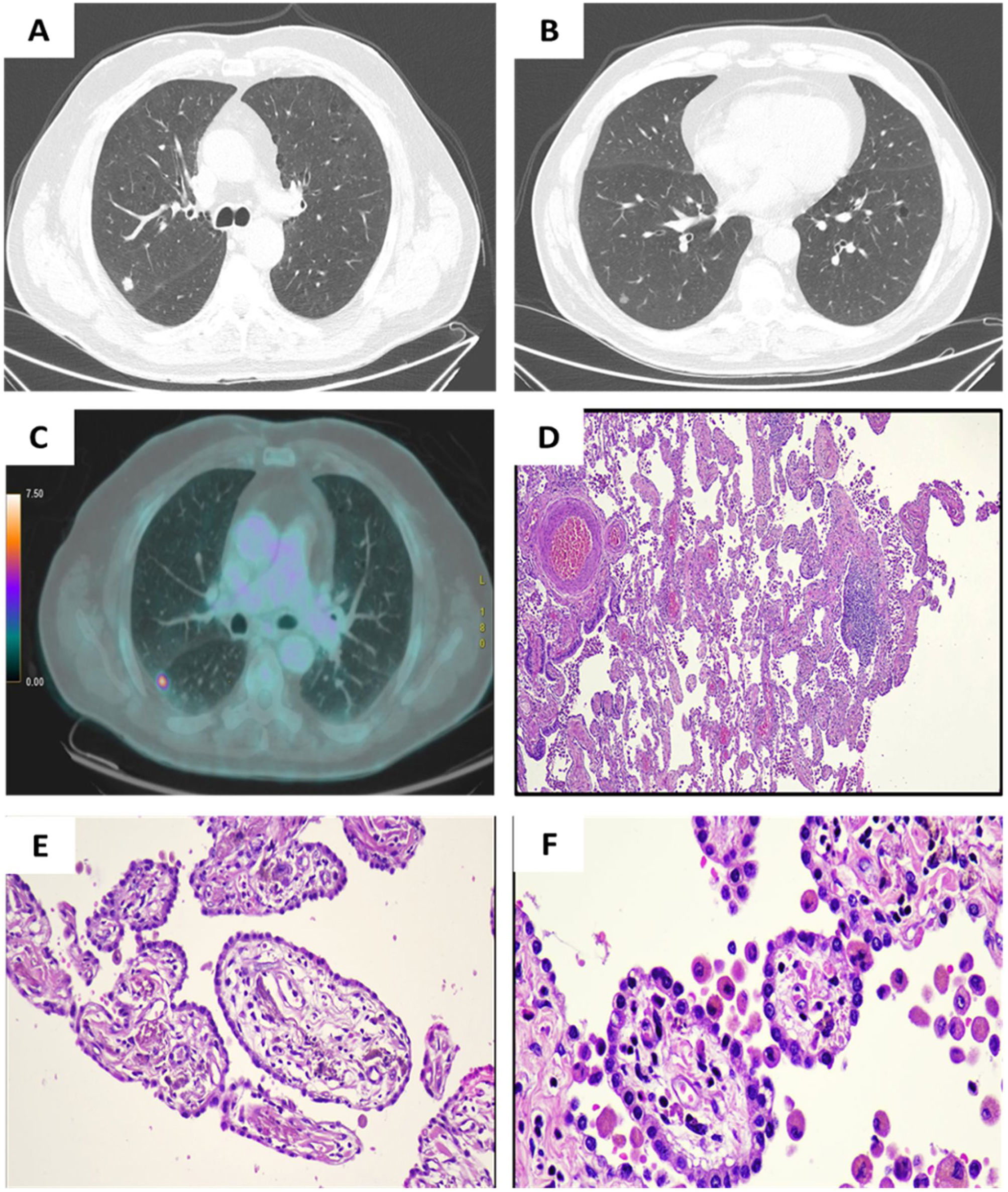
A 62-year-old male, active smoker. He was referred for the study of a pulmonary nodule, found incidentally on chest X-ray, the patient was asymptomatic and had no alterations in laboratory tests. The chest computed tomography (CT) scan showed a nodule in the right upper lobe (RUL) and a second nodule in the middle lobe (ML) (Fig. 1A and B).
(A) 11mm solid nodule in RUL. (B) 7mm subsolid nodule in middle lobe. (C) Hypermetabolic uptake in RUL with a maximum standardized uptake value (SUV) of 10.38. (D) TPL (E) Low-power magnification of placental transfmogrification showing villi-like proliferation destroying normal lung architecture, Hematoxylin-Eosin [ HE] x4. (F and G) Intermediate and high-power magnification showing papillary structures resembling placental villi, lined by cuboidal epithelial cells and containing myxoid-edematous or fibrotic stroma, with a variable number of bland stromal cells, proliferating vessels and inflammatory cells; HEX20.
PET-CT showed pathologic uptake of the RUL nodule, without increased metabolic activity of the other lesion (Fig. 1C). Right upper lobectomy and wedge resection of the ML was performed. The LSD biopsy yielded a large cell carcinoma, and the LM specimen revealed findings compatible with placental transmogrification (Fig. 1E and F).
Placental transmogrification of the lung (PTL) is an infrequent and benign lesion, the name PTL is due to the fact that the alveoli adopt an aspect similar to placental villi, but without fulfilling the functions carried out by the placenta.1
Although its pathophysiology is unknown, one of the possible origins of PTL lies in a probable benign proliferation of interstitial cells with cystic changes secondary to this proliferation.2 Another hypothesis proposes that it is a congenital lesion, but no cases have been reported in pediatric patients. The possibility of a common origin with emphysematous lung lesion, pulmonary lipomatosis or fibrochondromatous hamartoma is also raised.2,3
It is more frequent in men between 20 and 70 years old,2 if the lesion is not large enough to compromise the parenchyma, the patient will remain asymptomatic, which occurs in most cases, otherwise, there will be symptoms such as dyspnea or thoracic pain of acute/subacute or chronic evolution, or even pneumothorax due to rupture of the bulla.3
The radiological presentation is variable, it is generally observed as a bulla, mass, as a thin-walled cystic nodule surrounded by bullous emphysema and, less frequently, as a solitary nodule.3,4 PLT, unlike emphysema associated with spontaneous pneumothorax, occurs in younger age groups, preferentially located in the lower lobes as a single lesion and with a greater tendency for local progression of the disease.4 Horiuchi et al. described a case of PTL masquerading as difficult-to-treat pneumonia.5
Surgical resection is the treatment of choice, being curative in most cases. Currently, the option of a single resection of the affected area is contemplated, thus achieving a minimum loss of healthy pulmonary parenchyma; although lobectomy or pneumonectomy is other options.2–5
Use of artificial intelligence to generate textsThe authors declare that they have not used any type of generative artificial intelligence in the writing of this manuscript or for the creation of figures, graphs, tables or their corresponding captions or legends.
FundingThis research has not received any specific grants from agencies in the public, commercial or for-profit sectors.
Conflict of interestsThe authors state that they have no conflict of interests.


![(A) 11mm solid nodule in RUL. (B) 7mm subsolid nodule in middle lobe. (C) Hypermetabolic uptake in RUL with a maximum standardized uptake value (SUV) of 10.38. (D) TPL (E) Low-power magnification of placental transfmogrification showing villi-like proliferation destroying normal lung architecture, Hematoxylin-Eosin [ HE] x4. (F and G) Intermediate and high-power magnification showing papillary structures resembling placental villi, lined by cuboidal epithelial cells and containing myxoid-edematous or fibrotic stroma, with a variable number of bland stromal cells, proliferating vessels and inflammatory cells; HEX20. (A) 11mm solid nodule in RUL. (B) 7mm subsolid nodule in middle lobe. (C) Hypermetabolic uptake in RUL with a maximum standardized uptake value (SUV) of 10.38. (D) TPL (E) Low-power magnification of placental transfmogrification showing villi-like proliferation destroying normal lung architecture, Hematoxylin-Eosin [ HE] x4. (F and G) Intermediate and high-power magnification showing papillary structures resembling placental villi, lined by cuboidal epithelial cells and containing myxoid-edematous or fibrotic stroma, with a variable number of bland stromal cells, proliferating vessels and inflammatory cells; HEX20.](https://static.elsevier.es/multimedia/03002896/0000006000000001/v3_202406051404/S0300289623003125/v3_202406051404/en/main.assets/thumbnail/gr1.jpeg?xkr=ue/ImdikoIMrsJoerZ+w98FxLWLw1xoW2PaQDYY7RZU=)







