Pulmonary infiltrates are common within the hematopoietic stem cell transplant (HSCT) population and unfortunately portend an increased mortality. Bronchoscopy is often utilized as an initial diagnostic tool, but the literature supporting its diagnostic utility and effect on clinical management varies significantly. The aim of this study was to investigate the diagnostic ability, complication rate, and clinical impact of flexible bronchoscopy (FB) in evaluating pulmonary infiltrates in a large HSCT population.
Patients and methodRetrospective review of all patients undergoing FB after HSCT in the Bone Marrow Transplant Unit from 1996 to 2009.
ResultsFB was performed 162 times in 144 patients with pulmonary infiltrates yielding positive results in 52.5%. The most common positive results were bacterial pneumonia (31%), fungal pneumonia (15%), and alveolar hemorrhage (11%). Treatment changes occurred in 44% of patients after FB. Treatment changes included antibiotic modification (59%), addition of corticosteroids (21%), antifungal modification (12%), and antiviral modification (7%). The overall complication rate associated with FB was 30%, although 84% of these complications were considered minor.
ConclusionsFB in patients with pulmonary infiltrates after HSCT should still be considered a valuable tool in the evaluation and management of pulmonary infiltrates in the HSCT population. Future prospective, multicenter randomized studies are needed to evaluate the overall clinical impact that bronchoscopic results and management changes have in this unique population.
Los infiltrados pulmonares son frecuentes en la población con trasplante de células madre hemopoyéticas (TCMH) y, lamentablemente, comportan un aumento de la mortalidad. La broncoscopia se emplea con frecuencia como método diagnóstico inicial, pero la literatura que respalda su utilidad diagnóstica y su efecto sobre el tratamiento clínico presenta discrepancias significativas. El objetivo de este estudio fue investigar la capacidad diagnóstica de la broncoscopia flexible (BF) en la evaluación de los infiltrados pulmonares en una población amplia de pacientes con TCMH.
Pacientes y métodosRevisión retrospectiva de todos los pacientes a los que se practicó una BF después de un TCMH en la unidad de trasplantes de médula ósea entre 1996 y 2009.
ResultadosSe llevó a cabo una BF en 162 ocasiones en 144 pacientes con infiltrados pulmonares y se obtuvieron resultados positivos en el 52,5% de los casos. Los resultados positivos más frecuentes fueron la neumonía bacteriana (31%), la neumonía fúngica (15%) y la hemorragia alveolar (11%). Tras la BF se introdujeron modificaciones en el tratamiento del 44% de los pacientes. Los cambios del tratamiento consistieron en una modificación de la medicación antibiótica (59%), adición de corticosteroides (21%), modificación de la medicación antifúngica (12%) y modificación de la medicación antiviral (7%). La tasa global de complicaciones asociadas a la BF fue del 30%, si bien el 84% de estas complicaciones se consideraron de carácter menor.
ConclusionesLa BF en los pacientes que presentan infiltrados pulmonares después de un TCMH debe continuar considerándose un instrumento útil en la evaluación y el tratamiento de los infiltrados pulmonares en la población tratada con TCMH. Serán necesarios nuevos estudios prospectivos, multicéntricos y aleatorizados para evaluar las repercusiones clínicas globales que tienen los resultados de la broncoscopia y las modificaciones del tratamiento en esta población específica.
Hematopoietic stem cell transplantation (HSCT) was first introduced as a therapeutic modality applicable in oncology clinical practice in the late 1960s, and since then has been used to treat neoplastic and non-neoplastic disorders. Recent data from the National Bone Marrow Transplant Data Registry have documented more than 60,000 transplants since its creation in 1986. Unfortunately, pulmonary complications are often observed in this patient population, which contributes significantly to post-transplant morbidity and mortality.1–3 These complications include those of infectious etiology, such as infections caused by bacterial, viral and fungal pathogens, and those due to non-infectious causes, such as graft-versus-host disease (GVHD), diffuse alveolar hemorrhage, obliterating bronchiolitis, interstitial pneumonitis and pulmonary edema. Pulmonary infiltrates in the HSCT population constitute a difficult therapeutic dilemma. Some experts recommend the use of flexible bronchoscopy (FB) in HSCT patients in whom new infiltrates or worsening of existing infiltrates has been observed,4,5 while others have recommended more empirical treatment with broad-spectrum antimicrobial agents in patients with more localized infiltrates.6,7 An initial approach with broad-spectrum antimicrobials and dieresis has also been proposed, reserving more advanced diagnostic examinations for patients who do not respond, or in whom there are still concerns. There are no hard data which suggest that a certain approach is more effective.
Previous studies have examined the use of FB in the HSCT population with the main diagnostic methods such as bronchoalveolar lavage (BAL), protected specimen brush (PSB) and/or transbronchial biopsy (TBB).8–13 However, most of these studies have various limitations, such as small sample size, the inclusion of other non-transplant patient populations, lack of identification of treatment changes introduced as a consequence of the FB results, and the yield provided by FB in the period prior to the use of prophylaxis.
The aim of our study was to retrospectively evaluate the experience in our center with the use of FB in evaluating pulmonary infiltrates in an adult HSCT population. We planned to evaluate the diagnostic yield of FB, its impact on clinical treatment decisions in hospitalized adult HSCT patients and its complication rate.
Patients and MethodsThomas Jefferson University Hospital is a 957-bed tertiary care center, with a 14-bed bone marrow transplant unit (BMTU). Admissions to the BMTU correspond to newly diagnosed hematological malignancy patients, patients undergoing HSCT, or HSCT patients who require hospitalization due to transplant-related complications. All patients admitted to the BMTU in whom FB was performed after a HSCT between 1 January 1996 and 31 December 2009 were identified from hospital discharge codes, through the medical record department. Data were obtained retrospectively by reviewing the medical records and bronchoscopy reports of all patients. In patients who underwent more than one FB, each examination was considered independently. This study was approved by the Thomas Jefferson internal ethical review board.
All patients in the BMTU were admitted under a medical oncologist with a particular interest in bone marrow transplant. The decision to request a respiratory medicine consultation and the time of doing so was at the discretion of the medical oncologist responsible for the patient's care, as in our center there is no standard protocol for evaluating HSCT patients who present pulmonary complications.
Patient Population and Demographic CharacteristicsWe obtained demographic data, including age, sex, indication for HSCT and type of HSCT performed (allogeneic compared to autologous). We recorded time variables, such as the time between the transplant and obtaining radiological images, the bronchoscopic evaluation, and the time between mechanical ventilation and the bronchoscopic evaluation.
Laboratory Data and Chest X-rayThe laboratory data from the day of the FB included analytical values such as the total white cell count, hemoglobin, platelet count, prothrombin time, international normalized ratio (INR) and partial thromboplastin time. Radiological examinations (chest X-ray or chest computed tomography scans) carried out preoperatively were also obtained. The pulmonary infiltrates were analyzed from the final radiological report, which indicated absence of infiltrates, presence of focal infiltrates (which affected one or two lobes) or presence of diffuse infiltrates (which affected more than two lobes).
Diagnostic InterventionA respiratory consultation was carried out in all patients analyzed in our study. The decision to perform a FB, as well as the choice of method for obtaining diagnostic samples, was at the discretion of the pulmonologist in charge of the case. There are no strict indications or contraindications for performing FB in the HSCT population in our hospital. However, general indications for FB often include new infiltrates in which possible infection is a concern, alveolar hemorrhage or unknown etiology of new-onset respiratory failure. Relative contraindications include the presence of significant coagulopathy (INR>2), thrombocytopenia (platelet count <50000), hemodynamic instability or uncorrectable hypoxemia. The decision to apply a specific method to obtain diagnostic samples (BAL, PSB and/or TBB) was taken by the pulmonologist performing the FB.
Bronchoscopic ResultsThe samples obtained were confirmed with the surgical report and the results were based on the final microbiology, cytology and histopathology reports from the electronic medical record. The BAL samples were sent for bacterial culture, fungal culture, viral culture and mycobacterial smear and culture, together with cytological analysis (with evaluation of the presence of malignant disease and Papanicolaou and modified Wright–Giemsa tests for the detection of Pneumocystis, fungal and viral effects). Alveolar hemorrhage was defined by BAL samples with increasingly bloody return (three separate samples were required) or by the presence of 20% or more hemosiderin-laden macrophages, as defined by Afessa et al.14 Histopathological diagnosis of the transbronchial biopsy samples was obtained from the final histopathology reports. If open lung biopsy or autopsy reports were available, they were also analyzed to determine the pulmonary pathology, and were defined as pulmonary biopsies. These results were not included in the analysis of the diagnostic yield or treatment modifications.
ComplicationsInformation on the complications of the FB was obtained from the surgical reports together with a review of the patient's medical record to identify complications that appeared in the twenty-four hours following the bronchoscopy. Minor complications were defined as follows: hypoxemia requiring an increase in oxygen therapy administered by nasal cannulae, mild or moderate hemorrhage (not requiring intervention), hypotension not requiring vasopressor support or unable to complete the FB. Major complications were defined as follows: hypoxemia requiring additional oxygen therapy using a high flow mask, need for mechanical ventilation (non-invasive or invasive), arrhythmia requiring intravenous medication, hypotension requiring vasopressor support, severe hemorrhage requiring intervention, or death.
Outcome VariablesPatients’ hospital medical records were also examined to determine if their treatment had been modified in the 72h following the FB. Treatment modification was defined as addition, discontinuation or change of antimicrobial treatment, or the addition of systemic corticosteroids. Mortality was defined as death in hospital occurring at any time. Mortality was recorded from the date of transplant and bronchoscopy.
Statistical AnalysisDescriptive statistics were used for presentation of the FB results in our population. Mean, median and standard deviation were calculated using Microsoft Excel. The Mann–Whitney test was applied to compare continuous variables between groups. χ2 analysis was used to compare the groups with respect to the discrete variables. A P value less than .05 was considered statistically significant.
ResultsDemographic Characteristics of the Patients, Laboratory Data, Radiographic DataBetween January 1996 and December 2009, a total of 660 patients were treated with HSCT in the Thomas Jefferson University Hospital BMTU. Of these, 144 patients underwent 162 FB, obtaining diagnostic samples. The demographic characteristics of the patients at the time of the FB are summarized in Table 1.
Demographic Characteristics at the Time of the FB.
| All FB examinations (n=162) | |
| Mean age in years | 48.5 (13.5) |
| Sex | |
| Female | 68 (42%) |
| Male | 94 (58%) |
| Indication for transplant | |
| Leukemia | 100 (62%) |
| Lymphoma | 27 (17%) |
| Multiple myeloma | 18 (11%) |
| Others | 17 (10%) |
| Type of transplant | |
| Allogeneic | 137 (85%) |
| Autologous | 25 (15%) |
Mean age in years, with standard deviation in parentheses. Data on sex, indication for transplant and type of transplant are presented using the number of patients with percentage of patients in parentheses.
The 162 FB were carried out to evaluate pulmonary infiltrates identified on the computed tomography scan or chest X-ray. Chest X-ray was used in 40 patients; 30 (75%) had diffuse infiltrates. Chest CT scan was used in 122 patients; 95 (78%) had diffuse infiltrates. Fifty-three (33%) examinations were carried out on patients on mechanical ventilation due to respiratory failure. The time between the HSCT and radiographic evaluation of the pulmonary infiltrates was a median of 44 days, with a mean of 177.2 days and a range of 0–2606 days. The time from the radiographic evaluation until the FB was a median of 2 days, with a mean of 3.1 days and a range of 0–16 days.
As a standard method (unless contraindicated) all HSCT patients received antimicrobial prophylaxis with trimethoprim/sulfamethozaxole, voriconazole and acyclovir. After being discharged home, the prophylactic medication regimen was individualized by the patient's outpatient oncologist. In the total of 162 bronchoscopies, 161 (99%) patients were being treated with empirical broad spectrum antibiotics, 156 (96%) were performed when the patient was receiving antifungal medication, 158 (97%) when antivirals were administered and 145 (89%) when they were being treated with anti-Pneumocystis medication.
Bronchoscopy ResultsDiagnostic samples were obtained from a total of 162 flexible bronchoscopies. All examinations were carried out in the BMTU, at the patient's bedside or in the endoscopy room. In all patients in whom active mechanical ventilation was being used at the time of the examination, it was carried out in the BMTU; sedation was used when it was required for mechanical ventilation. This normally involves the use of propofol, midazolam and/or fentanyl in infusion. Neither paralyzing drugs nor general anesthesia were used in any of the patients for the examination, and in all cases an endotracheal tube was maintained, since it was needed for mechanical ventilation. All other examinations were carried out in the endoscopy room using moderate sedation. Topical lidocaine was used, followed by intravenous administration of fentanyl and midazolam, without an artificial airway.
The following techniques were applied during the FB: BAL, 145; PSB, 41 and TBB, 22. A positive result was identified in 85 FB examinations performed, which is a diagnostic yield of 52.5%. The breakdown of these techniques found 145 BAL with a yield of 53.1% positive results, 41 PSB with a yield of 22% positive results and 22 TBB with a yield of 81.8% positive results (Table 2). In the 22 TBB performed, a mean of 3.43 biopsies were attempted, with a range from 1 to 7.
Among the positive results (Table 3), a positive microbiological result was the most common observation (84 cases identified), followed by diffuse alveolar hemorrhage (18 cases identified). Bacterial pathogens were identified in 53 cases, viral in 4 cases, fungal in 25 and Mycobacterium avium complex in 2. No cases of Pneumocystis carinii pneumonia were diagnosed. No evidence of malignant disease was found. Candida spp. was the pathogen most frequently identified, followed by Streptococcus.
Microbiological Results in the Total of 85 Positive FB.
| Number | |
| Bacteria | |
| Streptococcus spp. | 13 |
| Staphylococcus spp. | 9 |
| Enterococci | 9 |
| Pseudomonas spp. | 7 |
| Escherichia coli | 4 |
| Lactobacillus | 2 |
| Bacteroides | 2 |
| Serratia | 1 |
| Enterobacter | 1 |
| Klebsiella | 1 |
| Proteus | 1 |
| Xanthomonas | 1 |
| Total | 51 |
| Fungi | |
| Candida spp. | 16 |
| Aspergillus | 5 |
| Saccharomyces | 2 |
| Yeast (unspecified) | 2 |
| Total | 25 |
| Virus | |
| CMV | 3 |
| Influenza | 1 |
| Total | 4 |
| Mycobacteria | |
| Mycobacterium avium-intracellular | 2 |
| Others | |
| Alveolar hemorrhage | 18 |
The TBB results are shown in Table 4. Signs of infectious pneumonia were observed in only one biopsy.
Bronchoscopy ComplicationsThe overall rate of complications associated with FB in the 24h following the intervention was 30% (49/162). Of these complications, 5% (8/162) were considered major and consisted of hypoxemia requiring additional oxygen therapy using a mask or need for mechanical ventilation (n=4), arrhythmia (n=1), hypotension requiring vasopressor support (n=1), severe hemorrhage (n=1) and death (n=1). There were 41 minor complications consisting of hypoxemia requiring additional oxygen therapy using nasal cannulae (n=25), mild to moderate hemorrhage (n=7), bronchospasm (n=5), hypotension not requiring vasopressor support (n=3) and aspiration (n=1). In total, mild hypoxemia accounted for 51% of all complications. There were no significant differences in the coagulation parameters between patients with FB complications and those who did not have complications after the use of FB (Table 5). In all of the patients in whom TBB was carried out, there were no cases of pneumothorax (0/22) on the chest X-rays obtained systematically after the examination.
Twenty patients had video-assisted thoracoscopic surgery (VATS) or an open lung biopsy after the FB. Four patients had an open lung biopsy after the FB with transbronchial biopsy. The results obtained on comparing the open lung biopsy with the TBB were as follows: non-diagnostic in 2 patients, coincidental diagnosis in one patient, and diagnostic discrepancy in one patient. Of the patients who underwent VATS, 11 died and 9 survived.
Clinical Results After the BronchoscopyTreatment changes and the types of change that occurred are shown in Table 6. We observed the introduction of treatment changes after 72 bronchoscopies (44.4%). This included 45 bronchoscopies with at least one positive result and 27 bronchoscopies with a non-diagnostic result. Treatment changes consisted of modification in the antibiotic medication (n=43), modification in the antifungal medication (n=9), modification in the antiviral medication (n=5) and addition of corticosteroids (n=15).
Treatment Changes Introduced After 162 Fibrobronchoscopies.
| Treatment change | Number |
| Modification of the antibiotic medication | 43 |
| Addition | 8 |
| Withdrawal | 35 |
| Modification of the antifungal medication | 9 |
| Addition | 8 |
| Withdrawal | 1 |
| Modification of the antiviral modification | 5 |
| Addition | 4 |
| Withdrawal | 1 |
| Modification of corticoids | 15 |
| Addition | 15 |
| Withdrawal | 0 |
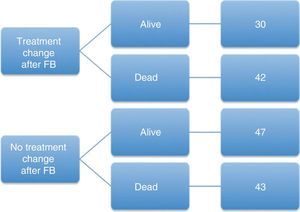
We examined the survival during hospitalization in patients in whom FB was carried out and treatment administered. There were no statistically significant differences in survival in patients in whom treatment was changed after the FB compared with those in whom no therapeutic modification had been introduced (Fig. 1). Overall, there were no differences in mortality in patients grouped according to the type of transplant, autologous compared to allogeneic (P=.617).
Results in Allogeneic Compared to Autologous Hematopoietic Stem Cell TransplantA total of 137 bronchoscopies were carried out in patients with allogeneic HSCT and 25 were performed in patients with autologous HSCT. In the autologous transplant population, no treatment changes were introduced after the bronchoscopy in ten patients, with a survival of 50% (5/10). There were treatment changes after the bronchoscopy in 15 patients, with a survival of 60% (9/15). In the allogeneic transplant population, there were no treatment changes after the bronchoscopy in 80 patients, with a survival of 52.5% (42/80). Treatment was modified after the bronchoscopy in 57 patients, with a survival of 63.2% (36/57).
DiscussionFB remains an attractive technique for most clinicians, given its diagnostic ability and ease of use in patients in a critical condition.4–6 Over a period of 14 years in our hospital, 144 of 660 HSCT patients (22%) underwent FB to evaluate pulmonary infiltrates; most were being treated with broad spectrum antimicrobials at the time of the FB. The overall diagnostic yield in our cohort was 52.5%; treatment changes were introduced after the FB in 44% of patients. We believe that these data continue to support the use of FB in the evaluation of pulmonary infiltrates in the HSCT population.
The positive diagnostic yield of FB in the HSCT population was a primary outcome variable in our study. The overall diagnostic yield of FB in our population was 52.5%. BAL was positive in 53.1% of cases and TBB was positive in 81.8% of cases in which it was performed. Most of the results obtained in the BAL corresponded to infectious microorganisms, especially streptococci and candida species; however, alveolar hemorrhage was also observed in 21.1% of positive BALs.
These results agree with those of previous studies, in which the diagnostic ability of FB after transplant was investigated. In the literature, a positive diagnostic yield was observed in 31%–74% of FB.8–13,1 However, as previously indicated, many of the studies had the limitation of small sample size, inclusion of patients without HSCT and the exclusion of prophylactic antimicrobial medication guidelines. The most extensive study conducted in HSCT patients appears to be the study published recently by Shannon et al. from data obtained in the period 1994–1999, in which they attempted to determine the impact of early versus late referrals for bronchoscopy. These authors retrospectively evaluated a total of 598 bronchoscopies with BAL performed in patients treated recently with HSCT, in whom an evaluation was carried out for the presence of pulmonary infiltrates. The overall yield of the technique was 55%, but the authors indicated a 2.5-fold increase in the diagnostic yield when the examinations were performed within 4 days of hospitalization. However, this increased diagnostic yield did not significantly modify the clinical treatment, since there do not seem to have been differences between the population with early use and the population with late use.15
Kasow et al. published a similar study that was more extensive in terms of size and duration, in which they examined a pediatric HSCT population at St. Jude Children's Research Hospital. These authors examined 89 patients over a period of 12 years. Their conclusion was that, in the pediatric population, the use of active immunosuppression or the presence of grade II-IV graft-versus-host disease reduced the probability of obtaining a positive BAL. The clinical impact of the BAL results was not examined, except for the finding that 16 of their patients had an open lung biopsy; however, 14 of these had a positive BAL, which could reduce the need for open lung biopsies.16
A second objective of our study was to assess treatment changes after the FB, defined as the addition or withdrawal of antimicrobial drugs or corticosteroids. Modifications were introduced in the clinical treatment in 44% of our population after the FB; thus we could consider that this is a significant clinical intervention. The changes most frequently identified were the modification of antibiotic treatment guidelines. It is interesting to note that the bronchoscopy provided a result in 52.5% of the examinations, and that treatment changes were made in a further 27 patients, even though the FB result was not diagnostic. It could be argued therefore, that the FB was thus “diagnostic” on discarding significant pulmonary disease and enabling the patient's clinician to possibly “de-escalate” the treatment.
A third objective of our study was to evaluate the complication rate of FB in the HSCT population. FB is considered a safe technique, with complication rates varying between 0.3% and 6% in the general population.17,18 However, in the HSCT population, the complication rates previously described vary between 0 and 41%.19 Our overall complication rate was 30%, with major complications occurring in only 5%, including one death. It is interesting to note that there were no significant differences in the coagulation parameters between patients who had complications after the FB and those who did not. It is of utmost importance that the vast majority of complications consisted of mild hypoxia, which seemed to have little clinical significance.
In view of existing data, many authors recommend the use of FB as the initial diagnostic method of choice in HSCT patients with pulmonary infiltrates. Others also recommend a second FB (possibly with the addition of TBB to the diagnostic arsenal) in the context of an initial non-diagnostic FB.6 However, the need to obtain new diagnostic samples, such as TBB or open lung biopsy samples, remains controversial. We have shown a fairly high diagnostic yield for TBB in our HSCT population, but most of these diagnoses remained non-specific. The real clinical impact of a diagnosis such as non-specific interstitial pneumonitis remains unknown. This diagnosis does not provide the clinician with any information about the specific underlying etiology and process, but it may still provide useful information for treating the patient. An important limitation of our TBB data is the small sample size and the introduction of a sampling bias.
The limitations of our study are multifactorial. Firstly, this is a retrospective study conducted in a single center, which may not be generalizable to all centers. The most important limitation in this respect may be in the clinical practice bias that exists in our hospital for evaluating HSCT patients. Since there is no specific protocol for evaluating HSCT patients, the decision to perform a bronchoscopy, when to do so and the decision to apply certain techniques, including BAL, TBB, PSB, etc. when performing the bronchoscopy are factors that may introduce bias. We believe that the high patient number, as well as the time frame of the present study could be useful for reducing the effect that one or two health professionals and their personal bias could have on the overall study results. It is interesting to note that, over fourteen years, there have been very few identifiable changes in the diagnostic yield obtained in these patients. However, there was a notable reduction in the use of protected specimen brush and transbronchial biopsy. The exact reason is not clear, since there were few major complications in our hospital related with bronchoscopy techniques; however, other changes have appeared in the literature during the study period, which may have influenced the decisions of our professionals when applying certain techniques. Secondly, although we define treatment modifications as those introduced within 3 days after the FB, we do not have any definitive way of ensuring that these changes were a direct consequence of the FB itself, given the retrospective nature of the study. A detailed review of the medical records was carried out, to try to relate the bronchoscopy results with treatment changes, but there may be inaccuracies. Thirdly, radiographic evaluation of the pulmonary infiltrates was not standardized, and could include plain X-rays or computed tomography scans. This may have influenced both the decision to move to a bronchoscopic technique and decision-making during its performance. Finally, as this is a retrospective study, no strong statements can be made regarding the causality with respect to the effect of the FB on the results. These issues may be addressed in a multicenter, randomized trial currently being conducted, in which HSCT patients with new onset infiltrates will be randomly included to early (within 36h) or late FB (within 7 days), in order to determine its effects on the results (ClinicalTrials.gov identifier: NCT00846352).
ConclusionDiagnostic yield and treatment changes following FB in our HSCT population were 53.5% and 44%, respectively. Our overall complication rate was high, 30%, but the rate of major complications was only 5%. The vast majority of complications corresponded to mild hypoxemia, which is an expected complication after FB. Our documented rate of major complications of 5% is very likely acceptable in the context of the significant morbidity and mortality associated with pulmonary complications in the HSCT population. Based on our results and on available data, we will continue to recommend FB as an initial diagnostic technique in HSCT patients with pulmonary infiltrates. Prospective studies will be required to evaluate the effects of these treatment changes on the clinical results.
Funding and Implementation of the ProjectNo funding was available or used for this project. All the work was carried out at the Thomas Jefferson University Hospital.
Conflicts of InterestThe authors do not have any possible conflicts of interest. Dr. Gilbert does not have any conflicts of interest to declare. Dr. Learner does not have any conflicts of interest to declare. Dr. Baram does not have any conflicts of interest to declare. Dr. Awsare does not have any conflicts of interest to declare.
Please cite this article as: Gilbert CR, et al. Utilidad de la broncoscopia flexible en la evaluación de infiltrados pulmonares en la población con trasplante de células madre hemopoyéticas: experiencia de 14 años en un solo centro. Arch Bronconeumol. 2013;49:189–95.