88-Year-old man, with a history of prostatic hyperplasia who had abandoned treatment, consulted for dyspnea, dry cough and right pleuritic chest pain in the last 3 days, as well as decreased diuresis. At the initial evaluation he was stable, with blood pressure 133/83, 95bpm, 37°C and SaO2 93%, without breath sounds in the right lung and a suprapubic mass painful on palpation.
Chest X-ray revealed a right unilateral moderate pleural effusion. Blood test showed impaired kidney function and increased acute phase reactants (creatinine: 3.16mg/dL; C-reactive protein: 152mg/L).
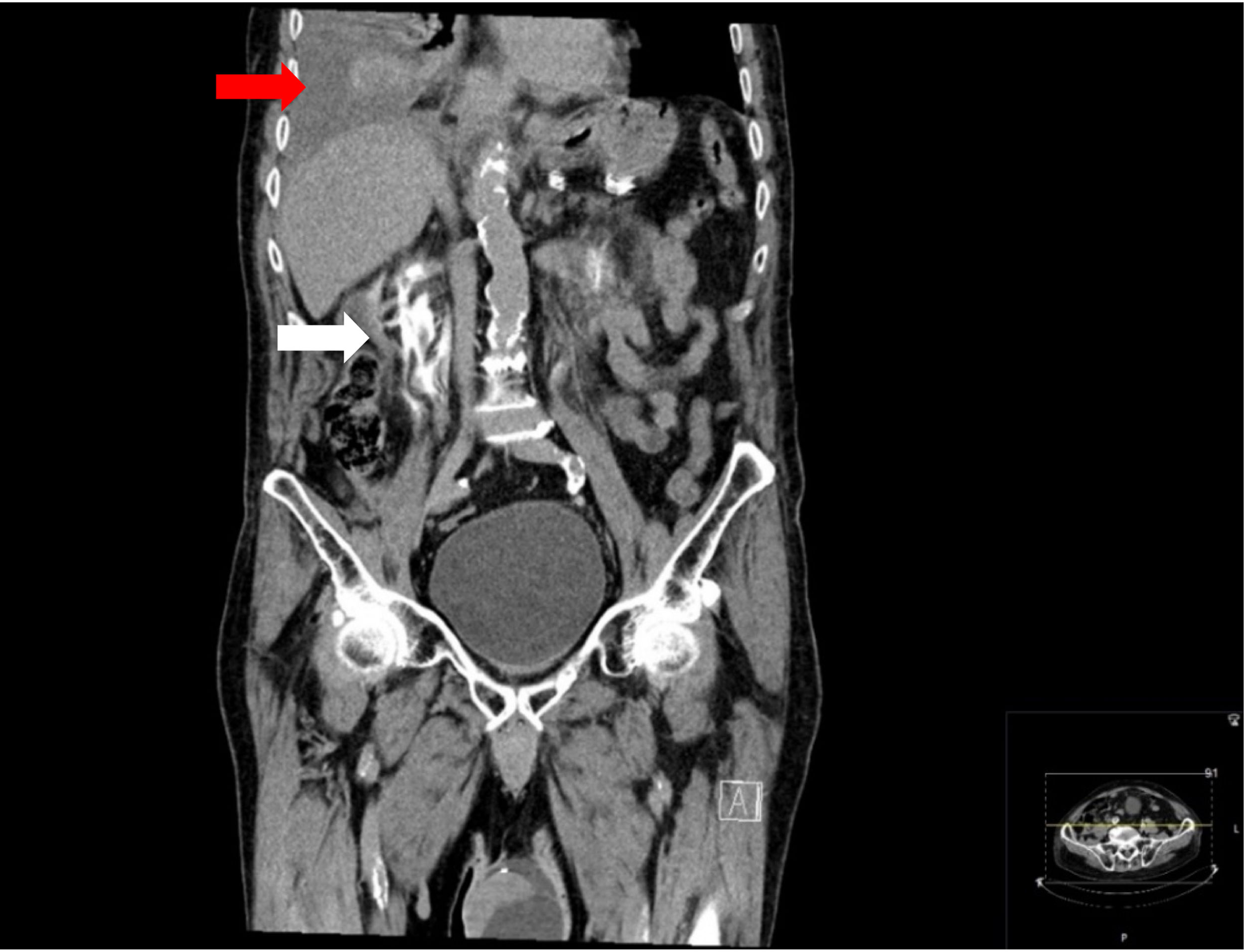
A thoracentesis was performed obtaining a yellowish pleural fluid. Its analysis showed a mononuclear exudate: glucose 149mg/dL; total protein 3.6g/dL; albumin 2.5g/dL; LDH 286IU/L, pH 7.35; pleural fluid/serum protein ratio 0.6; pleural fluid/serum LDH ratio 1.56. A 1500ml chest drain was also performed improving the symptoms, although only partially. CT revealed a still large right pleural effusion with no evidence of underlying pulmonary or diaphragmatic pathology. Likewise, a bladder balloon and a rupture of both ureters with contrast extravasation and formation of urinomas bilaterally, greater on the right, were evidenced, with discreet hyper-uptake of both ureters in relation to urethritis, as well as a notable increase in prostate size (Fig. 1).
Bladder catheterization demonstrated significant urinary retention. A second thoracentesis was performed to extend the analysis after the radiological findings. The pleural fluid obtained showed creatinine 3.17mg/dL, urea 155mg/dL, pleural fluid/serum creatinine ratio >1, confirming urinothorax. Culture and cytology of the pleural fluid were negative. A percutaneous nephrostomy was initially proposed but was not possible since no significant hydronephrosis was identified by ultrasound after bladder catheterization. Conservative management was adopted with favorable evolution. A control CT was performed without evidence of ureteral damage or urinomas, with persistence of minimal pleural effusion. Treatment for prostatic hyperplasia with an alpha-blocker was reinstated and prostatic surgery was proposed to the patient at discharge.
Urinothorax is a rare presentation of pleural effusion, until a 2017 review only 88 cases had been registered.1 Respiratory symptoms are non-specific and depending on the cause, which is usually traumatic or obstructive on the urinary tract, abdominal pain or urinary symptoms may appear.1–3 Among the obstructive causes, prostate pathology is the most frequent, although lithiasis or malignancy have been described.1,2 Other etiologies are surgery and gynecological pathology.2 It is usually ipsilateral to urinary injury1–3 and urine migration toward the pleura is often through lymphatic drainage or diaphragmatic permeability.1–3 The diagnosis is established by a pleural fluid similar to urine with pleural/plasma creatinine ratio >1.1–3 pH use to be <7.40 but in the presence of hematuria or infections may become alkaline.1,2 It is typically a transudate,1–3 but there are cases of exudate4,5 due to high LDH concentrations after cell disruption.1–3 Over time it becomes similar to serum, so early suspicion is necessary to increase diagnostic sensitivity.3 Treatment consists of relieving respiratory symptoms, where chest drainage can be helpful but is often insufficient, and management of the underlying cause.1,2
Conflict of InterestsThe authors state that they have no conflict of interests.