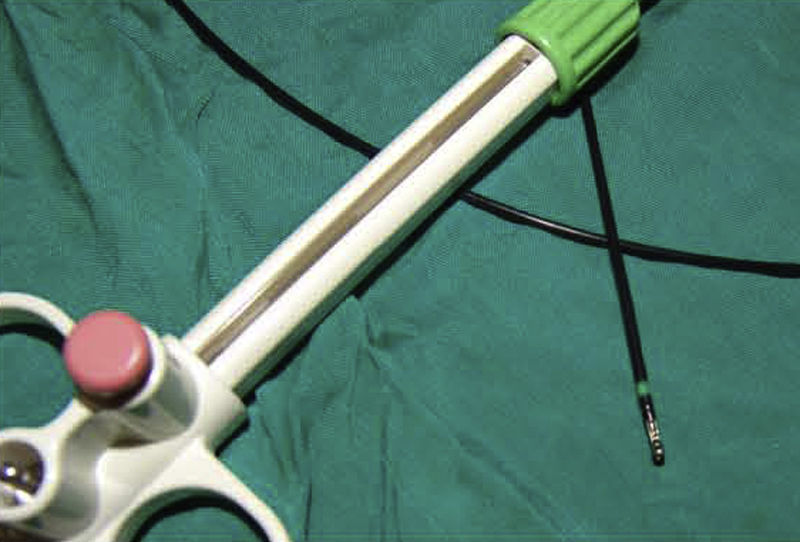
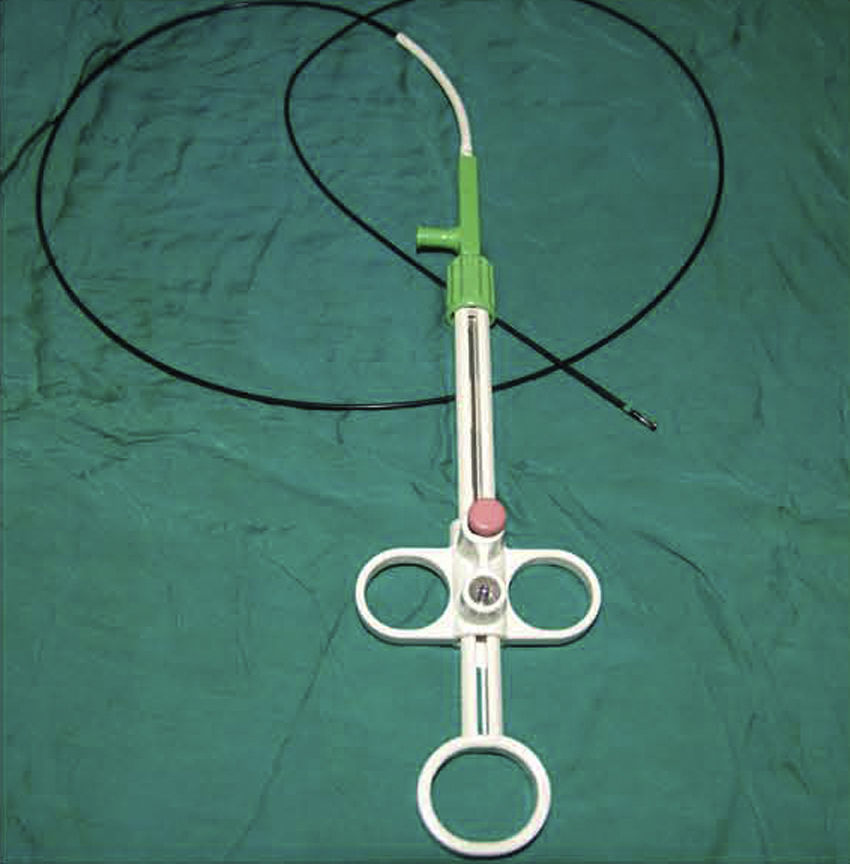
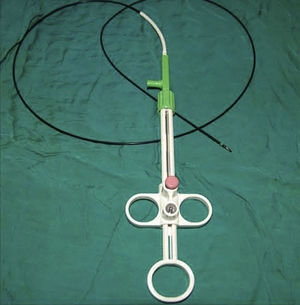
ProcedureThe patients were sedated with an intravenous opiate (fentanyl) and/or a short-acting benzodiazepine (midazolam); in addition, lidocaine was administered by means of inhalation and instillation during the bronchoscopy for the local anesthesia. Before, during and 3h after the bronchoscopy, electrocardiograms were done and both blood pressure and pulse-oximetry were monitored continuously. Before and after bronchoscopy, blood gas was analyzed in arterial blood. All patients underwent bronchoscopy under the previously mentioned circumstances. During the procedure, the patients received oxygen with a mask or cannula. After identifying the location for the biopsy, six biopsy samples were obtained. It has been demonstrated that obtaining three samples is enough to obtain an appropriate diagnostic value7; therefore, we randomly took three hot and three cold biopsies at a 1:1 ratio. In order to generate the random numbers for blocks of 6 numbers, a computer program was used. Immediately afterwards, the samples were put into different containers. All the biopsy samples were obtained with biopsy forceps (FD-7C-1, Olympus Co., Tokyo, Japan) with and without the application of electrocoagulation current (ICC 200 electrosurgical generator, ERBE, Germany), set at soft coagulation mode (40W) (Fig. 1).
A bronchoscopist who was not blinded to the biopsy method observed and registered the rate of hemorrhage. In order to quantify it, a 4-point scale was used. The lack of hemorrhage or a mild hemorrhage that did not require intervention was evaluated as degrees 1 and 2, respectively. The hemorrhages that required intervention, without and with the need to terminate the procedure, were evaluated as degrees 3 and 4, respectively.
PathologyDuring the study, all the biopsy samples were remitted first of all for clinical anatomic pathology, accompanied with the history and clinical findings of the patient. This was done to avoid any interruption in the patient treatment regime, which is usually based on the pathologic diagnosis. Afterwards, all the samples were numbered and stored. At the end of the study, a pathologist who was blinded to the patient medical files reviewed all the samples. To evaluate the quality of the samples obtained by hot biopsy, the pathologist was requested to describe the degree of electrocoagulation injury to the samples. For this evaluation, a three-point scale was used that ranged from 1 (absence of injury or mild injury) to 3 (severe injury). The tissue affectation determined the diagnostic value: when the injury was small, the diagnostic validity was high (degree 1 [high diagnostic value] to degree 3 [low diagnostic value]).
AnalysisThe size of the sample from 40 patients was considered similar to the study by Tremblay et al.1 The mean hemorrhage scores of the three cold and three hot biopsies were compared with the Wilcoxon signed rank test. The agreement was calculated for the diagnostic performance between the hot and cold biopsies. In order to evaluate the diagnostic performance between the two types of biopsies, the McNemar test was used. For all the statistical analyses, the SPSS, version 16 statistical program was used. A difference of 0.05 was considered statistically significant.
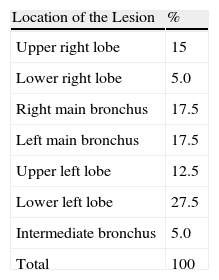
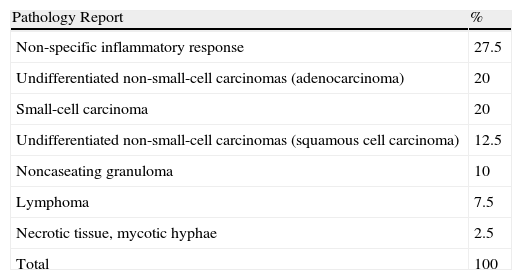
ResultsA total of 240 biopsies were obtained from the 40 patients included in the study. The male:female ratio was 1.85 (26 [65%] men and 14 [35%] women). Mean age was 56.72 (30–88). Tables 1 and 2, respectively, show the location and the final diagnosis of the biopsy samples obtained. Mean±standard deviation of the degree of injury due to electrocoagulation seen in the samples was 1.625±0.74. The degree of electrocoagulation injury in the samples was: grade 1=52.5%, grade 2=32.5%, and grade 3=15%. The diagnostic value of the samples obtained by hot biopsy in six samples was low (grade 3), and the pathologist suggested that the biopsy be repeated in four; nevertheless, the samples obtained with cold biopsy revealed the diagnosis of the patients. The samples obtained with cold biopsy were not diagnosed in two cases, while the pathology examination of the hot biopsy samples revealed the diagnosis. The frequency of positive agreement between the two methods was 85%. The procedure-related hemorrhage after hot biopsy was: grade 1=70.8%, grade 2=27.5%, grade 3=1.7%, and grade 4=0%. For those obtained with cold biopsy, it was: grade 1=52.5%, grade 2=44.2%, grade 3=3.3%, and grade 4=0%.
Final Diagnosis for 40 Patients.
| Pathology Report | % |
| Non-specific inflammatory response | 27.5 |
| Undifferentiated non-small-cell carcinomas (adenocarcinoma) | 20 |
| Small-cell carcinoma | 20 |
| Undifferentiated non-small-cell carcinomas (squamous cell carcinoma) | 12.5 |
| Noncaseating granuloma | 10 |
| Lymphoma | 7.5 |
| Necrotic tissue, mycotic hyphae | 2.5 |
| Total | 100 |
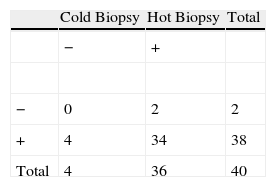
After hot biopsy, the mean hemorrhage score was significantly less in comparison with the cold biopsy (P=.006). The agreement between the diagnostic performances of both was 85%. No significant difference was detected between the diagnostic performances of the two biopsy methods (P=.687), which demonstrates that electrocoagulation produces a minimal deterioration in the quality of the samples (Table 3).
DiscussionDespite the development of new diagnostic instruments, during flexible bronchoscopy biopsy with forceps is still the diagnostic reference method for dealing with endobronchial lesions, and it has a high diagnostic performance.8 After endobronchial biopsy, hemorrhage is exceptional, but it can potentially threaten the life of the patient.3,8 Traditionally, electrocautery (electric scalpel) has been used in different fields for the treatment of hemorrhage. It has also been used in pulmonology, with satisfactory results, for the treatment of hemoptysis and neoplastic obstruction of the respiratory tract.9,10 Today, there are biopsy forceps with electrocautery (hot biopsy) (Figs. 2 and 3), and it has been hypothesized that they could potentially reduce the procedure-related hemorrhage after biopsy.1 However, it has also been postulated that the electric scalpel may reduce the quality of the samples obtained.4,11 Despite the availability of biopsy forceps with electrocautery, bronchoscopists are still not familiar with this instrument. Only a few published studies have dealt with these questions, and their results are controversial.1,4,5
Bronchoscopy biopsy forceps (Fig. 2) with electrocautery (hot biopsy).
The main objective of this present study was to evaluate the effect of hot biopsy forceps on the quality and diagnostic value of tissue samples, and the second objective was to compare the procedure-related hemorrhage after biopsy with cold as well as hot forceps. In the present prospective, controlled study, each patient was also a control subject because the use of the same patient for comparing the diagnostic performance of two sampling methods made it possible to statistically analyze paired data, which is much more powerful compared to the analysis of independent data. Randomized, controlled assays have a satisfactory power for evaluating the hemorrhage related with the procedure because each patient undergoes an individual biopsy technique (cold or hot). As far as we know, this new technique still has not been studied, as carrying out a randomized, controlled assay does not seem ethical from a medical standpoint because the random assignation could deprive half of the patients from receiving the diagnostic reference method (cold biopsy).12
Several factors can affect the diagnostic reliability of bronchial biopsy. The main causes are the clinical state of the patient and the presence of necrosis.13 According to the results of the present study, the quality of the results obtained with hot biopsy forceps has a minimal deterioration. This coincides with the results of another two published studies.1,5 Meanwhile, animal experimentation study by Wahidi et al.4 demonstrated that hot biopsy forceps can affect the quality and the diagnostic value of the samples. In order to raise the reliability of these findings, additional large-scale studies are required.
In our study, after hot biopsy the magnitude of the overall procedure-related hemorrhage was significantly less compared with cold biopsy (P=.006), although this did not seem to be clinically significant. In a similar study published by Tremblay et al.,1 similar results were demonstrated.
In a recently published prospective, randomized, simple blind and controlled study, Khan et al.5 concluded that the hot biopsy forceps did not affect the quality of the samples nor did they reduce the amount of the procedure-related hemorrhage. The results of said study for evaluating the quality of the samples were not satisfactory because an analysis for independent data was used, while the study had enough power to evaluate the magnitude of the procedure-related hemorrhage.12 In this study, after the biopsies there were no severe hemorrhagic episodes. As for the lower prevalence of severe hemorrhage when compared with cold biopsy, it is reasonable to conclude that hot biopsy forceps show a clinically significant reduction.
In theory, and regarding the results of the present study, hot biopsy forceps could improve the tolerance of the procedure, especially in patients with complications, such as those with a coagulation disorder (who were excluded from the present study) or when the biopsy was obtained from a very fragile or hypervascularized mass.1
In this study, a bronchoscopist who was not blinded to the biopsy method evaluated the procedure-related hemorrhage; therefore, there was a tendency towards a certain observer bias. In fact, observer bias is inevitable.
In addition, we documented a high percentage of non-specific inflammatory lesions (27.5%), which could be due to the established inclusion criteria that were not limited to patients with a visible mass during bronchoscopy.
Although a statistically significant difference was not detected between the diagnostic performances of the two biopsy methods (P=.687), in 15% of cases a lack of agreement was seen between the diagnostic performance of both methods, which is an important potential limitation for clinical practice.
In all the patients, both biopsy forceps were used, meaning that each patient was also a control subject. This strategy would not interfere with the histologic diagnostic performance, although with this design both the risk for hemorrhage as well as the results for tolerability should be reconsidered. It is probably very difficult to distinguish and classify the severity of the consecutive hemorrhages after six repeated biopsies in a single lesion during a bronchoscopy procedure. The random assignation is the only way to avoid this limitation, but as has been previously described, this could deprive half the patients of the diagnostic reference method (cold biopsy), and at this time is contrary to medical ethics.
In conclusion, regarding the results of the study, the quality of the sample obtained with hot biopsy forceps does not significantly deteriorate. The amount of the procedure-related hemorrhage was significantly less after hot biopsy compared with the cold biopsy method. As for the low prevalence of hemorrhage after the endobronchial biopsy,1–5 this is not reason enough for the systematic use of bronchoscopy forceps for hot biopsy. Nevertheless, the familiarity of the bronchoscopist with this method may improve the tolerability of bronchoscopy and endobronchial biopsy.
Conflict of InterestsThe authors of this manuscript have no economic or personal relationship that could cause a conflict of interests.
We would like to express our gratitude to the study participants.
Please cite this article as: Firoozbakhsh S, et al. Comparación de las pinzas de biopsia caliente frente a fría en el diagnóstico de lesiones endobronquiales. Arch Bronconeumol. 2011;47:547–51.