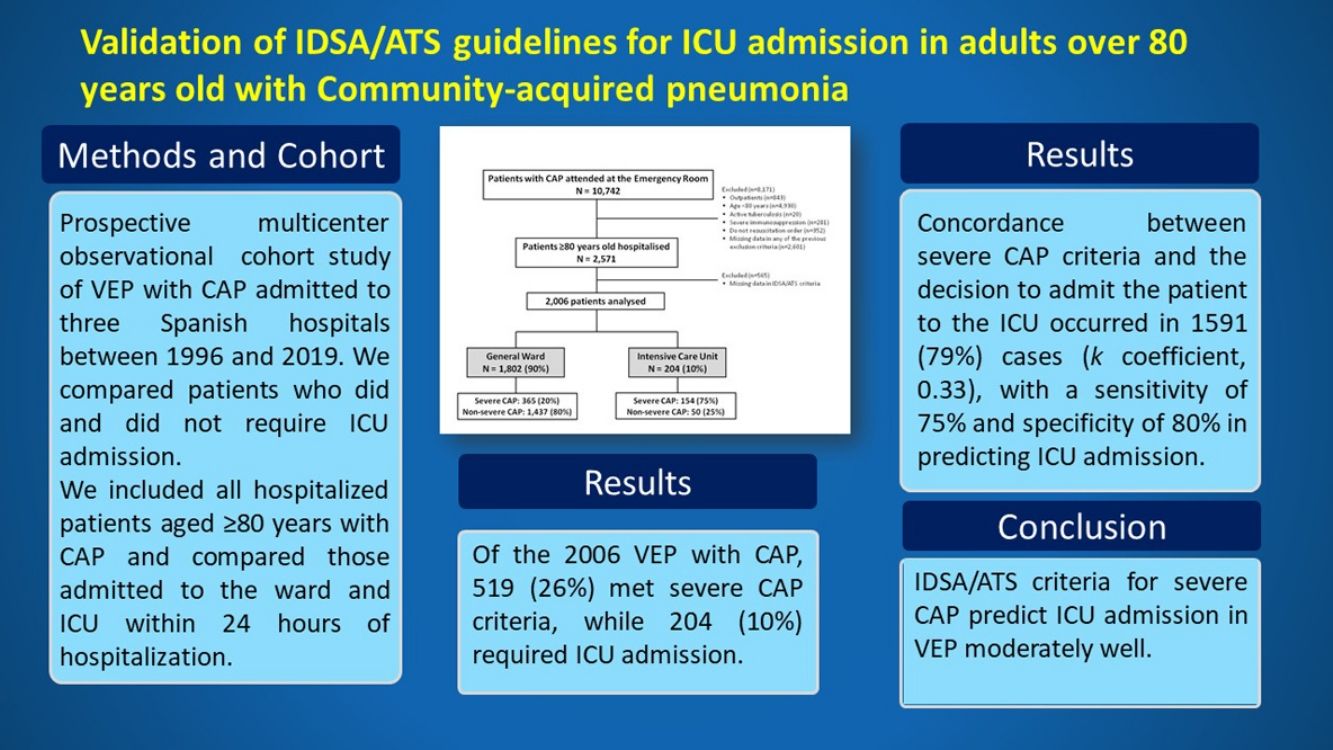
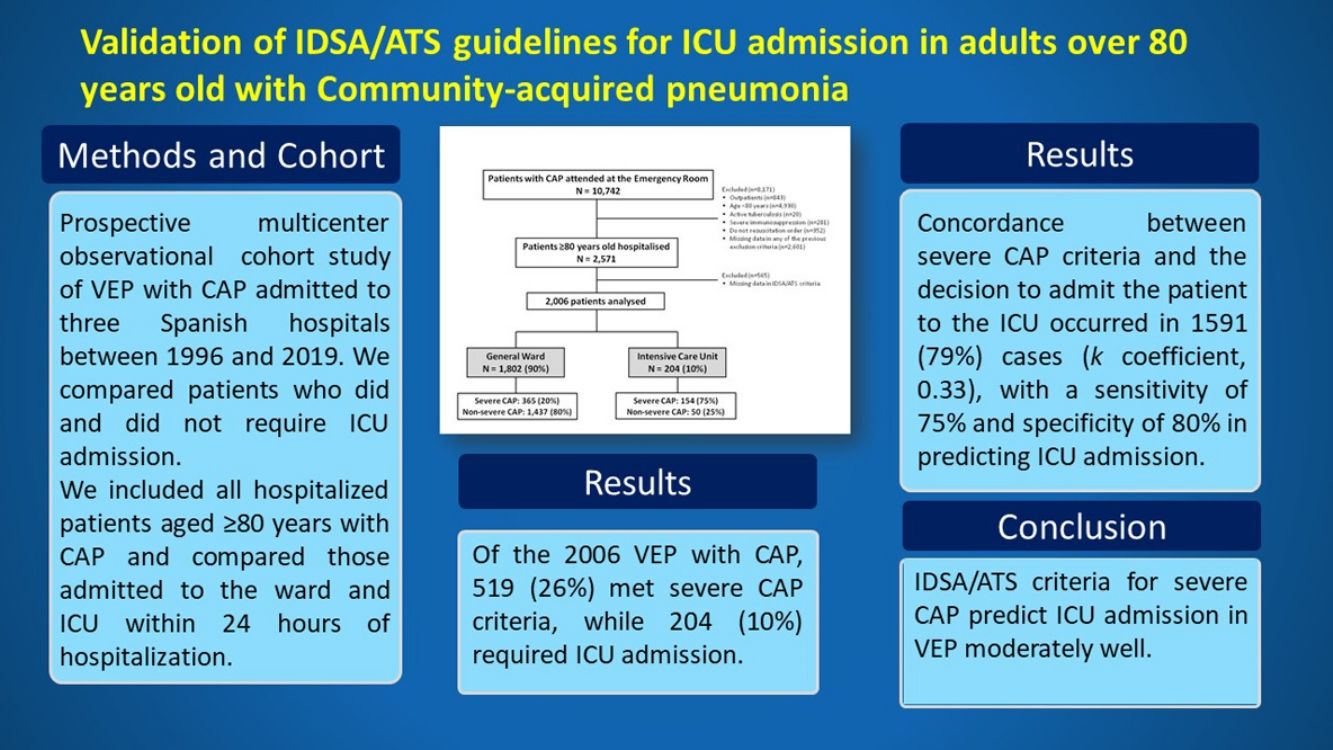
The 2007 IDSA/ATS guidelines for community-acquired pneumonia (CAP) recommended intensive care unit (ICU) admission for adults meeting severe CAP criteria. We aimed to validate the accuracy of IDSA/ATS criteria in patients≥80 years old (very elderly patients, VEP) with CAP.
MethodsProspective cohort study of VEP with CAP admitted to three Spanish hospitals between 1996 and 2019. We compared patients who did and did not require ICU admission. We also assessed factors independently associated with ICU admission, as well as the accuracy of severe CAP criteria for ICU admission and mortality. Major criteria include septic shock and invasive mechanical ventilation while minor criteria encompass other variables related to hemodynamics and respiratory insufficiency as well as level of consciousness, renal function, blood parameters indicative of sepsis and body temperature.
ResultsOf the 2006 VEP with CAP, 519 (26%) met severe CAP criteria, while 204 (10%) required ICU admission. Concordance between severe CAP criteria and the decision to admit the patient to the ICU occurred in 1591 (79%) cases (k coefficient, 0.33), with a sensitivity of 75% and specificity of 80% in predicting ICU admission. All patients with invasive mechanical ventilation received care in ICUs, while 45 (44%) patients with septic shock—previously stabilized in the emergency room—did not. Thirty-day mortality of ICU-admitted patients with septic shock was lower than that of patients in wards (30% vs. 60%, p=0.013). In contrast, patients with severe CAP and only minor criteria had similar mortality.
ConclusionsIDSA/ATS criteria for severe CAP predict ICU admission in VEP moderately well. While patients with septic shock and invasive mechanical ventilation warrant ICU admission, severe CAP without major severity criteria in VEP may be acceptably manageable in wards.
Over the last two decades, due to an increased life expectancy in many countries worldwide, the proportion of critically ill and patients ≥80 years old (very elderly patients: VEP) has grown significantly.1,2 A higher proportion of VEP admitted to the ICU largely impacts healthcare resources and costs.
Community-acquired pneumonia (CAP) is the main cause of sepsis and presents in up to 71% of all critically ill VEP, with an ICU mortality rate of 17%.3,4 However, there are no specific recommendations for managing critically ill VEP with CAP. Moreover, diagnosing CAP in VEP is often difficult and results in frequent delays in antibiotic therapy initiation.5
The most recent CAP guidelines6 issued by the Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) still recommend the use of the diagnostic criteria proposed in 20078 in defining patients with severe CAP requiring ICU admission. This recommendation followed the validation of the criteria by several studies.7–10 However, these severity criteria have not been validated yet in VEP. We hypothesized that IDSA/ATS severity criteria are not appropriate to guide decisions regarding ICU admission in VEP with CAP. The aim of the study was therefore to validate the predictive ability of the 2007 IDSA/ATS criteria for severe CAP in identifying individuals in the VEP population admitted to the ICU.
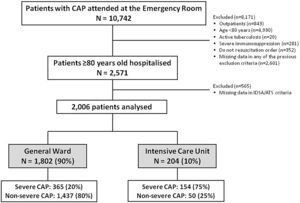
MethodsStudy design and patientsThis is a multicenter observational study based on the analysis of data obtained from a prospective registry of hospitalized patients with CAP. Three teaching hospitals from Spain participated in the study: Hospital Clinic of Barcelona (1996–2019) [n=1635]; Hospital Universitario Cruces (2005–2019) [n=627] and Hospital La Fe of Valencia (2012–2019) [n=309]). We prospectively included all hospitalized patients aged ≥80 years with CAP and compared those admitted to the ward and ICU within 24h of hospitalization. Exclusion criteria were: (1) age <80 years; (2) severe immunosuppression (neutropenia after chemotherapy or hematopoietic transplant; drug-induced immune suppression in solid organ transplant or cytotoxic therapy; oral corticosteroid treatment with at least 20mg prednisone or equivalent per day for at least two weeks; HIV infection); (3) active tuberculosis; and (4) patients with do-not-resuscitate (DNR) orders at the time of ICU admission. Pneumonia was defined as a new pulmonary infiltrate on a chest X-ray at hospital admission, with symptoms and signs of lower respiratory tract infection.11 More details about data collection and microbiological diagnosis are described in the Supplementary Material.
For publication purposes, the study was approved by the IRB of our institutions (Register: HCP2009/5451). Written informed consent was waived due to the non-interventional design of the study.
DefinitionsA prior episode of pneumonia was defined as that occurring within the prior 12 months. Severe CAP was defined when at least one major (septic shock or a need for invasive mechanical ventilation) or 3 minor criteria of the 2007 IDSA/ATS guidelines were present (Supplementary Table S1). IDSA/ATS criteria for severe CAP requiring ICU admission11 used the working definition of “direct ICU admission”, i.e., admission directly from the emergence room in the first 24h after consultation to the hospital. Prior antibiotic treatment was considered when patients had taken antibiotics in the previous month. Polymicrobial pneumonia was defined as more than one pathogen being identified as the causative agent. Septic shock was defined as a systolic blood pressure of <90mmHg and peripheral hypoperfusion with the need for vasopressors for >4h after fluid resuscitation. Appropriateness of empirical antibiotic treatment was defined In all patients based on multidisciplinary guidelines for CAP management.11,12
Outcomes and study groupsThe primary outcome was ICU admission. We divided the study population into two groups: patients hospitalized in the ward and patients admitted to the ICU, including intermediate care units. The secondary outcome was 30-day mortality.
Statistical analysisWe reported the number and percentage of patients as categorical variables, the median (Q1; Q3) as continuous variables with non-normal distributions, and the mean (standard deviation [SD]) as continuous variables with normal distributions. Categorical variables were compared using the chi-squared test or Fisher's exact test, whereas continuous variables were compared using the t-test or non-parametric Mann–Whitney U test.
We also performed univariable and multivariable logistic regression analyses13 to identify variables predictive of ICU admission. Factors showing an association in the univariable analyses (p<0.10) were incorporated into the multivariable regression model. Final variable selection was performed using the backward stepwise selection method (likelihood ratio) (pin<0.05, pout>0.10). Odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated. Single collinearity was evaluated using the Pearson correlation (r) and multicollinearity was examined by means of the variance inflation factor (VIF). Discrimination and calibration were assessed by area under the receiver operating characteristic curve (AUC) and the Hosmer–Lemeshow test, respectively. For the assessment of internal validity, we used ordinary nonparametric bootstrapping with 1000 bootstrap samples and bias-corrected, accelerated 95% CIs.14 We used the multiple imputation method15 for missing data in the analyses to identify variables predictive of ICU admission (Supplementary Table S2). To determine the ability of IDSA/ATS severe CAP criteria to predict ICU admission, we determined sensitivity, specificity and positive and negative likelihood ratio,16 along with 95% CIs. The coincidence between the predictive rule and the clinical decision for ICU admission was assessed with the kappa coefficient of agreement.17 The univariate association of the predictive rule and the severity criteria with ICU admission is also expressed as the relative risk and the 95% CI. The level of significance was set at 0.05 (two-tailed), and all analyses were performed using IBM SPSS Version 26.0 (IBM Corp., Armonk, NY, USA).
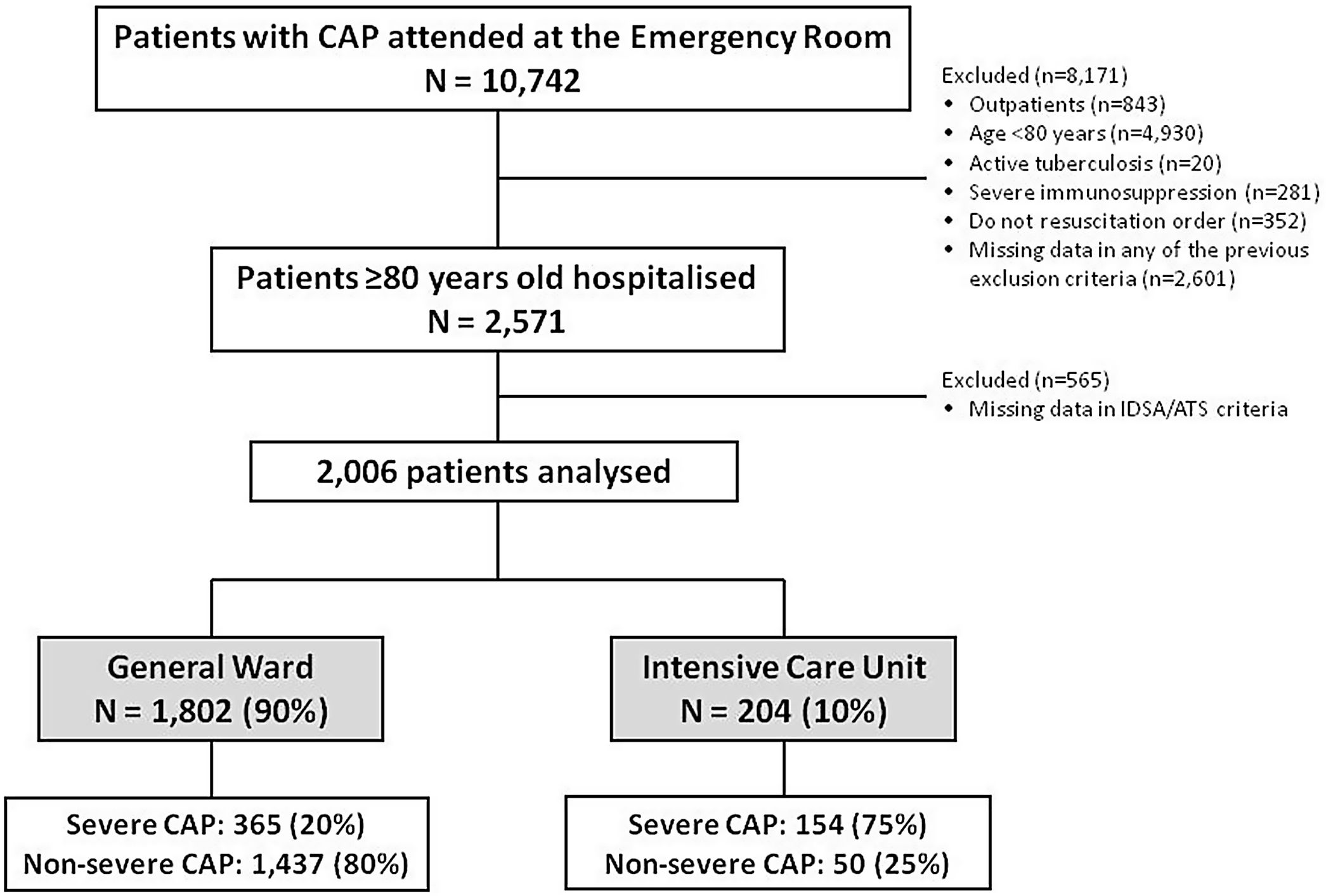
ResultsStudy populationDuring the study period, 10,742 patients with CAP visited the emergency room and 2571 (24%) were hospitalized VEP without a DNR order, of whom 2006 (78%) patients, with a median (Q1; Q3) age of 85 (82; 88) were included in the analysis. 1802 (90%) were admitted to the general ward while 204 (10%) to the ICU (Fig. 1).
The IDSA/ATS criteria identified 519 (26%) of this series of patients as having severe CAP: 58 (11%) had major severity criteria only; 84 (16%) had major and at least one minor severity criteria; and, in the absence of major criteria, 377 (73%) had three or more minor severity criteria. Of those 519 patients with severe CAP, 154 (30%) were admitted to the ICU. Only 50 (3%) of the 1487 patients who were defined as not having severe CAP received ICU admission.
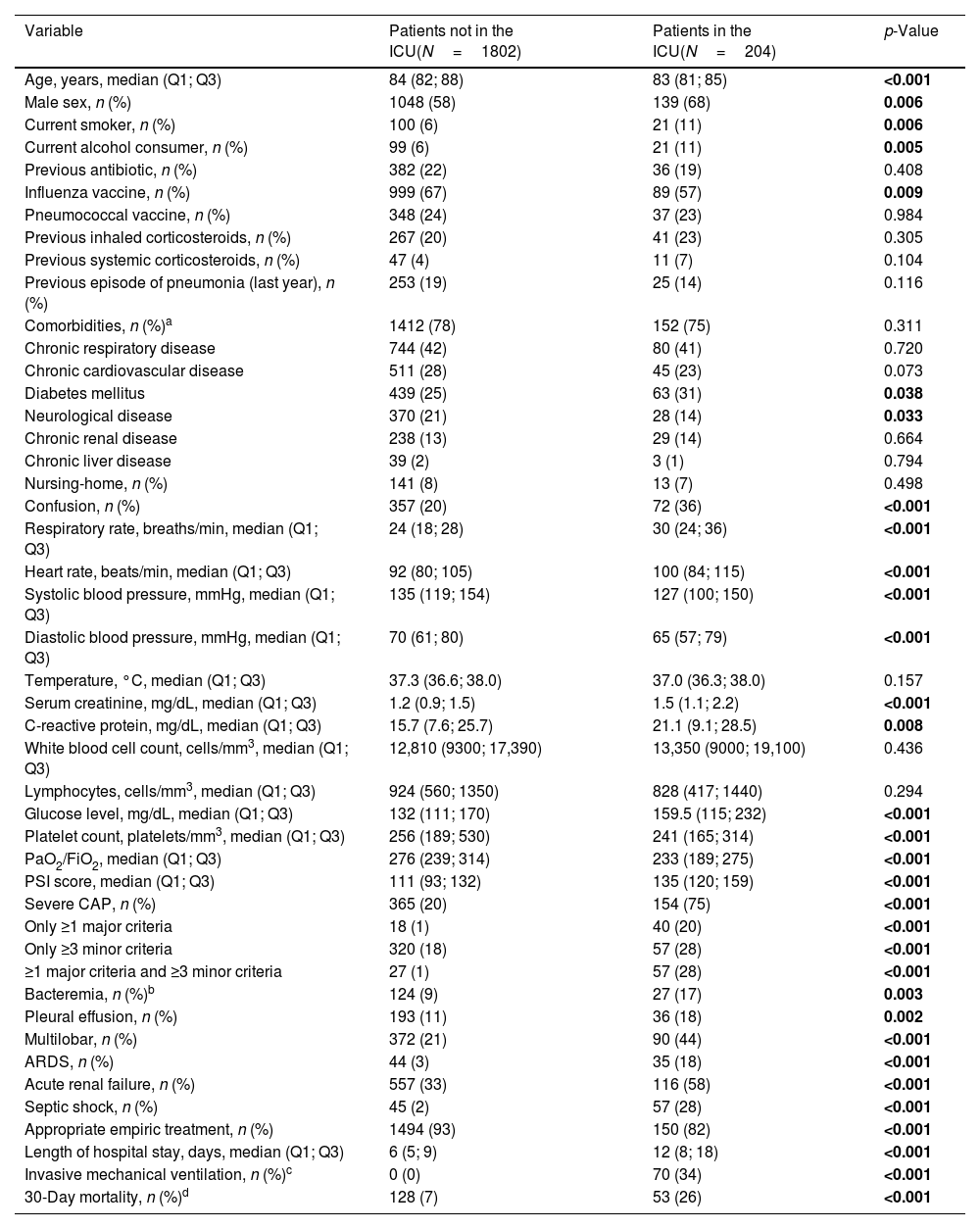
Patient characteristicsThe main clinical characteristics of the study population are shown in Table 1. Patients admitted to the ICU were younger, more often males, and more frequently smoked and abused alcohol. Conversely, when compared to those patients who were not admitted to ICU, those admitted to the ICU had received the influenza vaccine less frequently; were less likely to have chronic neurological diseases; and presented higher rates of diabetes mellitus, altered mental status, higher levels of creatinine, C-reactive protein and serum glucose, and a lower platelet count and PaO2/FiO2. Additionally, when compared to non-ICU-admitted patients, patients admitted to the ICU had higher PSI score; presented severe CAP criteria more frequently; and experienced more pulmonary and extra-pulmonary complications, longer hospital stay and higher 30-day mortality.
Characteristics of the study population by site of care.
| Variable | Patients not in the ICU(N=1802) | Patients in the ICU(N=204) | p-Value |
|---|---|---|---|
| Age, years, median (Q1; Q3) | 84 (82; 88) | 83 (81; 85) | <0.001 |
| Male sex, n (%) | 1048 (58) | 139 (68) | 0.006 |
| Current smoker, n (%) | 100 (6) | 21 (11) | 0.006 |
| Current alcohol consumer, n (%) | 99 (6) | 21 (11) | 0.005 |
| Previous antibiotic, n (%) | 382 (22) | 36 (19) | 0.408 |
| Influenza vaccine, n (%) | 999 (67) | 89 (57) | 0.009 |
| Pneumococcal vaccine, n (%) | 348 (24) | 37 (23) | 0.984 |
| Previous inhaled corticosteroids, n (%) | 267 (20) | 41 (23) | 0.305 |
| Previous systemic corticosteroids, n (%) | 47 (4) | 11 (7) | 0.104 |
| Previous episode of pneumonia (last year), n (%) | 253 (19) | 25 (14) | 0.116 |
| Comorbidities, n (%)a | 1412 (78) | 152 (75) | 0.311 |
| Chronic respiratory disease | 744 (42) | 80 (41) | 0.720 |
| Chronic cardiovascular disease | 511 (28) | 45 (23) | 0.073 |
| Diabetes mellitus | 439 (25) | 63 (31) | 0.038 |
| Neurological disease | 370 (21) | 28 (14) | 0.033 |
| Chronic renal disease | 238 (13) | 29 (14) | 0.664 |
| Chronic liver disease | 39 (2) | 3 (1) | 0.794 |
| Nursing-home, n (%) | 141 (8) | 13 (7) | 0.498 |
| Confusion, n (%) | 357 (20) | 72 (36) | <0.001 |
| Respiratory rate, breaths/min, median (Q1; Q3) | 24 (18; 28) | 30 (24; 36) | <0.001 |
| Heart rate, beats/min, median (Q1; Q3) | 92 (80; 105) | 100 (84; 115) | <0.001 |
| Systolic blood pressure, mmHg, median (Q1; Q3) | 135 (119; 154) | 127 (100; 150) | <0.001 |
| Diastolic blood pressure, mmHg, median (Q1; Q3) | 70 (61; 80) | 65 (57; 79) | <0.001 |
| Temperature, °C, median (Q1; Q3) | 37.3 (36.6; 38.0) | 37.0 (36.3; 38.0) | 0.157 |
| Serum creatinine, mg/dL, median (Q1; Q3) | 1.2 (0.9; 1.5) | 1.5 (1.1; 2.2) | <0.001 |
| C-reactive protein, mg/dL, median (Q1; Q3) | 15.7 (7.6; 25.7) | 21.1 (9.1; 28.5) | 0.008 |
| White blood cell count, cells/mm3, median (Q1; Q3) | 12,810 (9300; 17,390) | 13,350 (9000; 19,100) | 0.436 |
| Lymphocytes, cells/mm3, median (Q1; Q3) | 924 (560; 1350) | 828 (417; 1440) | 0.294 |
| Glucose level, mg/dL, median (Q1; Q3) | 132 (111; 170) | 159.5 (115; 232) | <0.001 |
| Platelet count, platelets/mm3, median (Q1; Q3) | 256 (189; 530) | 241 (165; 314) | <0.001 |
| PaO2/FiO2, median (Q1; Q3) | 276 (239; 314) | 233 (189; 275) | <0.001 |
| PSI score, median (Q1; Q3) | 111 (93; 132) | 135 (120; 159) | <0.001 |
| Severe CAP, n (%) | 365 (20) | 154 (75) | <0.001 |
| Only ≥1 major criteria | 18 (1) | 40 (20) | <0.001 |
| Only ≥3 minor criteria | 320 (18) | 57 (28) | <0.001 |
| ≥1 major criteria and ≥3 minor criteria | 27 (1) | 57 (28) | <0.001 |
| Bacteremia, n (%)b | 124 (9) | 27 (17) | 0.003 |
| Pleural effusion, n (%) | 193 (11) | 36 (18) | 0.002 |
| Multilobar, n (%) | 372 (21) | 90 (44) | <0.001 |
| ARDS, n (%) | 44 (3) | 35 (18) | <0.001 |
| Acute renal failure, n (%) | 557 (33) | 116 (58) | <0.001 |
| Septic shock, n (%) | 45 (2) | 57 (28) | <0.001 |
| Appropriate empiric treatment, n (%) | 1494 (93) | 150 (82) | <0.001 |
| Length of hospital stay, days, median (Q1; Q3) | 6 (5; 9) | 12 (8; 18) | <0.001 |
| Invasive mechanical ventilation, n (%)c | 0 (0) | 70 (34) | <0.001 |
| 30-Day mortality, n (%)d | 128 (7) | 53 (26) | <0.001 |
Abbreviations: ARDS indicates acute respiratory distress syndrome; CAP, community-acquired pneumonia; FiO2, fraction of inspired oxygen; ICU, intensive care unit; PaO2, partial pressure of arterial oxygen; PSI, pneumonia severity index; Q1, first quartile; Q3, third quartile. Percentages calculated on non-missing data. p-Values marked in bold indicate numbers that they are statistically significant within the 95% confidence limit.
ICU-admitted patients had a higher rate of etiological diagnosis than non-ICU patients (Supplementary Table S3). However, we did not find any significant differences regarding the relative proportion of causative pathogens between ICU and non-ICU patients.
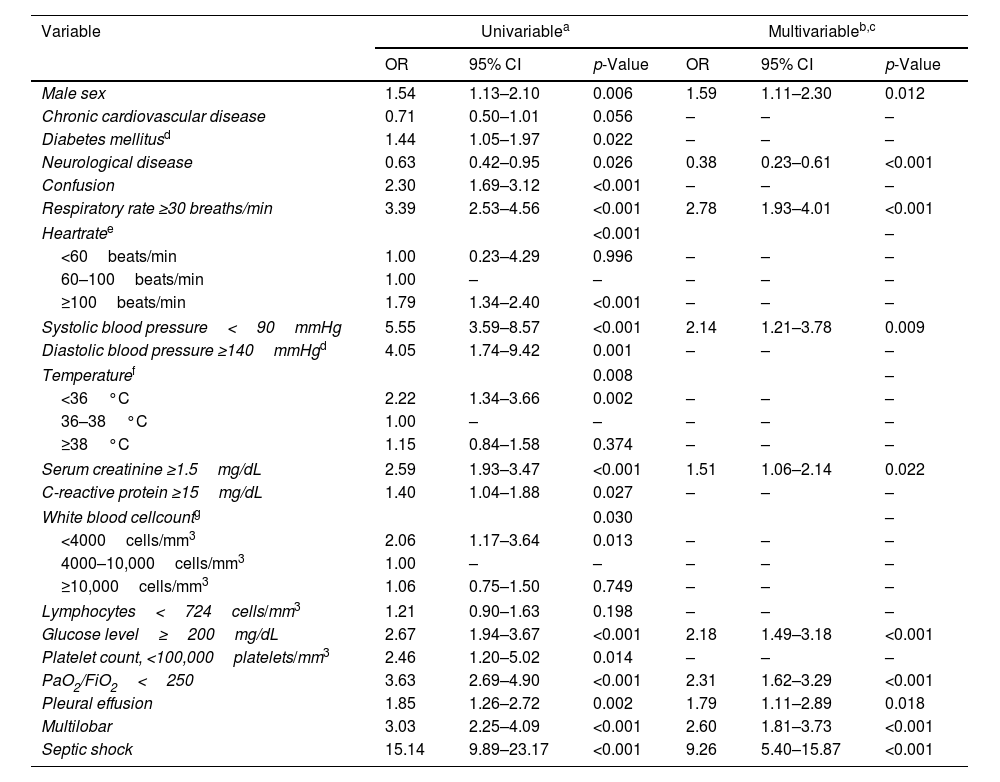
Predictors of ICU admissionLogistic regression analysis indicated that male sex, absence of chronic neurological disease, respiratory rate ≥30breath/min, systolic blood pressure <90mmHg, serum creatinine ≥1.5mg/dL, serum glucose ≥200mg/dL, PaO2/FiO2<250, pleural effusion, multilobar infiltration and septic shock were independently associated with ICU admission (Table 2). The AUC for the ICU admission prediction model was 0.86 (95% CI 0.84–0.89). Internal validation of the final model demonstrated robust results (Supplementary Table S4).
Significant univariable logistic regression analyses for variables associated with ICU admission and independent predictors of ICU admission determined by multivariable logistic regression analysis (N=2006).
| Variable | Univariablea | Multivariableb,c | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Male sex | 1.54 | 1.13–2.10 | 0.006 | 1.59 | 1.11–2.30 | 0.012 |
| Chronic cardiovascular disease | 0.71 | 0.50–1.01 | 0.056 | – | – | – |
| Diabetes mellitusd | 1.44 | 1.05–1.97 | 0.022 | – | – | – |
| Neurological disease | 0.63 | 0.42–0.95 | 0.026 | 0.38 | 0.23–0.61 | <0.001 |
| Confusion | 2.30 | 1.69–3.12 | <0.001 | – | – | – |
| Respiratory rate ≥30 breaths/min | 3.39 | 2.53–4.56 | <0.001 | 2.78 | 1.93–4.01 | <0.001 |
| Heartratee | <0.001 | – | ||||
| <60beats/min | 1.00 | 0.23–4.29 | 0.996 | – | – | – |
| 60–100beats/min | 1.00 | – | – | – | – | – |
| ≥100beats/min | 1.79 | 1.34–2.40 | <0.001 | – | – | – |
| Systolic blood pressure<90mmHg | 5.55 | 3.59–8.57 | <0.001 | 2.14 | 1.21–3.78 | 0.009 |
| Diastolic blood pressure ≥140mmHgd | 4.05 | 1.74–9.42 | 0.001 | – | – | – |
| Temperaturef | 0.008 | – | ||||
| <36°C | 2.22 | 1.34–3.66 | 0.002 | – | – | – |
| 36–38°C | 1.00 | – | – | – | – | – |
| ≥38°C | 1.15 | 0.84–1.58 | 0.374 | – | – | – |
| Serum creatinine ≥1.5mg/dL | 2.59 | 1.93–3.47 | <0.001 | 1.51 | 1.06–2.14 | 0.022 |
| C-reactive protein ≥15mg/dL | 1.40 | 1.04–1.88 | 0.027 | – | – | – |
| White blood cellcountg | 0.030 | – | ||||
| <4000cells/mm3 | 2.06 | 1.17–3.64 | 0.013 | – | – | – |
| 4000–10,000cells/mm3 | 1.00 | – | – | – | – | – |
| ≥10,000cells/mm3 | 1.06 | 0.75–1.50 | 0.749 | – | – | – |
| Lymphocytes<724cells/mm3 | 1.21 | 0.90–1.63 | 0.198 | – | – | – |
| Glucose level≥200mg/dL | 2.67 | 1.94–3.67 | <0.001 | 2.18 | 1.49–3.18 | <0.001 |
| Platelet count, <100,000platelets/mm3 | 2.46 | 1.20–5.02 | 0.014 | – | – | – |
| PaO2/FiO2<250 | 3.63 | 2.69–4.90 | <0.001 | 2.31 | 1.62–3.29 | <0.001 |
| Pleural effusion | 1.85 | 1.26–2.72 | 0.002 | 1.79 | 1.11–2.89 | 0.018 |
| Multilobar | 3.03 | 2.25–4.09 | <0.001 | 2.60 | 1.81–3.73 | <0.001 |
| Septic shock | 15.14 | 9.89–23.17 | <0.001 | 9.26 | 5.40–15.87 | <0.001 |
Abbreviations: CI indicates confidence interval; FiO2, fraction of inspired oxygen; ICU, intensive care unit; OR, odds ratio; PaO2, partial pressure of arterial oxygen. Data are shown as estimated ORs (95% CIs) of the explanatory variables in the ICU admission group. The OR represents the odds that the presence of ICU admission will occur given exposure of the explanatory variable, compared to the odds of the outcome occurring in the absence of that exposure. The p-value is based on the null hypothesis that all ORs relating to an explanatory variable equal unity (no effect).
The variables analyzed in the univariable analyses were sex, antibiotic use in the last week, chronic pulmonary disease, chronic cardiovascular disease, chronic renal disease, chronic liver disease, diabetes mellitus, neurological disease, confusion, respiratory rate, heart rate, systolic blood pressure, diastolic blood pressure, temperature, creatinine, C-reactive protein, lymphocytes, white blood cell count, glucose level, platelet count, PaO2/FiO2, pleural effusion, multilobar infiltration, and septic shock.
Hosmer–Lemeshow goodness-of-fit test, p=0.800. Area under the ROC curve, AUC=0.86 (95% CI 0.84–0.89).
Diabetes mellitus was excluded from the multivariable analysis because of collinearity with glucose level, while diastolic blood pressure was omitted because systolic blood pressure collinearity.
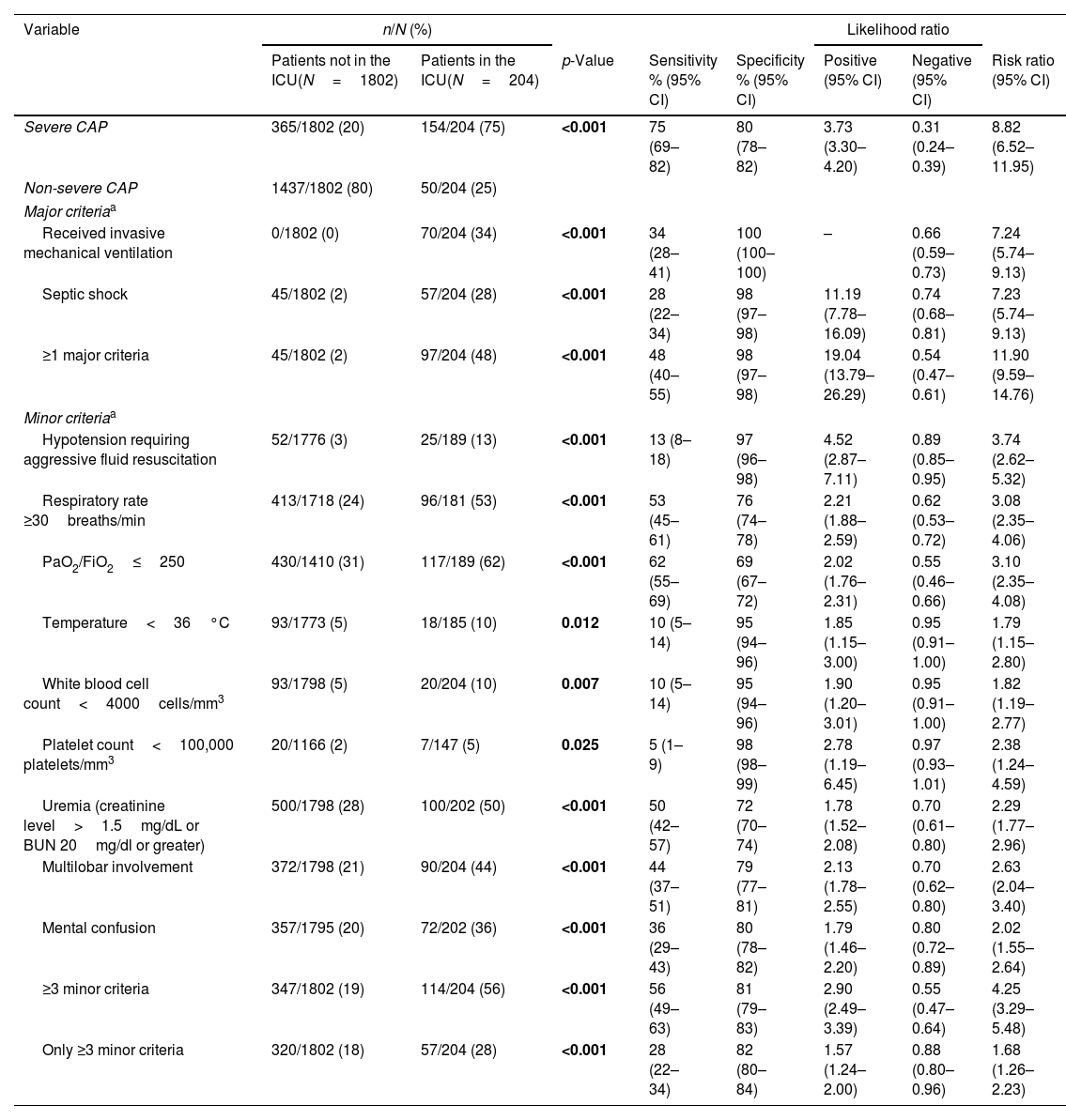
Concordance between IDSA/ATS criteria for severe CAP and ICU admission occurred in 1591 (79%) cases; the kappa coefficient was 0.33 (p<0.001). The predictive rule overestimated the number of patients who would be admitted to the ICU, i.e., 365 (20%) patients who were not admitted to the ICU had severe CAP criteria, whereas only 50 (25%) ICU-admitted patients had non-severe CAP.
Infectious Diseases Society of America/American Thoracic Society guidelines criteria for severe CAP and operative indices to predict ICU admission.
| Variable | n/N (%) | Likelihood ratio | ||||||
|---|---|---|---|---|---|---|---|---|
| Patients not in the ICU(N=1802) | Patients in the ICU(N=204) | p-Value | Sensitivity % (95% CI) | Specificity % (95% CI) | Positive (95% CI) | Negative (95% CI) | Risk ratio (95% CI) | |
| Severe CAP | 365/1802 (20) | 154/204 (75) | <0.001 | 75 (69–82) | 80 (78–82) | 3.73 (3.30–4.20) | 0.31 (0.24–0.39) | 8.82 (6.52–11.95) |
| Non-severe CAP | 1437/1802 (80) | 50/204 (25) | ||||||
| Major criteriaa | ||||||||
| Received invasive mechanical ventilation | 0/1802 (0) | 70/204 (34) | <0.001 | 34 (28–41) | 100 (100–100) | – | 0.66 (0.59–0.73) | 7.24 (5.74–9.13) |
| Septic shock | 45/1802 (2) | 57/204 (28) | <0.001 | 28 (22–34) | 98 (97–98) | 11.19 (7.78–16.09) | 0.74 (0.68–0.81) | 7.23 (5.74–9.13) |
| ≥1 major criteria | 45/1802 (2) | 97/204 (48) | <0.001 | 48 (40–55) | 98 (97–98) | 19.04 (13.79–26.29) | 0.54 (0.47–0.61) | 11.90 (9.59–14.76) |
| Minor criteriaa | ||||||||
| Hypotension requiring aggressive fluid resuscitation | 52/1776 (3) | 25/189 (13) | <0.001 | 13 (8–18) | 97 (96–98) | 4.52 (2.87–7.11) | 0.89 (0.85–0.95) | 3.74 (2.62–5.32) |
| Respiratory rate ≥30breaths/min | 413/1718 (24) | 96/181 (53) | <0.001 | 53 (45–61) | 76 (74–78) | 2.21 (1.88–2.59) | 0.62 (0.53–0.72) | 3.08 (2.35–4.06) |
| PaO2/FiO2≤250 | 430/1410 (31) | 117/189 (62) | <0.001 | 62 (55–69) | 69 (67–72) | 2.02 (1.76–2.31) | 0.55 (0.46–0.66) | 3.10 (2.35–4.08) |
| Temperature<36°C | 93/1773 (5) | 18/185 (10) | 0.012 | 10 (5–14) | 95 (94–96) | 1.85 (1.15–3.00) | 0.95 (0.91–1.00) | 1.79 (1.15–2.80) |
| White blood cell count<4000cells/mm3 | 93/1798 (5) | 20/204 (10) | 0.007 | 10 (5–14) | 95 (94–96) | 1.90 (1.20–3.01) | 0.95 (0.91–1.00) | 1.82 (1.19–2.77) |
| Platelet count<100,000 platelets/mm3 | 20/1166 (2) | 7/147 (5) | 0.025 | 5 (1–9) | 98 (98–99) | 2.78 (1.19–6.45) | 0.97 (0.93–1.01) | 2.38 (1.24–4.59) |
| Uremia (creatinine level>1.5mg/dL or BUN 20mg/dl or greater) | 500/1798 (28) | 100/202 (50) | <0.001 | 50 (42–57) | 72 (70–74) | 1.78 (1.52–2.08) | 0.70 (0.61–0.80) | 2.29 (1.77–2.96) |
| Multilobar involvement | 372/1798 (21) | 90/204 (44) | <0.001 | 44 (37–51) | 79 (77–81) | 2.13 (1.78–2.55) | 0.70 (0.62–0.80) | 2.63 (2.04–3.40) |
| Mental confusion | 357/1795 (20) | 72/202 (36) | <0.001 | 36 (29–43) | 80 (78–82) | 1.79 (1.46–2.20) | 0.80 (0.72–0.89) | 2.02 (1.55–2.64) |
| ≥3 minor criteria | 347/1802 (19) | 114/204 (56) | <0.001 | 56 (49–63) | 81 (79–83) | 2.90 (2.49–3.39) | 0.55 (0.47–0.64) | 4.25 (3.29–5.48) |
| Only ≥3 minor criteria | 320/1802 (18) | 57/204 (28) | <0.001 | 28 (22–34) | 82 (80–84) | 1.57 (1.24–2.00) | 0.88 (0.80–0.96) | 1.68 (1.26–2.23) |
Abbreviations: BUN indicates blood urea nitrogen; CAP, community-acquired pneumonia; FiO2, fraction of inspired oxygen; ICU, intensive care unit; PaO2, partial pressure of arterial oxygen. p-Values marked in bold indicate numbers that are statistically significant within the 95% confidence limit.
Sensitivity and specificity of IDSA/ATS criteria for severe CAP in identifying patients admitted to ICUs were 75% and 80%, respectively. Severe CAP was 3.73 times more frequent among ICU-admitted patients compared to those not admitted to the ICU. Likewise, the probability that ICU-admitted patients had non-severe CAP was only 0.31, when compared to non-ICU patients. Compared with patients with non-severe CAP, patients with severe CAP had an 8.82-fold higher relative risk of ICU admission.
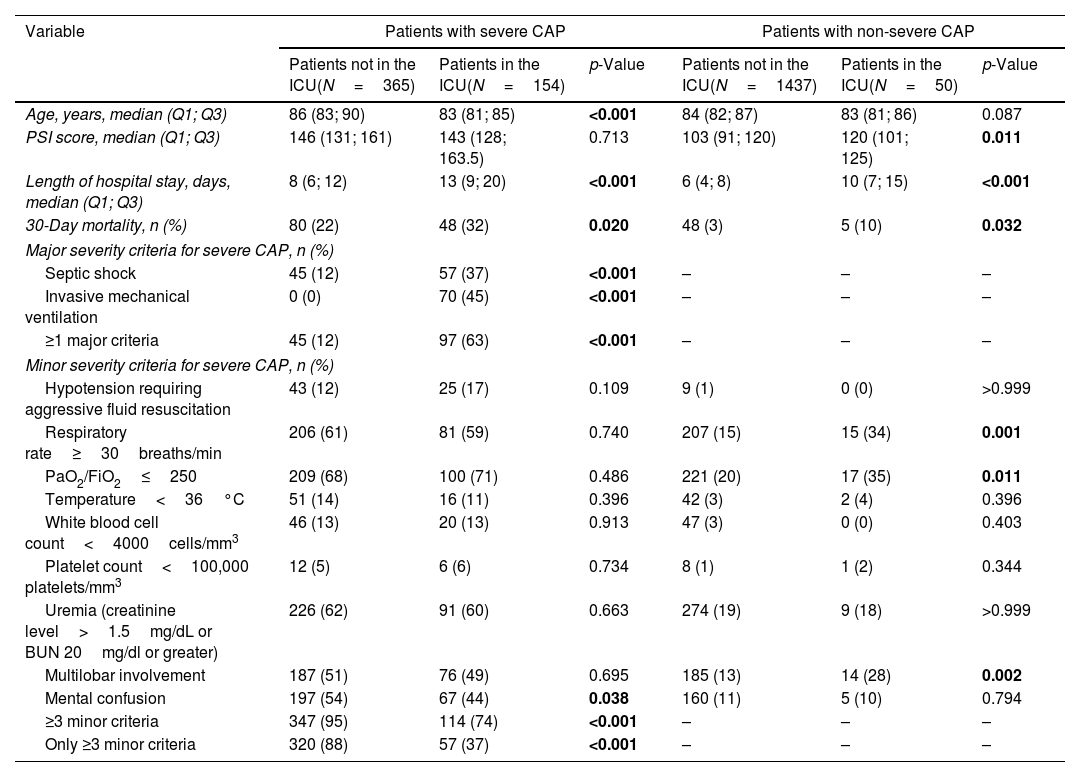
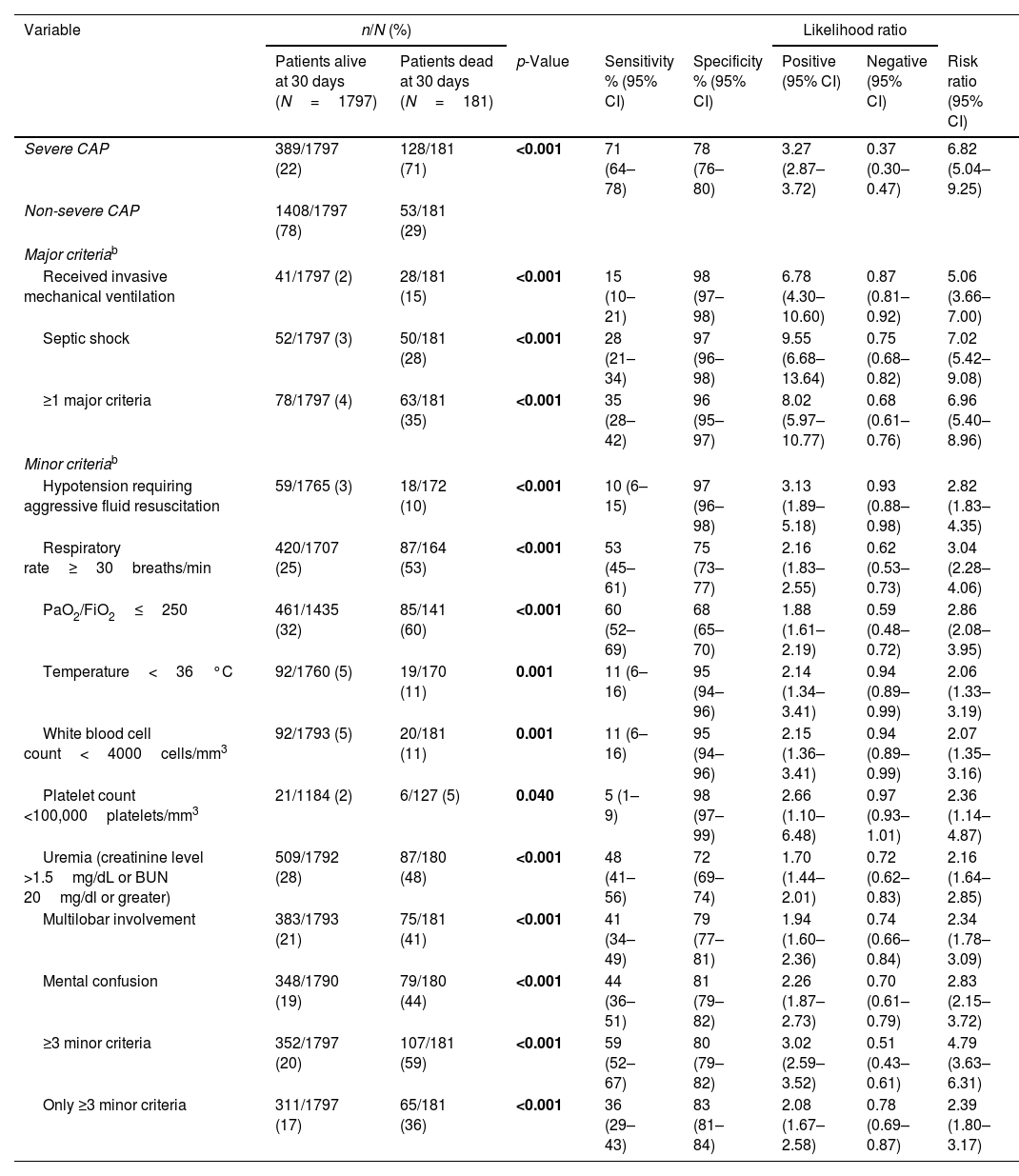
Severe CAP and prediction of mortalityThirty-day mortality was higher among ICU-admitted patients than in those not admitted to the ICU (p<0.001; Table 1). Differences in mortality between groups remained unchanged when analyzing patients with severe and non-severe CAP separately (Table 3). Table 5 shows the association between the predictive rule and mortality. Severe CAP and the presence of either of the two major severity criteria had the strongest association with mortality. All minor severity criteria were also significantly associated with 30-day mortality. Sensitivity, specificity, positive and negative likelihood ratios, and the risk ratio of severe CAP criteria in predicting 30-day mortality were similar to those of patients admitted to the ICU.
Association of the predictive rule of severe CAP and other indices with 30-day mortality a
| Variable | n/N (%) | Likelihood ratio | ||||||
|---|---|---|---|---|---|---|---|---|
| Patients alive at 30 days (N=1797) | Patients dead at 30 days (N=181) | p-Value | Sensitivity % (95% CI) | Specificity % (95% CI) | Positive (95% CI) | Negative (95% CI) | Risk ratio (95% CI) | |
| Severe CAP | 389/1797 (22) | 128/181 (71) | <0.001 | 71 (64–78) | 78 (76–80) | 3.27 (2.87–3.72) | 0.37 (0.30–0.47) | 6.82 (5.04–9.25) |
| Non-severe CAP | 1408/1797 (78) | 53/181 (29) | ||||||
| Major criteriab | ||||||||
| Received invasive mechanical ventilation | 41/1797 (2) | 28/181 (15) | <0.001 | 15 (10–21) | 98 (97–98) | 6.78 (4.30–10.60) | 0.87 (0.81–0.92) | 5.06 (3.66–7.00) |
| Septic shock | 52/1797 (3) | 50/181 (28) | <0.001 | 28 (21–34) | 97 (96–98) | 9.55 (6.68–13.64) | 0.75 (0.68–0.82) | 7.02 (5.42–9.08) |
| ≥1 major criteria | 78/1797 (4) | 63/181 (35) | <0.001 | 35 (28–42) | 96 (95–97) | 8.02 (5.97–10.77) | 0.68 (0.61–0.76) | 6.96 (5.40–8.96) |
| Minor criteriab | ||||||||
| Hypotension requiring aggressive fluid resuscitation | 59/1765 (3) | 18/172 (10) | <0.001 | 10 (6–15) | 97 (96–98) | 3.13 (1.89–5.18) | 0.93 (0.88–0.98) | 2.82 (1.83–4.35) |
| Respiratory rate≥30breaths/min | 420/1707 (25) | 87/164 (53) | <0.001 | 53 (45–61) | 75 (73–77) | 2.16 (1.83–2.55) | 0.62 (0.53–0.73) | 3.04 (2.28–4.06) |
| PaO2/FiO2≤250 | 461/1435 (32) | 85/141 (60) | <0.001 | 60 (52–69) | 68 (65–70) | 1.88 (1.61–2.19) | 0.59 (0.48–0.72) | 2.86 (2.08–3.95) |
| Temperature<36°C | 92/1760 (5) | 19/170 (11) | 0.001 | 11 (6–16) | 95 (94–96) | 2.14 (1.34–3.41) | 0.94 (0.89–0.99) | 2.06 (1.33–3.19) |
| White blood cell count<4000cells/mm3 | 92/1793 (5) | 20/181 (11) | 0.001 | 11 (6–16) | 95 (94–96) | 2.15 (1.36–3.41) | 0.94 (0.89–0.99) | 2.07 (1.35–3.16) |
| Platelet count <100,000platelets/mm3 | 21/1184 (2) | 6/127 (5) | 0.040 | 5 (1–9) | 98 (97–99) | 2.66 (1.10–6.48) | 0.97 (0.93–1.01) | 2.36 (1.14–4.87) |
| Uremia (creatinine level >1.5mg/dL or BUN 20mg/dl or greater) | 509/1792 (28) | 87/180 (48) | <0.001 | 48 (41–56) | 72 (69–74) | 1.70 (1.44–2.01) | 0.72 (0.62–0.83) | 2.16 (1.64–2.85) |
| Multilobar involvement | 383/1793 (21) | 75/181 (41) | <0.001 | 41 (34–49) | 79 (77–81) | 1.94 (1.60–2.36) | 0.74 (0.66–0.84) | 2.34 (1.78–3.09) |
| Mental confusion | 348/1790 (19) | 79/180 (44) | <0.001 | 44 (36–51) | 81 (79–82) | 2.26 (1.87–2.73) | 0.70 (0.61–0.79) | 2.83 (2.15–3.72) |
| ≥3 minor criteria | 352/1797 (20) | 107/181 (59) | <0.001 | 59 (52–67) | 80 (79–82) | 3.02 (2.59–3.52) | 0.51 (0.43–0.61) | 4.79 (3.63–6.31) |
| Only ≥3 minor criteria | 311/1797 (17) | 65/181 (36) | <0.001 | 36 (29–43) | 83 (81–84) | 2.08 (1.67–2.58) | 0.78 (0.69–0.87) | 2.39 (1.80–3.17) |
Abbreviations: BUN indicates blood urea nitrogen; CAP, community-acquired pneumonia; FiO2, fraction of inspired oxygen; ICU, intensive care unit; PaO2, partial pressure of arterial oxygen. p-Values marked in bold indicate numbers that are statistically significant within the 95% confidence limit.
Major severity criteria had the highest association with ICU admission, particularly invasive mechanical ventilation. However, 45 (44%) patients with septic shock who were initially managed and stabilized in the emergency department did not require subsequent ICU admission. In patients with septic shock, 72 (71%) did not receive invasive mechanical ventilation, and these had similar median PSI scores irrespective of their likelihood of ICU admission. However, 30-day mortality was lower in patients with septic shock admitted to the ICU (8 [30%] vs. 27 [60%], p=0.013).
In contrast, the 377 patients with severe CAP defined by the presence of ≥3 minor criteria in the absence of major criteria, less often were admitted to the ICU (Table 4). In this subset of patients, while the PSI score was lower in ICU-admitted patients (138 [123; 154] vs. 145 [130; 160], p=0.045), 30-day mortality was similar (12 [21%] vs. 53 [17%], p=0.37).
Characteristics of patients with severe and non-severe CAP in relation to hospital site of care.
| Variable | Patients with severe CAP | Patients with non-severe CAP | ||||
|---|---|---|---|---|---|---|
| Patients not in the ICU(N=365) | Patients in the ICU(N=154) | p-Value | Patients not in the ICU(N=1437) | Patients in the ICU(N=50) | p-Value | |
| Age, years, median (Q1; Q3) | 86 (83; 90) | 83 (81; 85) | <0.001 | 84 (82; 87) | 83 (81; 86) | 0.087 |
| PSI score, median (Q1; Q3) | 146 (131; 161) | 143 (128; 163.5) | 0.713 | 103 (91; 120) | 120 (101; 125) | 0.011 |
| Length of hospital stay, days, median (Q1; Q3) | 8 (6; 12) | 13 (9; 20) | <0.001 | 6 (4; 8) | 10 (7; 15) | <0.001 |
| 30-Day mortality, n (%) | 80 (22) | 48 (32) | 0.020 | 48 (3) | 5 (10) | 0.032 |
| Major severity criteria for severe CAP, n (%) | ||||||
| Septic shock | 45 (12) | 57 (37) | <0.001 | – | – | – |
| Invasive mechanical ventilation | 0 (0) | 70 (45) | <0.001 | – | – | – |
| ≥1 major criteria | 45 (12) | 97 (63) | <0.001 | – | – | – |
| Minor severity criteria for severe CAP, n (%) | ||||||
| Hypotension requiring aggressive fluid resuscitation | 43 (12) | 25 (17) | 0.109 | 9 (1) | 0 (0) | >0.999 |
| Respiratory rate≥30breaths/min | 206 (61) | 81 (59) | 0.740 | 207 (15) | 15 (34) | 0.001 |
| PaO2/FiO2≤250 | 209 (68) | 100 (71) | 0.486 | 221 (20) | 17 (35) | 0.011 |
| Temperature<36°C | 51 (14) | 16 (11) | 0.396 | 42 (3) | 2 (4) | 0.396 |
| White blood cell count<4000cells/mm3 | 46 (13) | 20 (13) | 0.913 | 47 (3) | 0 (0) | 0.403 |
| Platelet count<100,000 platelets/mm3 | 12 (5) | 6 (6) | 0.734 | 8 (1) | 1 (2) | 0.344 |
| Uremia (creatinine level>1.5mg/dL or BUN 20mg/dl or greater) | 226 (62) | 91 (60) | 0.663 | 274 (19) | 9 (18) | >0.999 |
| Multilobar involvement | 187 (51) | 76 (49) | 0.695 | 185 (13) | 14 (28) | 0.002 |
| Mental confusion | 197 (54) | 67 (44) | 0.038 | 160 (11) | 5 (10) | 0.794 |
| ≥3 minor criteria | 347 (95) | 114 (74) | <0.001 | – | – | – |
| Only ≥3 minor criteria | 320 (88) | 57 (37) | <0.001 | – | – | – |
Abbreviations: BUN indicates blood urea nitrogen; CAP, community-acquired pneumonia; FiO2, fraction of inspired oxygen; ICU, intensive care unit; PaO2, partial pressure of arterial oxygen; PSI, pneumonia severity index; Q1, first quartile; Q3, third quartile. Percentages calculated on non-missing data. p-Values marked in bold indicate numbers that are statistically significant within the 95% confidence limit.
The definition of severe CAP in the 2007 IDSA/ATS guidelines is moderately accurate for predicting both ICU admission and mortality in patients aged 80 years and older, with 25% of the patients with severe CAP criteria (mainly based on the presence ≥3 minor criteria) being admitted to the ICU.
Integrating certain key characteristics of VEP patients (e.g., frailty, malnutrition, multiple comorbidities, polypharmacy, etc.) in their enhance the clinical decision-making process, in particular regarding certain life-support treatments such as the use of IMV.18 In addition, ICU admission in VEP with CAP might largely vary due to local hospital practices. In our study, 10% of VEP with CAP required ICU admission, which is in line with prior studies.19,20 Developing tools that support decision-making processes beyond the “crude age” is necessary.
Some of the variables independently associated to a higher likelihood of ICU admission in our cohort largely overlap with IDSA/ATS criteria for severe CAP. Others, such as male sex and hyperglycemia are frequently associated with ICU admission both in the general population and VEP, while pleural effusion makes part of the “Risk of Early Admission to ICU” (REA-ICU) score.21,22 Patients with a chronic neurological disease, which is a frequent cause of disability in VEP, often face exclusion from ICU admission.
In our cohort, the IDSA/ATS criteria for severe CAP moderately predicted ICU admission (75% sensitivity, 80% specificity). In a meta-analysis, the same criteria had a pooled sensitivity of 84% and a specificity of 78% for predicting ICU admission in the general adult population.23 The presence of major criteria, particularly receiving invasive mechanical ventilation, was a main determinant in deciding whether ICU admission. It is worth mentioning that in spite that our study is not the first at attempting to assess the prediction ability of IDSA/ATS criteria with regards to the likelihood of ICU admission, there is an inherent flaw in this approach, namely that receiving invasive mechanical ventilation as one of the major criteria is per se associated with ICU admission. Hence the potential usefulness of minor criteria over major criteria in certain populations. In the case of VEP, patients are less likely to receive endotracheal intubation and mechanical ventilation than younger patients. Moreover, not all patients that receive invasive mechanical ventilation are admitted to the ICU. Patients can be intubated by the emergence services outside the hospital or early after they arrive to the emergence room and only require invasive mechanical ventilation during a short period before they are either admitted to the ICU or even the ward. In any case, whereas in the first IDSA/ATS criteria validation study conducted by Liapikou et al.7 authors concluded that the need for ICU admission derived from minor severity criteria alone was uncertain, our study suggest that it might be the opposite in the case of VEP.
Most patients with severe CAP treated outside of the ICU had ≥3 minor severity criteria in the absence of major criteria, and they did not therefore, require active life support measures. Thus, using the IDSA/ATS minor criteria to identify severe CAP early for aggressive emergency department resuscitation resulted in lower hospital mortality and ICU admission rates, as well as less inappropriately delayed ICU admissions.24 Once these VEP patients with minor severity criteria have been stabilized in the emergency room, our results do not support that further admission to the ICU would have resulted in reduced mortality.
Available evidence shows that well-selected VEP with CAP admitted to the ICU present better outcomes than those who are not.25,26 In our cohort, patients with severe CAP not admitted to an ICU were older than those admitted to an ICU, with a similar PSI score (which includes age, comorbidities and acute severity of pneumonia). In a multicenter study by Andersen et al., 29.6% of VEP were denied ICU admission.25 Our findings suggest that chronological age, as patients with DNR were excluded, play a relevant in the decision to assign some of these patients with severe CAP to the ward rather than ICU. With available data, it seems advisable to use the IDSA/ATS criteria as an aid to clinical judgment that can be further complemented with other biomarkers and the patients baseline quality of life until more evidence is gathered in VEP.27,28
The prediction of severe CAP criteria for 30-day mortality was similar to that for ICU admission in our VEP.
The strengths of this study include the prospective design, large sample size, participation of three hospitals, and comprehensive data collection over an extended time period, which also might pose a limitation due to potential historical bias. However, our work has several limitations. First, we did not record data on baseline quality of life, frailty, and/or functional status, which might have had an impact on clinical decisions regarding ICU admission. Second, relevant variables concerning the management of septic shock were not collected, e.g., dosage and duration of vasopressors. Third, it should be reminded that the IDSA/ATS criteria for indicating direct ICU admission in cases of severe CAP entailed admission to the ICU within 24h from hospitalization, and therefore our study does not provide data on the ability of IDSA/ATS criteria to predict ICU admission at a later phase during hospital admission. Fourth, blood urea nitrogen (BUN) level was not systematically determined in our population; therefore, we used serum creatinine level as a surrogate, as we have done in previous studies.7,29 Fifth, we used the physicians’ decision for ICU admission as the gold standard, as this reflected actual clinical practice. However, the variability of clinicians’ judgment and the frequent constraints on the availability of ICU beds may have influenced site-of-care decisions. Finally, serum lactate, which is currently part of the definition of septic shock, was not systematically registered until recent years.
ConclusionThe IDSA/ATS criteria for severe CAP predict ICU admission in VEP moderately well. While our results indicate that patients with invasive mechanical ventilation and those with septic shock should be allocated to the ICU even when they have been stabilized previously, severe CAP not fulfilling either of those major severity criteria might be managed acceptably in wards.
Availability of dataThe datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
FundingThis study was supported by CIBER de Enfermedades Respiratorias (CIBERES CB06/06/0028), and by 2009 Support to Research Groups of Catalonia 911, IDIBAPS. The founders of the study had no role in the study design, data collection, analysis, or interpretation, writing of the report, or decision to submit for publication. CC received a grant from the Fondo de Investigación Sanitaria (PI19/00207), Instituto de Salud Carlos III, co-funded by the European Union.
Conflict of interestsThe authors declare that they have no competing interest.
We are indebted to all participating medical and nursing colleagues for their assistance and cooperation in this study.