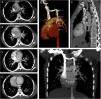
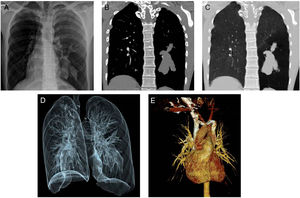
A 20-year-old female patient presented to our radiology department complaining of shortness of breath. Chest X-ray evaluation revealed tubular opacities in the lower zone of the left lung (Fig. 1A). Contrast-enhanced computed tomography (CT) showed non-enhanced tubular lesions compatible with mucocele in the superior and posterior segments of the left lower lobe (Fig. 1B). There was also air trapping in the lower lobe of the left lung (Fig. 1C and D). Three dimensional (3D) CT image demonstrated a persistent left superior vena cava in the left side of the mediastinum (Fig. 1E). The left superior vena cava was draining into the coronary sinus. It hadn’t any association with left pulmonary veins (Fig. 2A–G).
(A) Chest X-ray reveals tubular opacities in the lower zone of the left lung. (B) Contrast-enhanced CT shows non-enhanced tubular lesions compatible with mucocele in the superior and posterior segments of the left lower lobe. (C and D) There is also air trapping in the lower lobe of the left lung. (E) 3D CT image demonstrates a persistent left superior vena cava in the left side of the mediastinum.
Contrast-enhanced axial consecutive CT scans (A–D) reveal a left superior vena cava (dashed arrows) drained into the coronary sinus (arrow head). There is no association with the left pulmonary veins of the left superior vena cava. 3D volume rendered (E) and sagittal (F) and coronal (G) MIP CT images demonstrate clearly the left superior vena cava (dashed arrows) drained into the coronary sinus (arrow heads).
Bronchial atresia is a congenital malformation that may affect lobar, segmental-sub segmental bronchi. Interruption of focal bronchial segments causes air trapping of adjacent lung segment and occurs mucoceles in the obstructed bronchi. The atretic bronchi are characterized by a tubular or nodular opacity in X-ray. The plain radiography shows also hyperinflation in adjacent lung segment. CT scans different obstructed bronchial segments with mucus plugs than pulmonary vascular structures.1 Thus, CT imaging helps precise diagnosis.