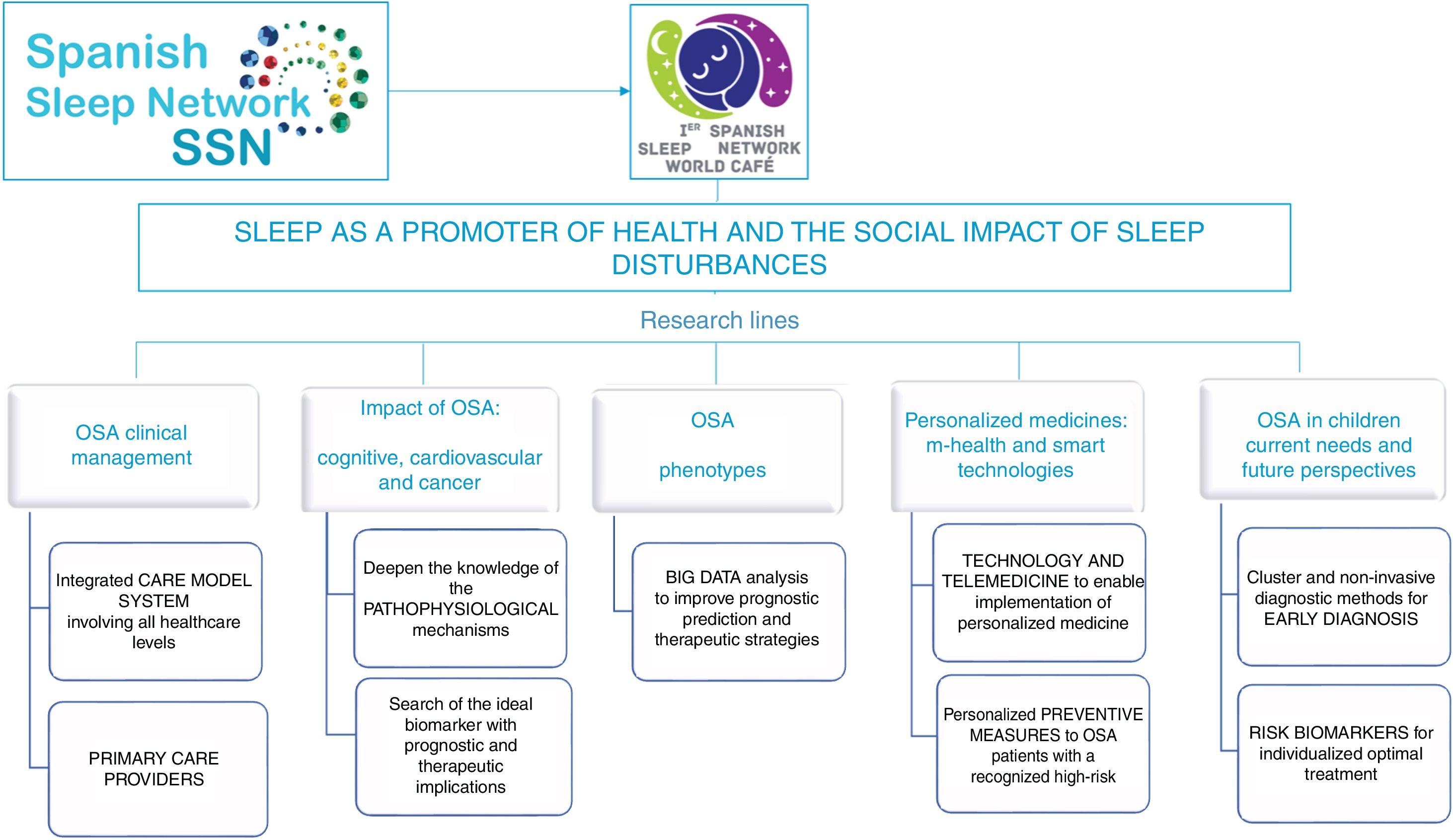
Sleep is considered an essential part of life and plays a vital role in good health and well-being. Equally important as a balanced diet and adequate exercise, quality and quantity of sleep are essential for maintaining good health and quality of life. Sleep-disordered breathing is one of the most prevalent conditions that compromises the quality and duration of sleep, with obstructive sleep apnea (OSA) being the most prevalent disorder among these conditions. OSA is a chronic and highly prevalent disease that is considered to be a true public health problem. OSA has been associated with increased cardiovascular, neurocognitive, metabolic and overall mortality risks, and its management is a challenge facing the health care system. To establish the main future lines of research in sleep respiratory medicine, the Spanish Sleep Network (SSN) promoted the 1st World Cafèc) experts tm) meeting. The overall vision was established by consensus as “Sleep as promoter of health and the social impact of sleep disturbances”. Under this leitmotiv and given that OSA is the most prevalent sleep disorder, five research lines were established to develop a new comprehensive approach for OSA management: (1) an integrated network for the comprehensive management of OSA; (2) the biological impact of OSA on comorbidities with high mortality, namely, cardiovascular and metabolic diseases, neurocognitive diseases and cancer; (3) Big Data Analysis for the identification of OSA phenotypes; (4) personalized medicine in OSA; and (5) OSA in children: current needs and future perspectives.
El sueño se considera una parte esencial de la vida y es vital para una buena salud y para el bienestar. De igual importancia que una dieta equilibrada y una adecuada actividad física, la calidad y la cantidad del sueño son esenciales para mantener una buena salud y calidad de vida. Las alteraciones respiratorias del sueño son los trastornos más prevalentes que comprometen la calidad y duración del sueño, siendo el síndrome de la apnea obstructiva del sueño (SAHS) el más frecuente. El SAHS es una enfermedad de elevada prevalencia que se considera un problema de salud pública. Se ha asociado con aumento del riesgo cardiovascular, neurocognitivo, metabólico y especialmente de mortalidad, y su manejo representa un reto para el sistema de salud. Para establecer las principales líneas futuras de investigación en medicina respiratoria del sueño, el Spanish Sleep Network promovió la primera edición del World Cafe experts tm) meeting. El mensaje principal ¢El sueño como promotor de la salud y el impacto social de los trastornos del sueño¢ se estableció por consenso. Bajo este lema y dado que el SAHS es el trastorno del sueño más prevalente, se establecieron cinco líneas de investigación para desarrollar una aproximación completa para el manejo de este síndrome: 1) Una red integrada para el manejo del SAHS; 2) El impacto biológico del SAHS en las comorbilidades con elevada mortalidad como la enfermedad cardiovascular, las enfermedades metabólicas y neurocognitivas y el cáncer; 3) El análisis de grandes bases de datos para la identificación de fenotipos del SAHS; 4) Medicina personalizada en el SAHS, y 5) El SAHS en niños: necesidades actuales y perspectivas futuras.
Worldwide, obesity, physical inactivity, and poor diet quality are creating an unsustainable burden of chronic disease. Good sleep quality is also essential for maintaining good health and quality of life. Among the sleep disorders (SD), sleep-disordered breathing (SDB) is one of the most prevalent conditions that compromise sleep quality. The predominant condition associated with SDB is obstructive sleep apnea (OSA), which affects at least 10% of the middle-aged population.1•3
The management of OSA is challenging the health care system. Diagnosis and treatment of this condition are expensive and require complex tools that are not available in all areas. This chronic and highly prevalent disease has been associated with increased cardiovascular, neurocognitive, metabolic and overall mortality risks, which have contributed to an increasing interest in new strategies for its management.
The SSN is a multidisciplinary research group that has contributed to the identification of OSA impacts and management over the last 20 years. Its main objective has been to promote research in the field of sleep and was developed based on three fundamental pillars: friendship, generosity, and collaborative work. As a result, this network has generated numerous and outstanding contributions in this area that have been pioneering, especially in the development of some of the leading randomized studies in our field. The aim of the 1st World Cafèc), that occurred in March 2017 in Guadalajara (Spain), was to assemble the talent needed to promote the exchange of knowledge and creation of new ideas with the purpose of establishing the main future investigation lines for sleep respiratory medicine for the next 5 years. This meeting attempted to bring together the main scientific societies associated with sleep disorders in Spain: Sociedad Española de Neumología y Cirugía Torácica (SEPAR), Sociedad Española de Sueño (SES), Centro de Investigaciones Biomèc)dicas en Red (CIBER), Federación Española de Medicina del Sueño (FESMES) and a representation of the most relevant Spanish sleep researchers. To assure generational renewal during this meeting, a group of young researchers assumed the lead of the future actions of the SSN. The overall vision was established by consensus as “Sleep as promoter of health and the social impact of sleep disturbances”. Under this focus and with OSA being the most prevalent SD, five research lines were discussed: (1) to incorporate and involve all levels of care; (2) to explore the biological impact of OSA on diseases with high mortality; (3) to cluster and phenotype OSA; (4) to personalize OSA management using current m-Health and smart technologies; and (5) to study the impact of OSA and specific management of the disease in children.
The purpose of this paper is to document the discussions and conclusions from this important meeting (Fig. 1) for dissemination to the scientific community.
Integrated network for the comprehensive management of OSAIn recent years, there has been an increase in the demand for consultations and diagnostic studies in sleep units, which has resulted in long waiting lists and high costs.4,5 It is unrealistic to assume that adequate management of a chronic and highly prevalent disease such as OSA can be accomplished by sleep specialists alone. There is a need for a new care model for OSA management, namely, an integrated network that involves all healthcare levels. The involvement of primary care in OSA management could be a realistic and viable alternative to the current model6,7 and would improve the implementation of the screening and assessment for OSA.8 To accomplish this goal, adequate training of primary care providers in sleep medicine and the search for strategies that guarantee cost effectiveness should be a priority. Primary care physicians and practice nurses should be involved in the initial stage of the management of OSA patients, and only patients with more complex conditions should be referred to specialized units. In other words, departing from the current model in which most patients are managed in sleep units (the base of the pyramid) with very little intervention from primary care (the apex), we should work to involve primary care physician and nursing in the management of most of these patients (becoming the base of the pyramid) and referring only to those patients of greater complexity to the units more specialized (vertex).9
Regarding the diagnosis, primary care physicians should be able to correctly establish a clinical suspicion of OSA and to identify the risk groups, giving priority referral to patients with high-risk jobs, debilitating sleepiness or respiratory failure. Once a proper screening and assessment for OSA is accomplished by primary care physicians, practitioners should be able to perform highly simplified methods in those relatively simple cases of patients with a high pretest probability for OSA, which would shorten wait lists for sleep units, improve patient access to sleep services, and enable the initiation of treatment sooner in those patients who need it most. Some publications have already shown that this strategy for OSA based in primary care is not clinically inferior to standard care in a specialist sleep center and is cost effective.6,10,11
The SSN has also assessed the topic of therapeutic decisions and follow-up of the patients. Masa et al. determined the diagnostic cost effectiveness of automatic scoring compared with manual scoring and with polysomnography, showing that automatic scoring was a significantly lower-cost alternative for the diagnosis of patients with suspected OSA.12 This group also suggested that auto-adjusted titration at home can replace standard titration with polysomnography.13 Both findings simplify the therapeutic decisions on OSA in primary care and make them easier to implement, saving money and reducing waiting lists. With respect to follow-up, Sánchez-de-la-Torre et al. showed that the assessment of continuous positive airway pressure (CPAP) compliance by primary care physicians was as effective as conventional CPAP management in a sleep unit, rendering treatment more cost effective.7 Finally, the GESAP trial14 demonstrated that the diagnosis and management of OSA conducted by primary care personnel is a cost-effective alternative to management in specialized sleep units.15 However, it is true that the application of this type of protocol in clinical practice, as has occurred with other diseases, is not always easy or possible.
The important role of specialized technicians in sleep medicine is also noteworthy. To achieve excellence in these procedures, it is not sufficient to receive adequate training in sleep medicine; rather, it should be necessary to achieve a technician accreditation. The SSN is working on this topic, and first Spanish technicians were accredited in sleep medicine recently. Finally, the role of sleep therapy equipment suppliers should not be forgotten. They must be required to meet care standards that should be evaluated by sleep units and both, providers and sleep units, must work closely together.
In conclusion, a change from the current care model system to an integrated network model is needed. The involvement of primary care providers specifically trained in screening, therapeutic decisions and follow-up would enable more cost-effective management of SDB. Due to the current evidence demonstrating the cost-effective management of OSA in primary care, the specific objective in the next few years for the SSN is to implement this model in the clinical practices in our country.
Biological impact of OSA on comorbidities with high mortality: cardiovascular disease, neurocognitive disease and cancerSD have been strongly associated with an increased risk for several diseases associated with high mortality and social impacts, such as cardiovascular disease,16 neurocognitive impairment,17 and cancer.18
The presence of OSA leads to pathophysiological mechanisms that include intermittent hypoxia (IH), sleep fragmentation and changes in intrathoracic pressure. These alterations seem to activate inflammation, sympathetic activation, hypercoagulability, endothelial dysfunction, oxidative stress and metabolic alterations; however, little is known regarding the role of each process and its specific implications.
In this context, Almendros et al.19 demonstrated the putative role of IH in tumor biology in murine models, thereby lending biological plausibility to the epidemiological studies that have shown increased cancer incidence and mortality in OSA patients.20 Additionally, the SSN has recently shown that IH induces a hypoxia-induced-factor that compromises the immunosurveillance capacity against tumor cells or other noxious entities.21,22 These alterations suggest a pathogenic pathway that could explain the higher incidence of cancer mortality in these patients. However, in most cases, it has not been possible to identify the specific mechanisms as a pathogenic pathway or to determine whether some pathways act simultaneously, linking the immediate consequences of OSA with its risks.
A better pathophysiological characterization could have diagnostic consequences. OSA is a complex, heterogeneous and multicomponent disorder that is not well defined by the measurements derived only from sleep studies. In fact, these parameters are poor predictors of the associated end-organ morbidity that results from the underlying OSA, and they do not provide useful guidance regarding possible therapeutic options. The identification of a biomarker could imply the possibility of dispensing with classic sleep studies to identify patients with sleep disorders and improve the diagnostic process. An example of the strategy to screen for OSA in pediatric patients is the use of proteomics in urine samples. Gozal et al.23 showed that the levels of a group of proteins were higher in OSA patients than in the controls, facilitating the identification of patients. If these biomarkers had the ability to identify patients at risk for a specific consequence, the disease could be prevented by initiating a specific treatment.
Numerous randomized clinical trials (RCTs) have evaluated the impact of OSA and its treatment with CPAP, a significant number of which focused on cardiovascular outcomes. Nevertheless, this impact has been poorly explored in other diseases, such as cancer and neurodegenerative disease. Interestingly, the attempt to demonstrate the relationship between OSA and cardiovascular consequences or the effectiveness of its treatment has resulted in contradictory conclusions. Some of the studies of risk reduction revealed no or even a deleterious effect of treating OSA.24,25 These types of results have created discrepancies between the existing evidence from basic/epidemiological studies and RCTs. There are several possible explanations for the discrepancies. The first could be that previous studies overestimated the impact of the findings on the actual risk of SD in patients. Second, it could be that the damage produced was structural and, therefore, irreversible. Moreover, heterogeneity within the forms of OSA could affect the predisposition to suffer complications or the specific positive response to the treatment. Finally, many of these RCTs identify composite outcomes. There should also be an awareness of the fact that, in general, the events that compose the “composite outcomes” do not have all the same “value”. Further studies are needed to identify OSA treatment in specific patient phenotypes and on specific outcomes.
In conclusion, a deeper understanding of the pathophysiological mechanisms that are associated with the risk of SD is needed in the field of sleep medicine, as they have consequences with respect to patient management. In particular, the predictive patterns of biomarkers could optimize the management of the disease and precisely identify each patient to address the type and need of treatment, which would have important economic implications.
Big data analysis for the identification of OSA phenotypesEfficient tools should be used to characterize the population to predict patients at high risk of suffering from the consequences of OSA. One of the current tools is the analysis of large data sets through a big data methodological approach. This type of analysis has had a significant impact on the medical field. It permits accurate modeling of complex diseases and offers new opportunities for innovative clinical applications to subsequently benefit the patient. The increasing availability of clinical databases for large-scale analysis and the access to biobanks offer a new possibility to develop new strategies for disease prediction, prevention and treatment.
Cluster analysis in large OSA databases has been used to characterize its heterogeneity and identify existing phenotypes.26•28 Several clinical phenotypes have been identified, although there is a lack of association between these categorizations and significant clinical results, while others require clinical validation.29 As an example, in the European Sleep Apnea Database (ESADA) of 6555 patients with OSA, various clinical phenotypes, such as excessive daytime sleepiness (EDS) and insomnia, and their relationship with comorbidities were analyzed.30 It was found that cardiovascular disease was less prevalent in the group with EDS and more common in the insomnia phenotype, although the group with EDS had more severe OSA.
Recently, an analysis of the largest database obtained to date has been published. The analysis included a cohort of 1,704,905 patients with OSA in US population between 30 and 94 years old.31 The main objective was to assess the different comorbidities associated with OSA, gender differences and the potential effect of age. The diagnosis of OSA was independently associated with a greater number of comorbidities. The prevalence of cardiovascular disease increased with age, especially between 60 and 70 years. Type 2 diabetes and ischemic heart disease were more prevalent in men, whereas high blood pressure and depression were more prevalent in women, with the latter being more frequent at younger ages. The gender differences between the prevalence of heart failure, arrhythmias and stroke were less pronounced. This better characterization of the OSA phenotype in women opens the door to developing new lines of research.
A recent publication32 used cluster analysis to characterize the population of CPAP-treated subjects in Catalonia. Six clusters were identified, but the majority of patients could be divided into two large groups: older patients with high mortality and increased use of healthcare services and those patients with fewer comorbidities, low mortality and less use of healthcare services. These results highlight the heterogeneity of patients treated with CPAP and emphasize the importance of identifying the indications and expected benefits of CPAP for specific OSA phenotypes. This further suggests that there is an opportunity to adapt interventions to different groups.33 The authors also described that CPAP treatment is associated with reductions in mortality at the population level, although only in men.
Actually, there are two specific tools currently being promoted by the SSN and offered to the scientific community. The BIOSAOS project is a clinical database common to all Spanish sleep units that is associated with biological samples. The aim of this project is to explore new biomarkers in OSA, to perform prospective studies with optimized experimental designs and methodological procedures and to facilitate the transfer of knowledge and collaboration among researchers. The SSN has developed a general population database, the Vitoria Sleep Cohort, a group that includes 2000 patients between 30 and 70 years old with 20 years of follow-up. These two databases will provide the opportunity to perform specific actions at the population level. The analysis of large databases can provide useful real-life information and/or assist in the design of future studies.
Personalized medicine in OSAAs mentioned, OSA requires personalized medicine to classify the different phenotypes of the disease to prescribe precise and adequate treatment that is targeted to the needs of individual patients on the basis of their genetic, biomarker, phenotypic, or psychosocial characteristics. Efforts to perform unbiased clustering have suggested that additional parameters in the classification approaches may be of value in more clearly defining the subjects.
The gold standard for OSA diagnosis is in-laboratory polysomnography, but portable monitoring devices, with less complex and faster home diagnosis, have been developed in the past.34 Furthermore, innovative methods have validated the utility of craniofacial digital photography for the diagnosis of OSA.35,36 This approach should therefore enable improvements in OSA risk stratification according to craniofacial morphological phenotypes. Nevertheless, innovative thinking is necessary to develop new, easy, affordable and inexpensive diagnostic methods.
Moreover, it is important to consider the heterogeneous response to CPAP. The usefulness of CPAP treatment in reducing blood pressure in patients with resistant hypertension has been demonstrated, but responses are highly variable. In fact, 25•30% of patients who use CPAP treatment for >4h/night do not experience a positive effect.37,38 A singular circulating microRNA that predicts blood pressure responses to CPAP in patients with resistant hypertension and OSA has been reported (HIPARCO score), which identifies patients with a favorable blood pressure response.39 This biomarker enables the identification of patients who will have a positive response to treatment to facilitate the customization of treatment.
The absence of these factors, as well as low adherence, may contribute to the occurrence of undesirable deleterious effects. Thus, it becomes a priority to predict the possible response to treatment in each patient cluster and adapt the treatment modality in a personalized manner. Moreover, new scenarios and algorithms of treatment modalities that combine the various available treatment options are needed.40 Precision medicine is defined as the targeted prevention or treatment of individual patient needs, as determined by their genetic characteristics, biomarker profiles, and phenotypic or psychosocial characteristics, each of which confers a unique phenotype to each patient. Thus, we must consider the possibility of applying personalized preventive measures to OSA patients who have a recognized high-risk profile, with the knowledge that such targeted interventions will prevent the occurrence of comorbidities.
Finally, the importance of good adherence to CPAP treatment is as critical as the adequate selection of the treatment. The participatory aspects of a new treatment41 take the patient from being a passive recipient of care to assuming the active management of their own wellness. Access to health applications and the web through connected mobile devices plays a central role in health care, particularly in the context of mobile applications (apps). Recently, the application of participatory care using a web-based technology to enhance CPAP adherence has been demonstrated.42 The use of telemedicine in healthcare is clearly advancing, and the rapid technological advances will probably deeply change the organization of health care systems to involve not only all levels of medical personnel but also engineers and other nonphysician professionals.
OSA in children: current needs and future perspectivesThe relevance of OSA in childhood is linked to two fundamental aspects: its prevalence and its important health consequences.43•45 The prevalence of OSA in children ranges from 0.2 to 4.1%43•45 and 21.5 to 46.6%46 in obese children. The pathogenesis of childhood OSA is multifactorial.43•45 Adenotonsillar hypertrophy is the most frequent cause,43•45 but craniofacial alterations, functional factors, abnormal neurological control and obesity are also implicated. The NANOS-Study46 showed that adenotonsillar hypertrophy and obesity are independent risk factors for childhood OSA. Furthermore, it is necessary to consider the possible involvement of genetic factors,43•45 and new techniques of genetic mapping could help to identify the genes involved in childhood OSA. Children are the best and most natural model for carrying out genetic studies.
The diagnosis of OSA in children requires performing nocturnal polysomnography,43•45 but portable systems have been validated in the hospital and at home.43,44,47 Specific urine proteins have been identified48; furthermore, the use of neural networks in the analysis of oxygen saturation has demonstrated good sensitivity and specificity.49•51
The relevance of OSA in children is determined by the association with delayed growth, enuresis, and cardiovascular, metabolic and neurocognitive morbidity.43•45 Regarding cardiometabolic morbidity, pulmonary hypertension is one of the first complications described in children with severe OSA. OSA in children is associated with increased systemic blood pressure and insulin resistance, especially when obesity is present.43•45 However, studies that have evaluated the effect of OSA treatment on metabolic parameters have reported contradictory results. The only RCT on adenotonsillectomy for childhood sleep apnea revealed no improvement in circulating lipoproteins after adenotonsillectomy,52 but recent studies have shown improvements in lipid profiles in obese and nonobese children.53
With regard to neurocognitive disorders, behavioral disorders, inattention, hyperactivity and academic difficulties are more frequent in children with OSA.43•45 However, the CHAT study did not show significant improvements in executive function with treatment; therefore, some of the negative consequences of OSA may be only partially reversible, emphasizing the need for early diagnosis and treatment.
Not all children with OSA develop morbidity, which supports the theory that a specific susceptibility influenced by environmental factors determines a phenotypic expression. The use of organ damage biomarkers54•56 would allow individualized treatment and serve as a control for assessing response to treatment. The possibility of residual OSA after adenotonsillectomy is not negligible, and dietary, medical, orthodontic or CPAP treatment may be necessary.43•45 Among the factors related to the persistence of OSA, obesity is a clear risk factor for a poorer response to adenotonsillectomy.52,56 The search to identify risk phenotypes and residual OSA will allow us to predict the response to treatment and identify at-risk populations to facilitate optimal, stepped and individualized treatment.
In summary, OSA in children is a major health problem; without an adequate diagnosis and treatment, it is associated with important consequences. In the future, the identification of phenotypes will allow us to individualize treatment. It is necessary to develop new diagnostic techniques and improve the knowledge of morbidity biomarkers, which will require large longitudinal studies of cohorts to define the natural history of OSA.
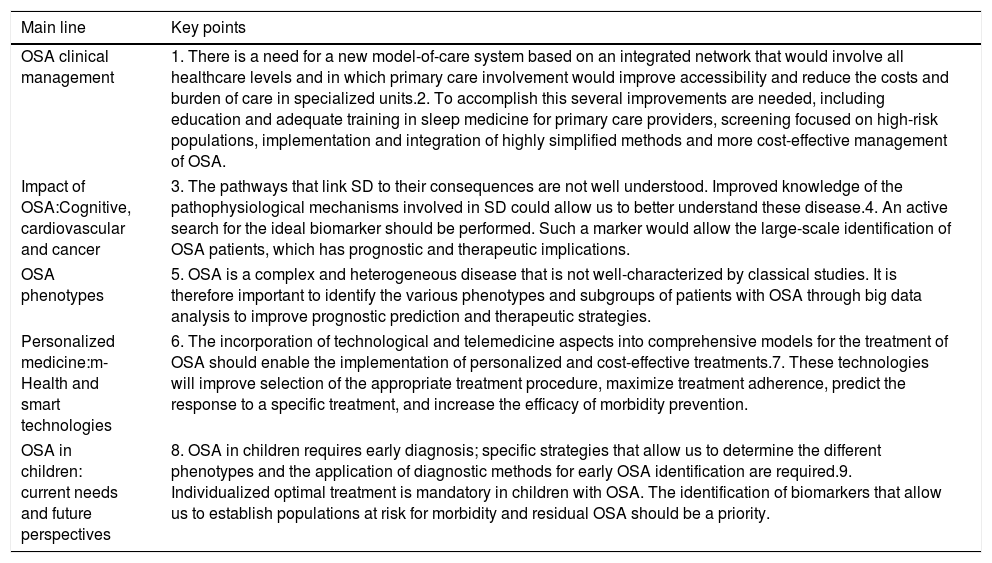
ConclusionsThe main conclusions of these five lines of study are summarized as Key points in Table 1.
Spanish Sleep Network (SSN) 1st World Cafèc) Key points.
| Main line | Key points |
|---|---|
| OSA clinical management | 1. There is a need for a new model-of-care system based on an integrated network that would involve all healthcare levels and in which primary care involvement would improve accessibility and reduce the costs and burden of care in specialized units.2. To accomplish this several improvements are needed, including education and adequate training in sleep medicine for primary care providers, screening focused on high-risk populations, implementation and integration of highly simplified methods and more cost-effective management of OSA. |
| Impact of OSA:Cognitive, cardiovascular and cancer | 3. The pathways that link SD to their consequences are not well understood. Improved knowledge of the pathophysiological mechanisms involved in SD could allow us to better understand these disease.4. An active search for the ideal biomarker should be performed. Such a marker would allow the large-scale identification of OSA patients, which has prognostic and therapeutic implications. |
| OSA phenotypes | 5. OSA is a complex and heterogeneous disease that is not well-characterized by classical studies. It is therefore important to identify the various phenotypes and subgroups of patients with OSA through big data analysis to improve prognostic prediction and therapeutic strategies. |
| Personalized medicine:m-Health and smart technologies | 6. The incorporation of technological and telemedicine aspects into comprehensive models for the treatment of OSA should enable the implementation of personalized and cost-effective treatments.7. These technologies will improve selection of the appropriate treatment procedure, maximize treatment adherence, predict the response to a specific treatment, and increase the efficacy of morbidity prevention. |
| OSA in children: current needs and future perspectives | 8. OSA in children requires early diagnosis; specific strategies that allow us to determine the different phenotypes and the application of diagnostic methods for early OSA identification are required.9. Individualized optimal treatment is mandatory in children with OSA. The identification of biomarkers that allow us to establish populations at risk for morbidity and residual OSA should be a priority. |
Olga Mediano, Irene Cano-Pumarega, Manuel Sánchez-de-la-Torre, María Luz Alonso-Álvarez, María Fernanda Troncoso, Francisco García-Río, Carlos Egea, Joaquín Durán Cantolla, Joaquín Terán-Santos, Juan Fernando Masa, Josep María Montserrat: none declared.
Ferran Barbèc): received a research grant from ResMed Foundation USA, Philips USA, the Health Research Fund, Spanish Ministry of Health, the Spanish Respiratory Society (SEPAR) and Oxigen Salud Spain.
To the Sociedad Española de Neumología y Cirugía Torácica (SEPAR), the Sociedad Española de Sueño (SES), the Centro de Investigaciones Biomèc)dicas en Red (CIBER) and the Spanish Sleep Network (SSN) members, especially those who participated in the 1st World Cafèc) meeting (Guadalajara, Spain). This work is especially dedicated to our dear friend Joaquin Teran, one of the fathers and architects of the SSN who gave us a life of friendship, affection, enthusiasm and exemplary professionalism.
Joaquín Durán-Cantolla (Centro de Investigación Biomèc)dica en Red de Enfermedades Respiratorias (CIBERES), Madrid, Spain; Instituto de Investigación Bioaraba, OSI Araba Hospital Universitario, Vitoria, Spain. Facultad de Medicina, Departamento de Medicina, Universidad del País Vasco, UPV/EHU, País Vasco, Spain). Joaquín Terán-Santos (Centro de Investigación Biomèc)dica en Red de Enfermedades Respiratorias (CIBERES), Madrid, Spain; Sleep Unit, Pneumology Department, Hospital Universitario de Burgos, Burgos, Castilla-León, Spain). Ferran Barbèc) (Centro de Investigación Biomèc)dica en Red de Enfermedades Respiratorias (CIBERES), Madrid, Spain; Group of Translational Research in Respiratory Medicine, Hospital Universitari Arnau de Vilanova y Santa Maria, IRB Lleida, Lleida, Spain). Juan Fernando Masa (Centro de Investigación Biomèc)dica en Red de Enfermedades Respiratorias (CIBERES), Madrid, Spain; Pneumology Department, Hospital San Pedro de Alcántara, Cáceres, Spain). Josep María Montserrat (Centro de Investigación Biomèc)dica en Red de Enfermedades Respiratorias (CIBERES), Madrid, Spain; Pneumology Department, Hospital Universitario Clinic-IDIBAPS, Barcelona, Spain).