With the aim of improving the diagnostic yield of transbronchial lung biopsy, cryotherapy probes have begun to be used for obtaining lung specimens. Studies evaluating the histological material from endobronchial tumors obtained by cryobiopsy have found that the specimens obtained are larger than those obtained with conventional forceps, and that the quality for histology is better.1,2 From these data, the possibility of using cryoprobes as an alternative to the conventional method in the study of diffuse parenchymal lung disease has been proposed, and the results suggest that the technique improves diagnostic efficacy.3 Similarly, descriptive studies aimed at analyzing the viability and the safety of the technique have been performed and have shown no increase in adverse effects, even in lung transplantation patients.4
In this respect, the authors have analyzed the data from 77 patients with suspected diffuse interstitial disease randomized to undergo transbronchial lung biopsy with cryoprobe (39 patients) or conventional forceps (38 patients). A greater number of patients in the cryobiopsy group presented moderate bleeding compared to the conventional group (56.4% versus 34.2%, P=.068). However, this bleeding was not significant, the patients did not require other medical or surgical interventions, and the time of the procedure was not increased. For classification purposes, any bleeding that required suction and occlusion of the segmental bronchus was considered as moderate.
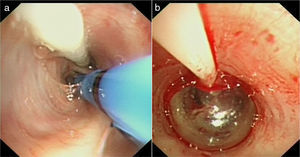
One of the features of this new technique is that, due to the size of the biopsies obtained, the bronchoscope has to be withdrawn with the specimen attached to the tip of the probe; therefore, unlike the conventional method, the endoscopic vision of the bronchial tree is lost for some seconds. Re-introduction of the bronchoscope and occlusion manoeuvres in the segmental bronchus in which the cryobiopsy has been performed may be complicated by the presence of bleeding. In this respect, the aim of using an occlusion balloon is not to reduce the amount of bleeding, but rather to provide better control of bleeding, should it occur. This aspect represents a change in the technique previously described by this group.5
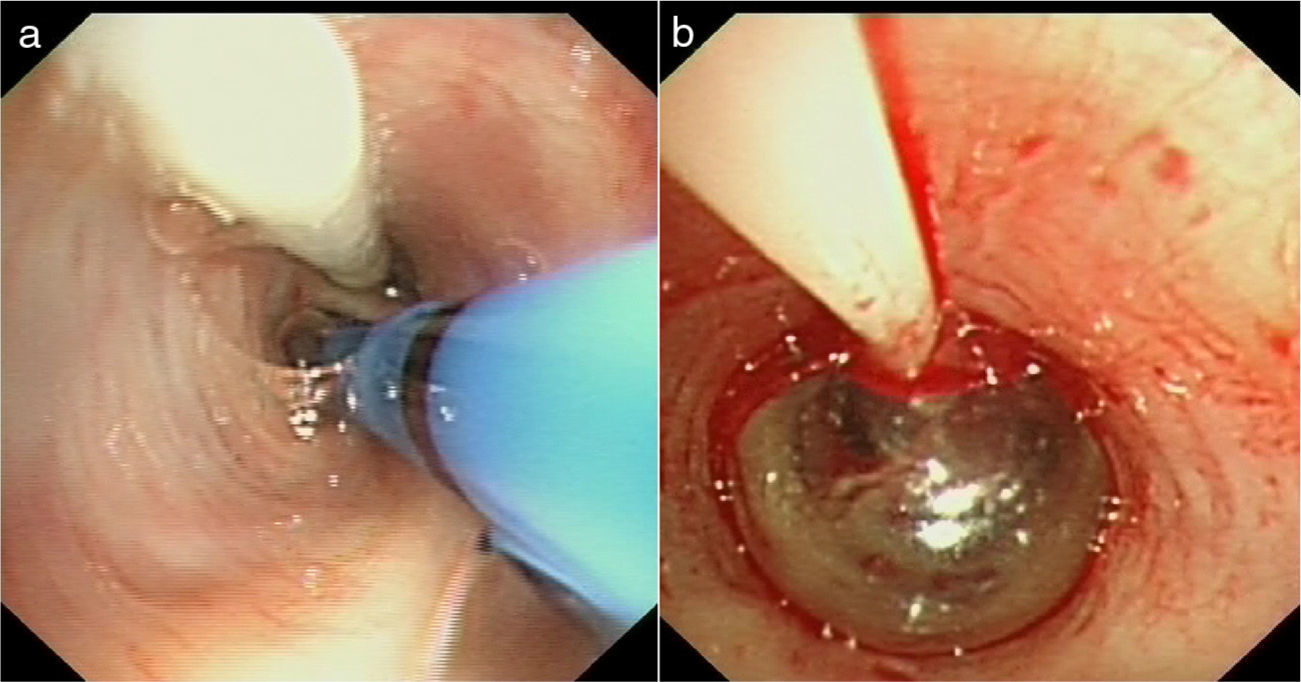
Accordingly, before starting the procedure, an occlusion balloon is introduced (Model B5-2C®, Olympus Medical Systems Corp, Tokyo, Japan) via the side channel of the endotracheal tube (Reference 104100. Broncoflex® 7.5mm, Rüsch, Teleflex Medical, Durham, US) and placed at the entrance to the lung segment from which the transbronchial lung biopsy is to be obtained. Immediately after the specimen is obtained, the occlusion balloon is inflated until absence of bleeding is confirmed on endoscopy.
In conclusion, the preventive use of a hemostatic balloon allows the bleeding to be limited to an occluded area, in the case of hemorrhage. Although this does not directly reduce the intensity of any possible bleeding, it does facilitate endoscopy guiding (Fig. 1).
The authors declare no conflict of interests.
Please cite this article as: Pajares Ruiz V, Torrego Fernández A, Puzo Ardanuy C, Gil de Bernabé A. Utilización de un balón de oclusión en la realización de biopsias pulmonares transbronquiales con criosonda. Arch Bronconeumol. 2014;50:309–310.