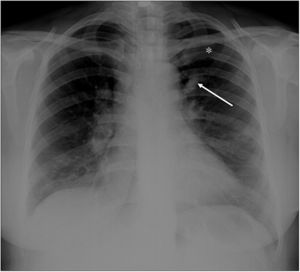
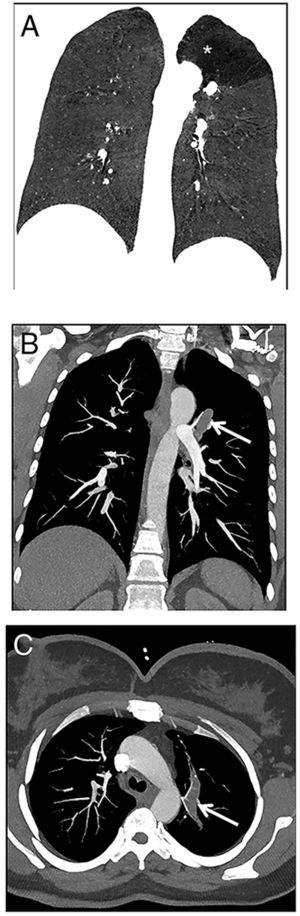
A 22-year-old woman was referred to our emergency radiology unit with sudden onset of shortness of breath and left-sided chest pain. The chest radiography revealed left hilar tubular opacite (arrow) and hyperaeration (asterisk) in the upper zone of the left lung (Fig. 1). The contrast enhanced computed tomography (CT) showed a non-contrast enhancing tubular mass that was seen extending from the left hilum, with surrounding hypoattenuation of the apicoposterior segment of the left upper lobe (asterisk), a finding indicative of hyperinflation (Fig. 2A). There was also no connection between the non-contrast tubular mass (arrows) and pulmonary artery of the apicoposterior segment in the left upper lobe (Fig. 2B–C). CT findings were also including mucocele and occlusion of the bronchus central to the mucocele. CT results (mucocele with hyperaeration of the adjacent lung parenchyma) were considered pathognomonic for bronchial atresia. Surgical treatment was no performed because the patient refused operation.
The reformat coronal CT at maximum inspiration (A) shows a non-contrast enhancing tubular lesion with surrounding hypoattenuation of the apicoposterior segment of the left upper lobe (asterisk), a finding indicative of hyperinflation. The coronal CT scan also demonstrates aerial trapping in the apicoposterior segment of the left upper lobe. The contrast enhanced maximum intensity projection images (B and C) reveal no connection between the non-contrast tubular lesion (arrows) and pulmonary artery of the apicoposterior segment in the left upper lobe.
The bronchial atresia is a congenital abnormality resulting from focal interruption of a lobar, segmental, or sub segmental bronchus with associated peripheral mucus impaction and associated hyperinflation of the obstructed lung segment. In bronchial atresia, cause of hyperinflation of the adjacent lung is collateral air drift. Unlike congenital lobar overinflation, there is no ball-valve effect in this condition. Hence, the lobar or segmental hyperinflation is mild.1
Radiologically, bronchial atresia is associated with a triad of findings: focal interruption of a bronchus; associated distal mucus impaction (bronchocele) that is visible as a branching tubular or ovoid area of increased attenuation; and associated hyperinflation of the obstructed pulmonary segment.2 Bronchial atresia should be kept in mind in patients with shortness of breath and chest pain.