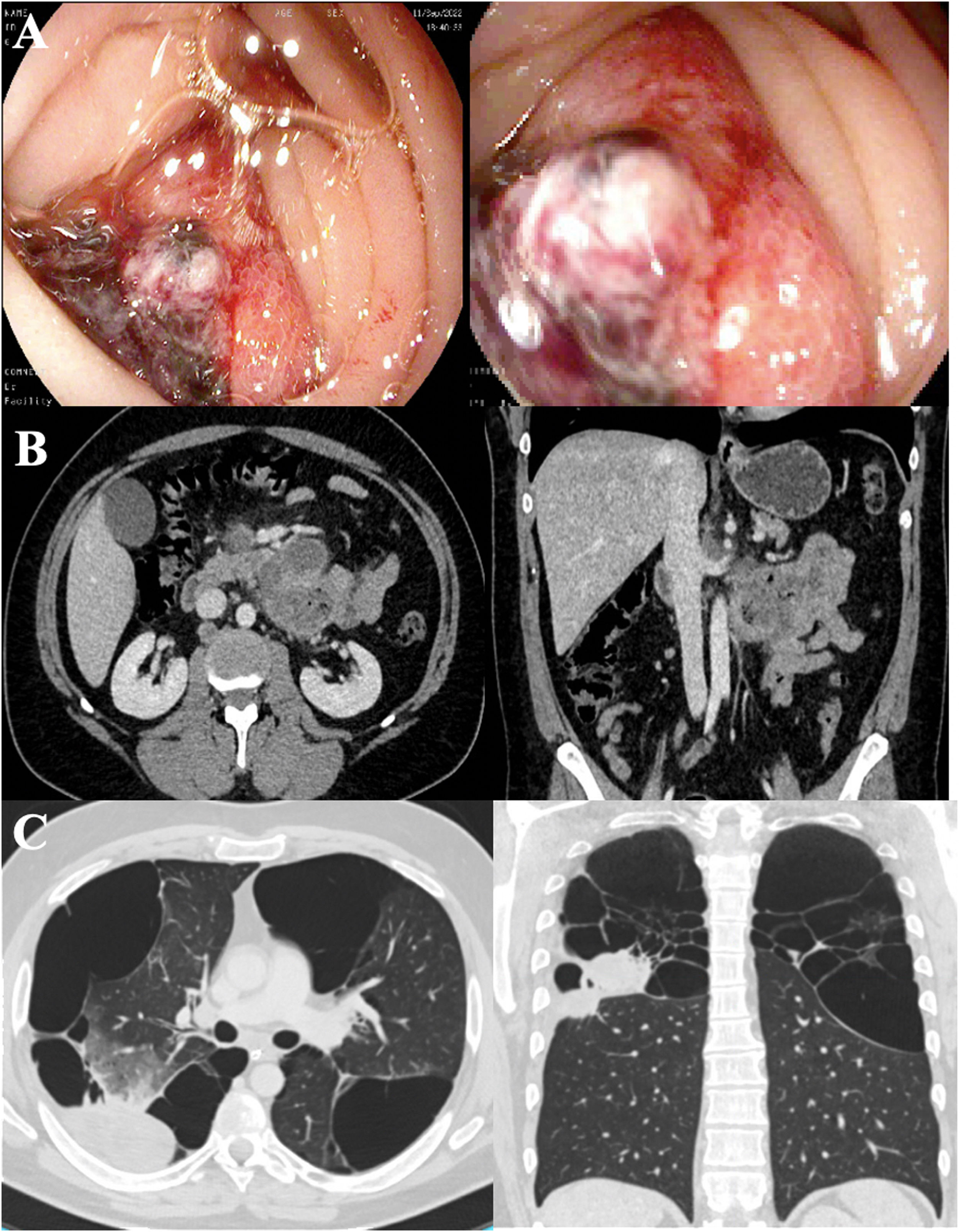
We report the case of a 40-year-old man, COPD GOLD II, with bullous emphysema who was admitted for upper gastrointestinal bleeding (UGIB) and a hemoglobin of 5g/dl. Gastroscopy (Fig. 1A) revealed an actively bleeding ulcer (Forrest IB) in the 3rd segment of the duodenum. An abdominal CT scan was performed (Fig. 1B), showing wall thickening in the regions and adjacent enlarged lymph nodes. Histological and immunohistochemical studies were consistent with high-grade primary pulmonary adenocarcinoma metastases.
(A) Endoscopic image of a large duodenal ulcer with active oozing hemorrhage (Forrest IB). (B) Computed axial tomography image of the abdomen with lesion in the 4th segment of the duodenum with adjacent lymph node blockage. (C) Computed axial tomography image of the chest showing a tumor in the posterior segment of the right upper lung lobe. Extensive bulbous emphysema in upper lobes.
Chest CT scan (Fig. 1C) located the primary pulmonary tumor in the right upper lobe with right hilar and left axillary lymphadenopathies. The histological study of the axillary lymph node was consistent with primary pulmonary adenocarcinoma metastasis strongly positive for PD-L1. The patient was treated with endoscopy and radiotherapy without success, so to achieve hemostasis, a duodenal prosthesis was placed by endoscopy, resulting in progressive recovery and control of gastrointestinal bleeding. Treatment with pembrolizumab then began.
The incidence of gastrointestinal metastasis from lung cancer is less than 2%. It mainly affects the jejunum and ileum, followed by gastric and colonic metastases.1,2 Most are asymptomatic or have non-specific symptoms (abdominal pain, weight loss or anemia) which leads to underdiagnosis, as is evident from the discrepancy between the estimated incidence in clinical studies (0.3%–1.7%) and post-mortem studies (4.7%–14%).1 Obstruction, intestinal perforation, or UGIB are the most common complications.3,4
Duodenal involvement is extremely rare, occurs in advanced stages, and confers poor prognosis. In a search of the literature, Ahmed et al.5 found 16 cases of duodenal involvement published since 1999; incidence was clearly predominant in men, mean age was 59 years, and, in most cases, duodenal involvement developed after the diagnosis of lung carcinoma. The most common subtype was pulmonary adenocarcinoma (40%) and mean survival after diagnosis was 2–4 months.
The peculiarity of this case lies in the form of debut: the diagnosis of lung carcinoma was reached after the onset of UGIB caused by duodenal metastatic involvement, while in most cases, gastrointestinal involvement is a casual diagnosis.
Duodenal metastases pose a diagnostic dilemma: imaging tests (CT and PET-CT) may be useful, but capsule endoscopy appears to be the most viable diagnostic test in the case of small lesions, as it could reduce underdiagnosis. Local treatment, meanwhile, poses a therapeutic dilemma: there is no standardized approach and none of the approaches used appears to have a significant impact on survival. Endoscopic resection of small lesions is safe, although most patients are only candidates for palliative surgery.
In conclusion, duodenal metastasis from lung carcinoma is an unusual entity that is underdiagnosed and has a poor short-term prognosis. A high index of suspicion is necessary, especially in patients with a history of lung cancer and gastrointestinal symptoms or anemia.
Conflict of interestsThe authors state that they have no conflict of interests.