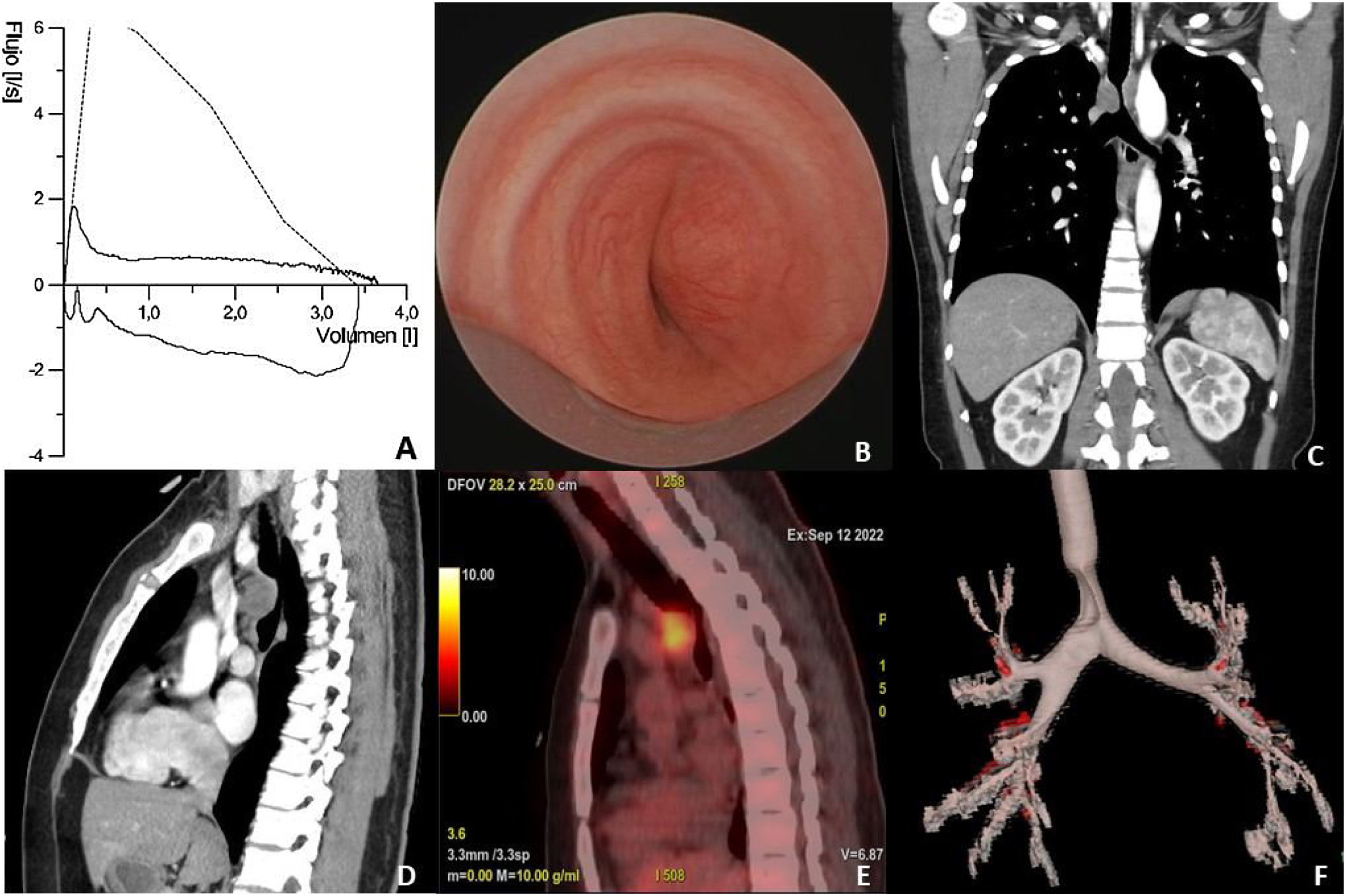
28-Year-old woman originally from Peru. History of pneumonia at the age of 2. Seen in the Pulmonology clinic for grade 1 mMRC dyspnea and dry cough with cold foods. Presented to the emergency department with increased dyspnea, non-productive cough, fever, epistaxis, dysphagia, and odynophagia. Physical examination revealed stridor following a SARS-CoV-2 infection in 2020, with no history of intubation. Forced spirometry (Fig. 1A) showed a spirometry curve morphology with inspiratory and expiratory plateaus suggestive of tracheal obstruction. Bronchoscopy (Fig. 1B) revealed distal tracheal stenosis, measuring 2–3cm, with tissue originating from the right lateral wall, occupying 90% of the tracheal lumen and protruding over the entrance of the right main bronchus. IgG 922mg/dL, IgE 71.4mg/dL. Chest CT scan (Fig. 1C, D, and F) showed a lobulated soft tissue mass in the distal third of the tracheal lumen, encroaching and partially obstructing its anterior and right borders, and to a lesser extent, the left side, carina, and right main bronchus. It measures approximately 28mm×15mm×28mm. PET-CT (Fig. 1E) revealed a mediastinal lesion with pathological metabolism (SUVmax 7) warranting histological evaluation. No other local or distant abnormalities were noted.
(A) Morphology of the spirometric curve with inspiratory and expiratory plateau. (B) Distal tracheal stenosis seen in fibrobronchoscopy. (C and D) Chest CT with lobulated soft tissue mass, at the level of the distal third of the tracheal lumen, which conditions partial stenosis. (E) Mediastinal lesion with pathologic metabolism. (F) Chest CT reconstruction showing tracheal stenosis.
Diagnosis via rigid bronchoscopy: Tracheal mucosa biopsy revealed intensely artifacted sclerosing inflammatory lesion with highly suggestive histological characteristics of IgG4-associated disease. Treated with a Y-shaped endobronchial tracheal prosthesis (Dumon type) due to critical tracheal stenosis, along with prednisone at 1mg/kg with gradual tapering, resulting in a reduction in the size of the peritracheal soft tissue lesion. The prosthesis was removed after 5 months.
IgG4-RD is a systemic condition characterized by abundant infiltration of IgG4-positive plasma cells. Approximately 90% of patients exhibit systemic involvement, with isolated organ lesions, nodules, or masses being rare. Laryngotracheal involvement is exceptionally rare, described in only a limited number of cases.
Elevated serum IgG4 concentration is not necessary for diagnosis, as it can also be elevated in other conditions, and roughly 30% of patients with biopsy-confirmed IgG4-RD have normal serum concentrations, highlighting the importance of histopathology.1
Most IgG4-RD patients respond favorably to treatment with glucocorticoids, and the effectiveness of the anti-CD20 monoclonal antibody rituximab has been described in cases of hypopharyngolaryngeal involvement, especially in cases refractory to systemic corticosteroids.2
Subglottic involvement is a rare manifestation of IgG4-RD with rapid progression to critical obstruction, underscoring the importance of recognizing and treating airway stenoses in patients refractory to local treatments.3
Authors’ contributionsAll authors were involved in the conception and design of the work; acquisition, analysis, interpretation of data, drafting the work, revising it critically for important intellectual content.
Conflict of interestsCAS has received fees in the last 3 years for giving lectures, scientific advice, participation in clinical studies, or writing publications for (in alphabetical order): ALK, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Novartis, and Pfizer. CAS declares not receiving ever, directly or indirectly, funding from the tobacco industry or its affiliates. FROA and UCS has no conflict of interests and declare not receiving ever, directly or indirectly, funding from the tobacco industry or its affiliates.