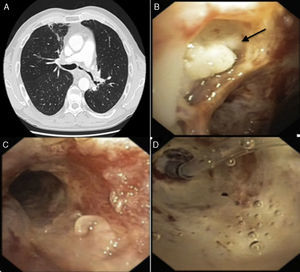
A 71-year-old man with a history of lung adenocarcinoma diagnosed and treated in 2006 with concomitant chemo- and radiotherapy, presented in February 2015 with recurrent respiratory infections. Chest and abdomen computed tomography (Fig. 1A) showed stenosis of the left main bronchus. Flexible bronchoscopy revealed: (a) left lower paratracheal ulcerative lesion covered with mucopurulent secretion (Fig. 1B) and (b) pseudomembranous mucosa in the distal third of the trachea and left main bronchus (Fig. 1C). The left main bronchus was successfully dilated with a balloon catheter (CRE™ Pulmonary; Boston Scientific) (Fig. 1D). Tracheobronchial aspiration was performed in the left main bronchus and endobronchial biopsies were obtained from the ulcerative lesions. The biopsy revealed bifurcated hyphae at 45° angles, with positive Grocott staining, confirming the diagnosis of Aspergillus fumigatus. Culture of the tracheobronchial aspirate was positive for Aspergillus fumigatus.
(A) Loss of volume in the left hemithorax with stenosis of the left main bronchus and bronchiectasis in the apical segment of the right upper lobe. (B) Left lower paratracheal ulcerative lesion covered with mucopurulent secretion (arrow). (C) Pseudomembranous mucosa in the distal third of the trachea and left main bronchus. (D) Balloon catheter dilation of stenosis in left main bronchus.
Treatment was started with liposomal amphotericin B (25mg twice a week) for 2 months (first phase). The patient's respiratory status is currently stable, and endoscopic monitoring and treatment review are pending.
The pseudomembranous form of invasive tracheobronchial aspergillosis is characterized by extensive involvement of the lower airways, with detachment of the necrotic epithelium which, together with the endobronchial mucosa, form the pseudomembranes which cover the mucosa surface.1 Diagnosis should be based on clinical findings, imaging tests, bronchoscopy, pathology examination, and culture and identification of the fungus.2 This variant occurs mainly in immunosuppressed patients, such as lung transplant recipients and patients with HIV, hematological and non-hematological cancers, and COPD patients.3
Please cite this article as: Ariza-Prota M, Morales-Soto A, Rosell-Grataços A. Traqueobronquitis seudomembranosa y ulcerativa causada por Aspergillus fumigatus. Arch Bronconeumol. 2016;52:436–437.