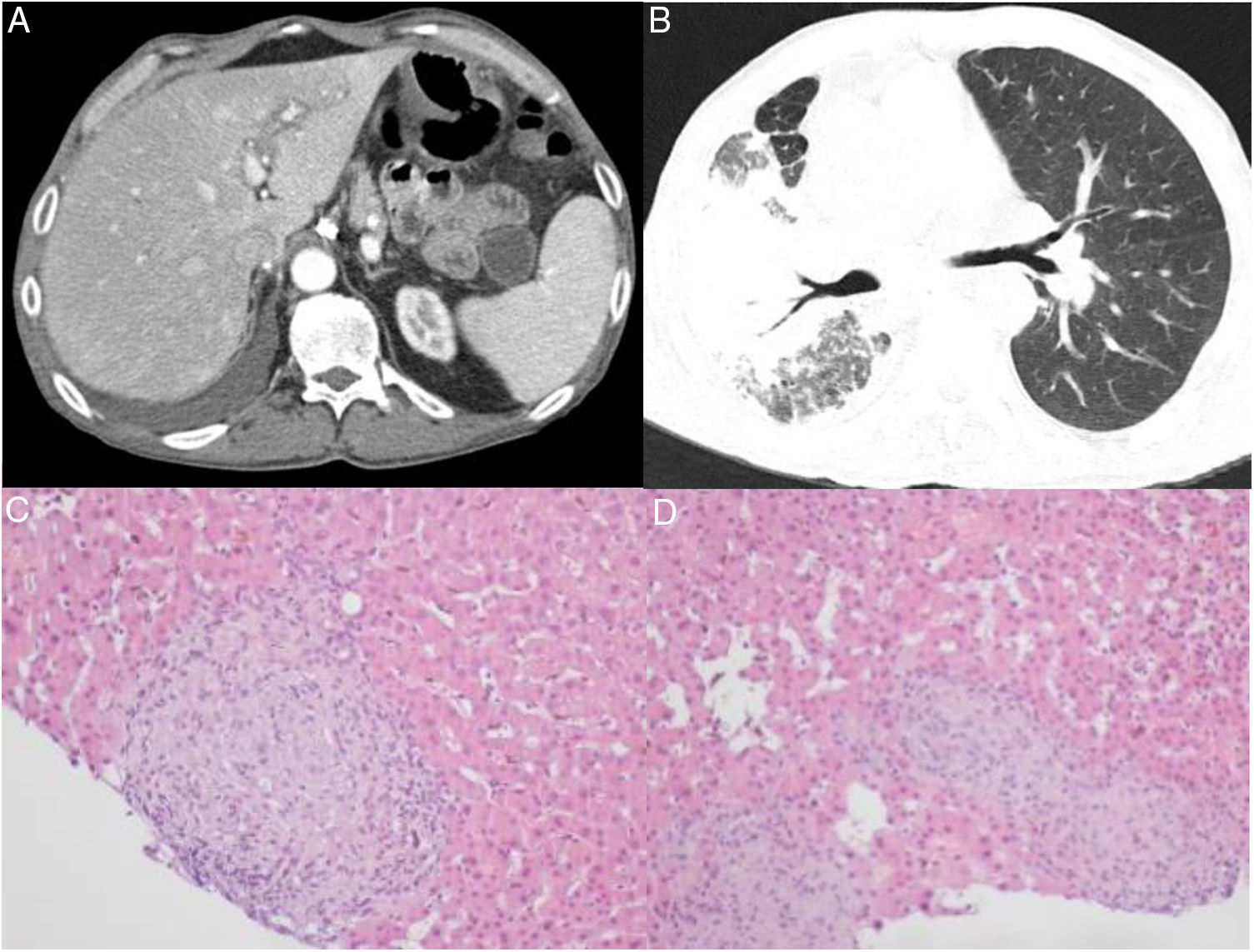
The authors report the case of a 55-year-old man with a left unipulmonary transplant due to pseudotumoral silicosis. He was immunosuppressed with tacrolimus and everolimus. Five years after transplantation, he developed asthenia, abdominal pain, diarrhea and lost more than 10% of his body weight. Blood tests showed iron deficiency anemia and elevated alkaline phosphatase and gamma-glutamyl transferase levels, but no other relevant findings. A computerized tomography scan was performed (Fig. 1A/B), which showed ileal inflammation and heterogeneous, nodular hepato-splenomegaly. Liver biopsy (Fig. 1C/D) revealed diffuse hepatic involvement by a granulomatous inflammatory process. A stool sample was sent for culture, which let to the growth of Mycobacterium avium. Disseminated infection (hepatic and intestinal) by M. avium was then assumed. Chest imaging showed no changes suggestive of pulmonary mycobacteriosis in the transplanted lung and mycobacterial analysis of bronchoalveolar lavage was negative. The patient was started on rifabutin, azithromycin and ethambutol and immunosuppressive therapy was adjusted. After 6 months of therapy, the coprocultures were negative and the patient was showing significant clinical and radiological improvement.
(A) Abdominal CT: heterogeneous and nodular hepato-splenomegaly. (B) Chest CT-transplanted lung: normal appearance. Right lung: signs of pseudotumoral silicosis with massive fibrosis and confluence of silicotic aggregates; both CT scans show a small right-sided pleural effusion that was already present before the transplantation and remains stable since then. This diagnosis is based on the history of substantial exposure to silica dust during 30 years, compatible radiological features, consistent BAL findings and exclusion of other competing diagnoses. (C) and (D) Liver biopsy: epithelioid granulomas.
Extrapulmonary nontuberculous mycobacteriosis (NTM) in lung transplant recipients is rare.1,2 However, its incidence is increasing, probably reflecting improvement in microbiological techniques and longer survival of these patients.1 Establishing the diagnosis of NTM infection can be quite difficult and a high index of suspicion is usually required.2